Very proud of our new review @CircAHA on end-organ damage by altered #hemodynamics in #heartfailure.
A true honor to be in the company of 3 legends in the field (Dr. Guazzi, Dr. Testani & Dr. Borlaug). Tweetorial below! https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.119.045409#.X1llBig0WKg.twitter
A true honor to be in the company of 3 legends in the field (Dr. Guazzi, Dr. Testani & Dr. Borlaug). Tweetorial below! https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.119.045409#.X1llBig0WKg.twitter
Key hemodynamic alterations in #heartfailure are:
1. Impaired CO
2. Elevated filling pressures
Normal CO:
REST: 4-8 L/min
EXERCISE: 6 mL/min rise per 1 mL/min rise in VO2
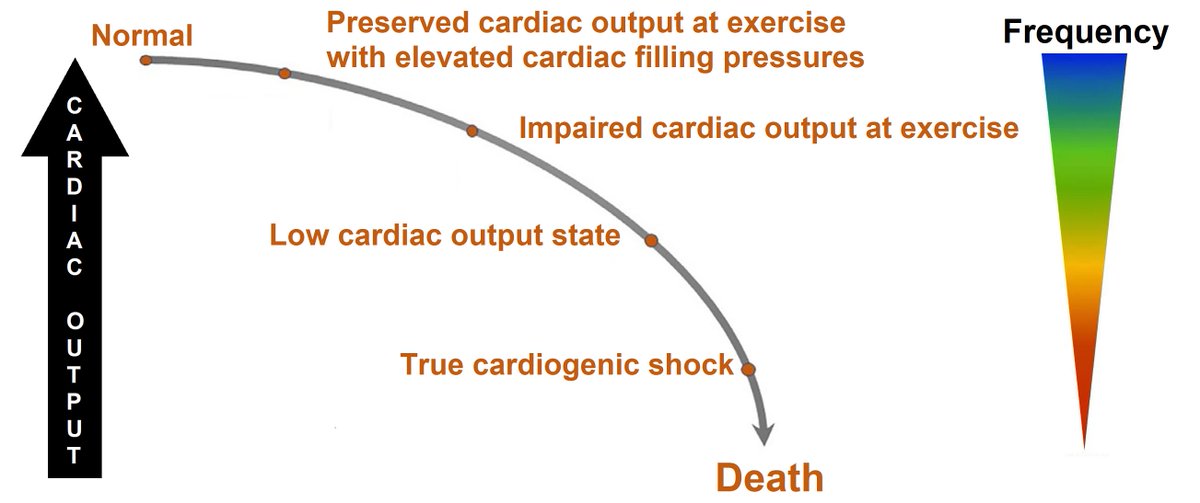
Abnormal CO = continuum (Figure below)
1. Impaired CO
2. Elevated filling pressures
Normal CO:
REST: 4-8 L/min
EXERCISE: 6 mL/min rise per 1 mL/min rise in VO2
Abnormal CO = continuum (Figure below)
Most patients with #heartfailure have normal CO at rest (especially #HFpEF), yet exercise response is abnormal.
