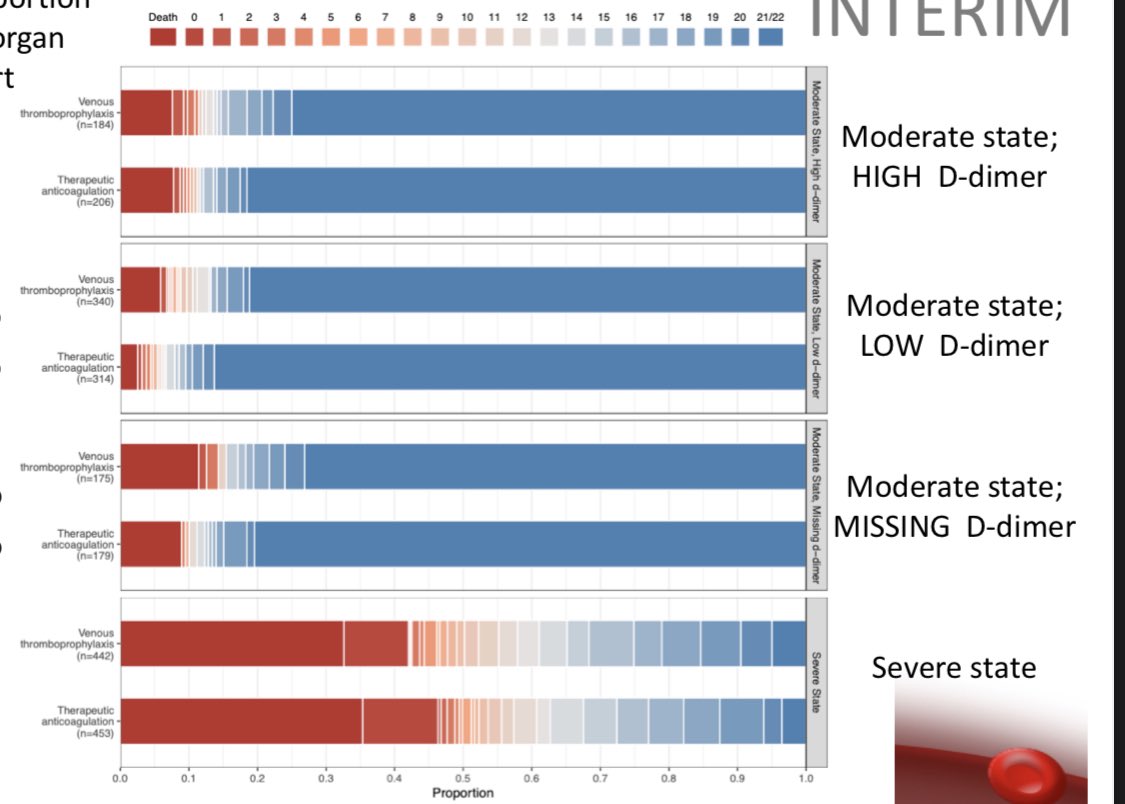
Interesting (unpublished) results from ATACC/ACTIV4/REMAP-CAP #COVID19 studies
Interesting (unpublished) results from ATACC/ACTIV4/REMAP-CAP #COVID19 studies-therapeutic #anticoagulation (TA) reduced organ failure support days in non-ICU patients but had no benefit in ICU patients
-no mortality reduction with TA in either group
1/
https://static1.squarespace.com/static/5f8f2c323fb81b0ae2ce3bca/t/6013140a5a92973b5768764f/1611863053327/mpRCT+interim+presentation.pdf
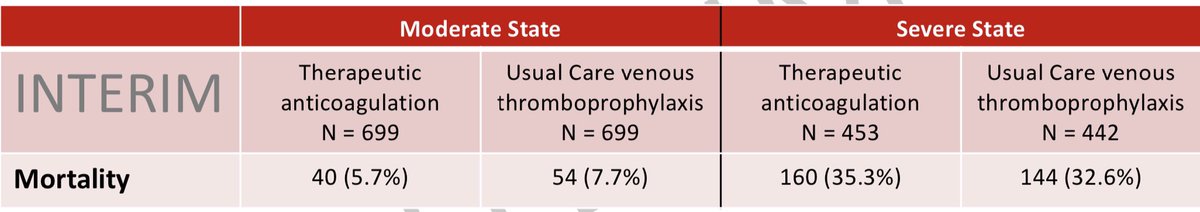
No table 1 info. We can see from the limited data provided that the median age was in the 60s and there were 2:1  :
:  in the ICU cohort.
in the ICU cohort.
Unfortunately we don’t have any information about the patients’ comorbidities or the severity of their illness at presentation.
2/
 :
:  in the ICU cohort.
in the ICU cohort.Unfortunately we don’t have any information about the patients’ comorbidities or the severity of their illness at presentation.
2/
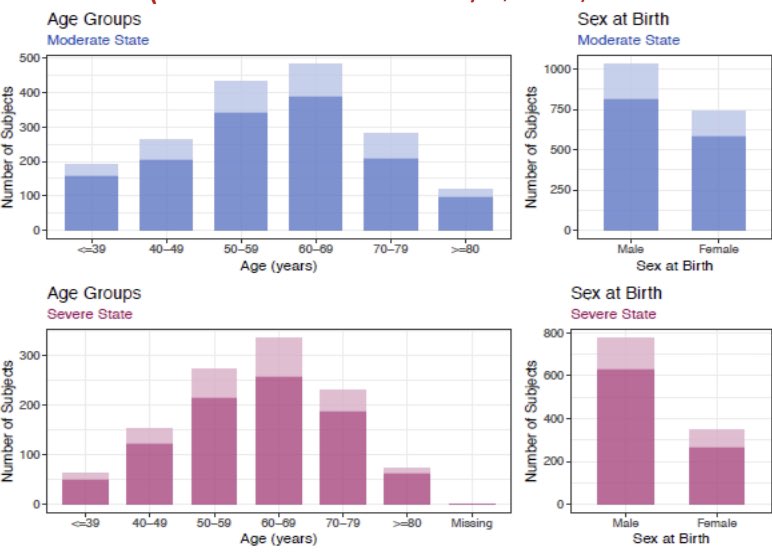
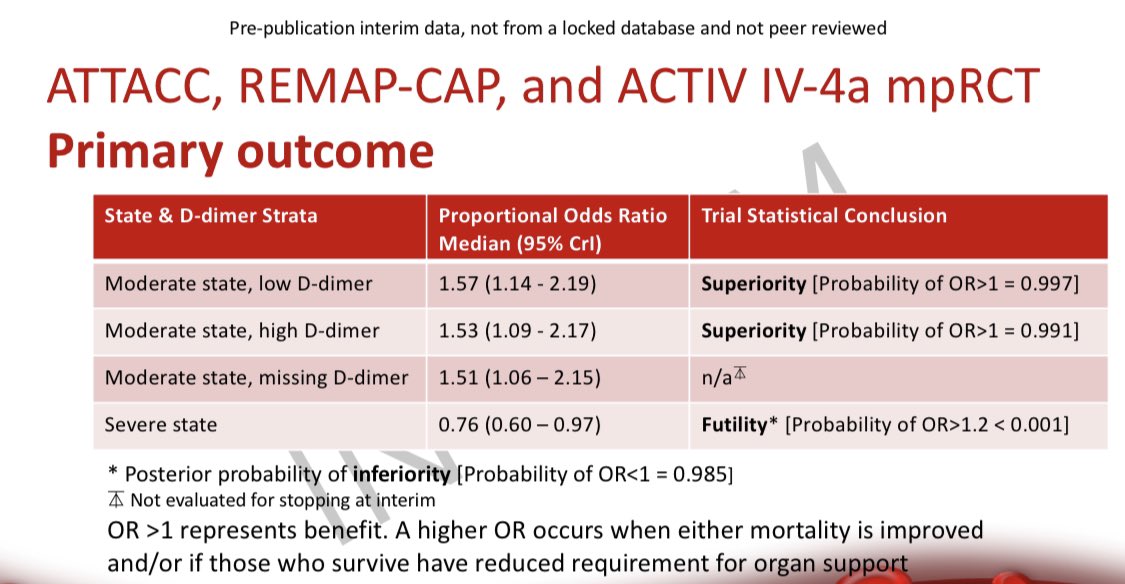
Interestingly, patients with a higher D-dimer weren’t any more likely to benefit from TA.
This is an important observation because many institutions have used high D-dimer as a trigger for intermediate or therapeutic anticoagulation.
3/
This is an important observation because many institutions have used high D-dimer as a trigger for intermediate or therapeutic anticoagulation.
3/
The primary outcome - organ support free days (OSFD) - appears to be significantly INCREASED (good news) in moderate disease with TA, but OSFD is DECREASED (bad news) in severe disease with TA.
No info about rates of MV, NIPPV, RRT, etc. so it’s hard to parse this further.
4/
No info about rates of MV, NIPPV, RRT, etc. so it’s hard to parse this further.