Remember, healthy person increases CO with 300-500% during exercise. Heart failure patient only 80% on average (but strongly dependent on severity/type)
Remember, healthy person increases CO with 300-500% during exercise. Heart failure patient only 80% on average (but strongly dependent on severity/type)
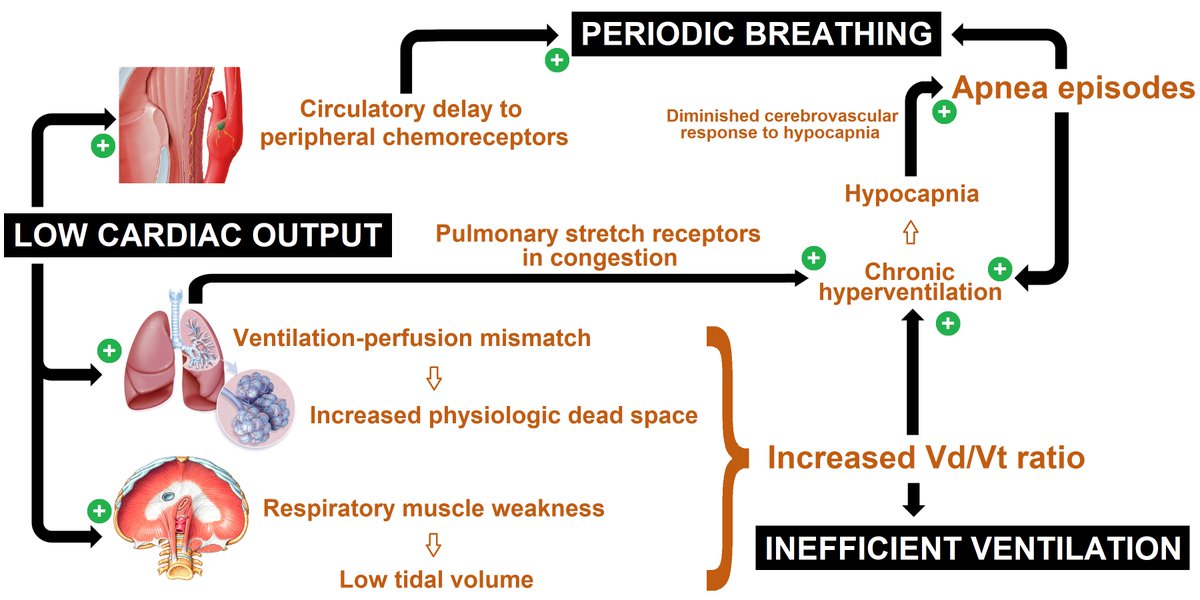
Effect of impaired CO on the lung:
1. Little impact on oxygenation when congestion is absent
2. Marked impact on ventilation: ventilatory inefficiency & periodic breathing
Causes:
- ventilation-perfusion mismatch (death space)
- muscle weakness (diafragm)
- chemoreceptor delay
1. Little impact on oxygenation when congestion is absent
2. Marked impact on ventilation: ventilatory inefficiency & periodic breathing
Causes:
- ventilation-perfusion mismatch (death space)
- muscle weakness (diafragm)
- chemoreceptor delay
Effect of impaired CO on the kidney:
Remember: kidneys are great at autoregulation! This means RBF needs to drop substantially before GFR . Explains how severe low output can have relatively preserved GFR, especially if congestion is absent!
. Explains how severe low output can have relatively preserved GFR, especially if congestion is absent!
CAVE: (prolonged) hypotension!
Remember: kidneys are great at autoregulation! This means RBF needs to drop substantially before GFR
 . Explains how severe low output can have relatively preserved GFR, especially if congestion is absent!
. Explains how severe low output can have relatively preserved GFR, especially if congestion is absent!CAVE: (prolonged) hypotension!
Effect of impaired CO on the kidney (part 2):
- Neurohumoral activation Na avidity
Na avidity
- Low RBF Increased FF (more time for filtration & EA constriction < neurohormones)
Increased FF (more time for filtration & EA constriction < neurohormones) Higher osmolality in peritubular capillaries
Higher osmolality in peritubular capillaries more proximal reabsorption (Starling forces!) #acetazolamide
more proximal reabsorption (Starling forces!) #acetazolamide
- Neurohumoral activation
 Na avidity
Na avidity- Low RBF
 Increased FF (more time for filtration & EA constriction < neurohormones)
Increased FF (more time for filtration & EA constriction < neurohormones) Higher osmolality in peritubular capillaries
Higher osmolality in peritubular capillaries more proximal reabsorption (Starling forces!) #acetazolamide
more proximal reabsorption (Starling forces!) #acetazolamide
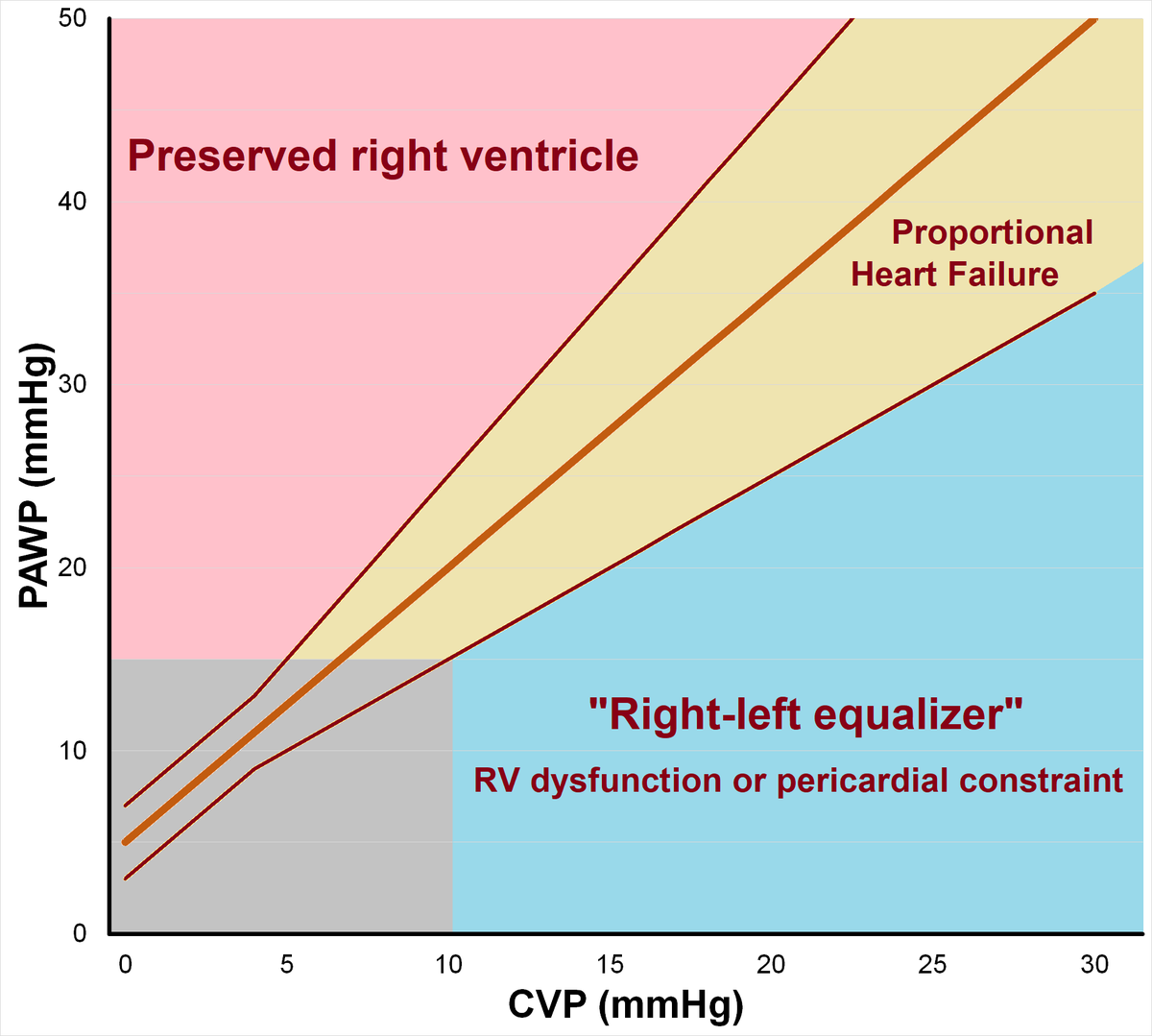
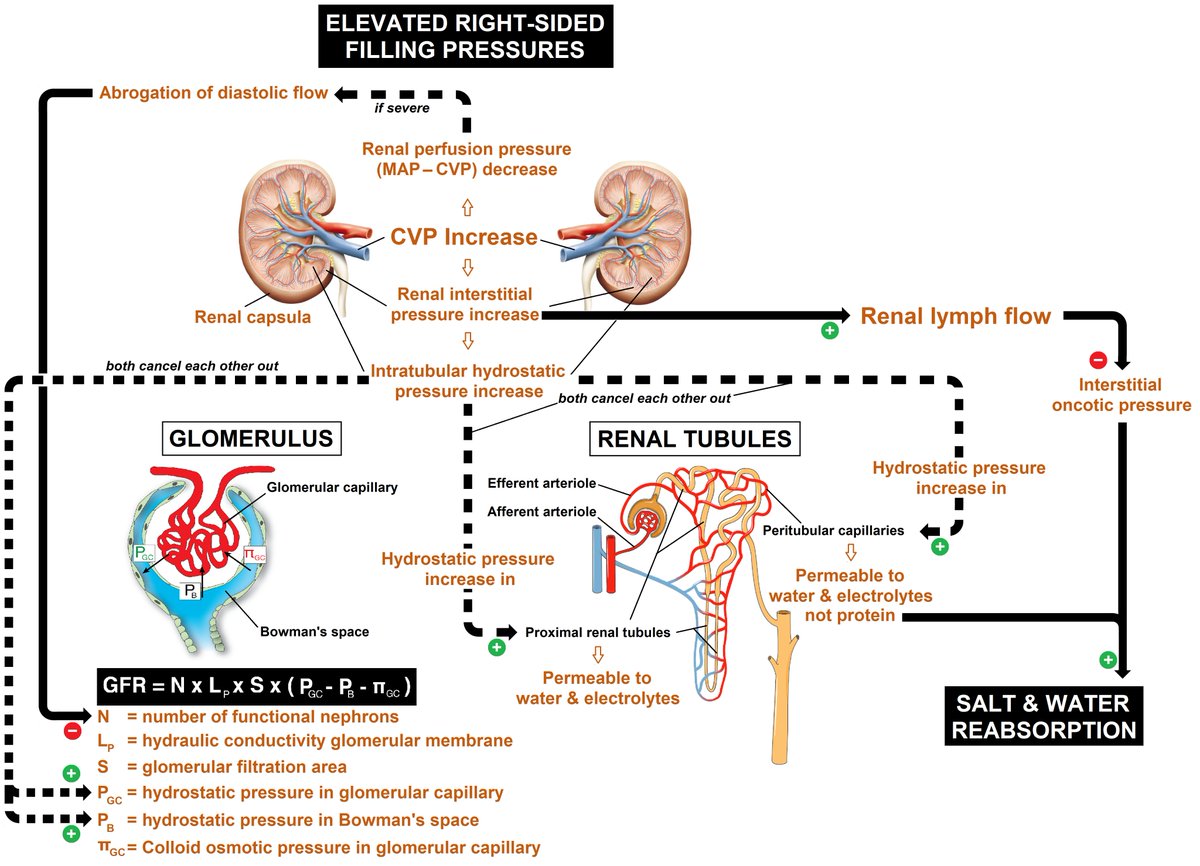
Switching to congestion now:
Normal rest PAWP 5-13 mmHg. Notice 13 is 98th percentile of normal. Therefore, traditional PAWP >15mmHg cut-off for #heartfailure is rather insensitive.
No diagnosis without #exercise!
Normal exercise PAWP
<25 mmHg (supine)
<2 PAWP/CO slope (upright)
Normal rest PAWP 5-13 mmHg. Notice 13 is 98th percentile of normal. Therefore, traditional PAWP >15mmHg cut-off for #heartfailure is rather insensitive.
No diagnosis without #exercise!
Normal exercise PAWP
<25 mmHg (supine)
<2 PAWP/CO slope (upright)
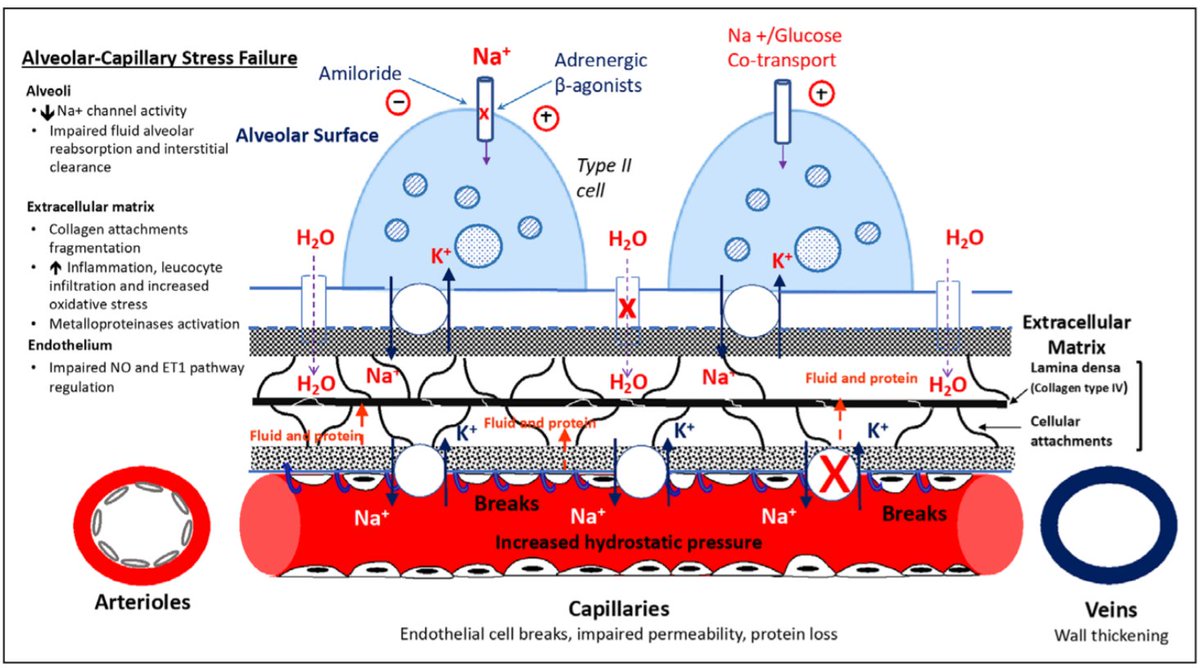
Effect of elevated PAWP on the lung:
PAWP Pcap, Pcap is driving lung edema!
Pcap, Pcap is driving lung edema!
When venous resistance is low, PAWP good approximation. However, for example in #ARDS, elevated venous resistance may cause high Pcap despite low PAWP.
Other examples: sepsis, high-altitude, neurological
PAWP
 Pcap, Pcap is driving lung edema!
Pcap, Pcap is driving lung edema!When venous resistance is low, PAWP good approximation. However, for example in #ARDS, elevated venous resistance may cause high Pcap despite low PAWP.
Other examples: sepsis, high-altitude, neurological
Don't forget that CVP influences lung edema as well, as it impedes lymphatic flow, the main protective mechanism against lung edema. Acute rise more dangerous than slow rise (lymphatic adaptations take time).
Chronic pressure overload: alveolar-capillary stress failure
Chronic pressure overload: alveolar-capillary stress failure
Conclusion: If we treat blood pressure to avoid end-organ damage, we better get the #hemodynamics right in #heartfailure. Especially lung & kidneys will be happy

 Read on Twitter
Read on Twitter