4/
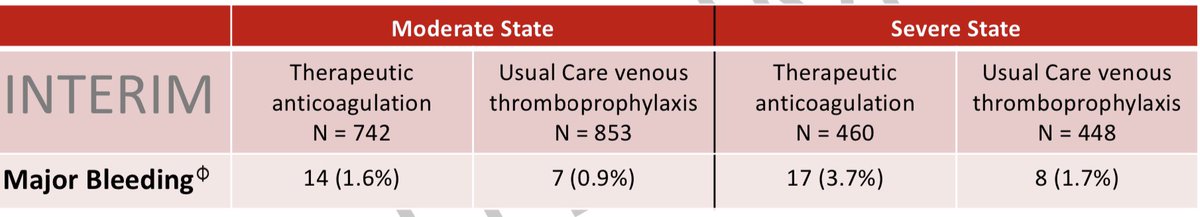
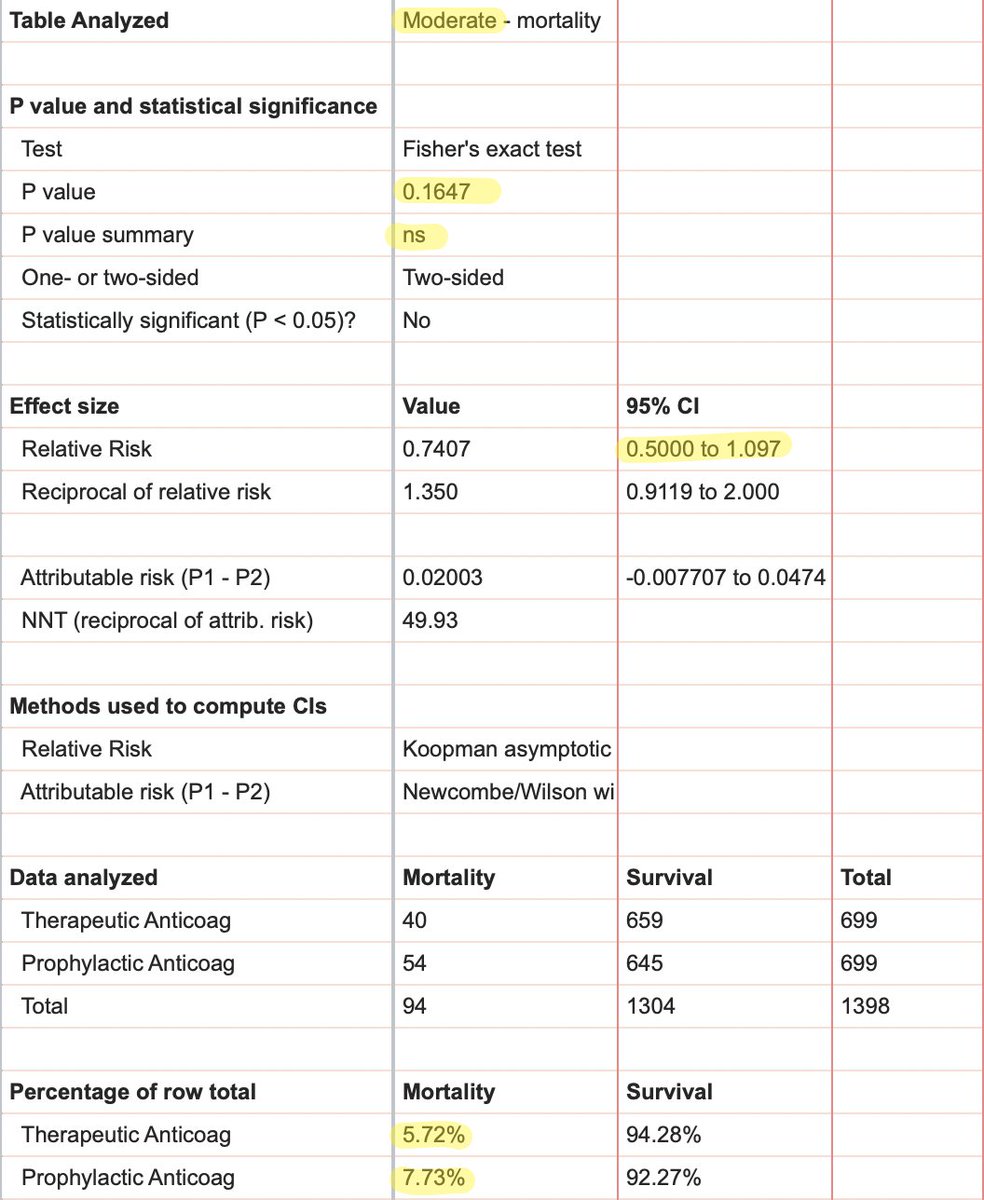
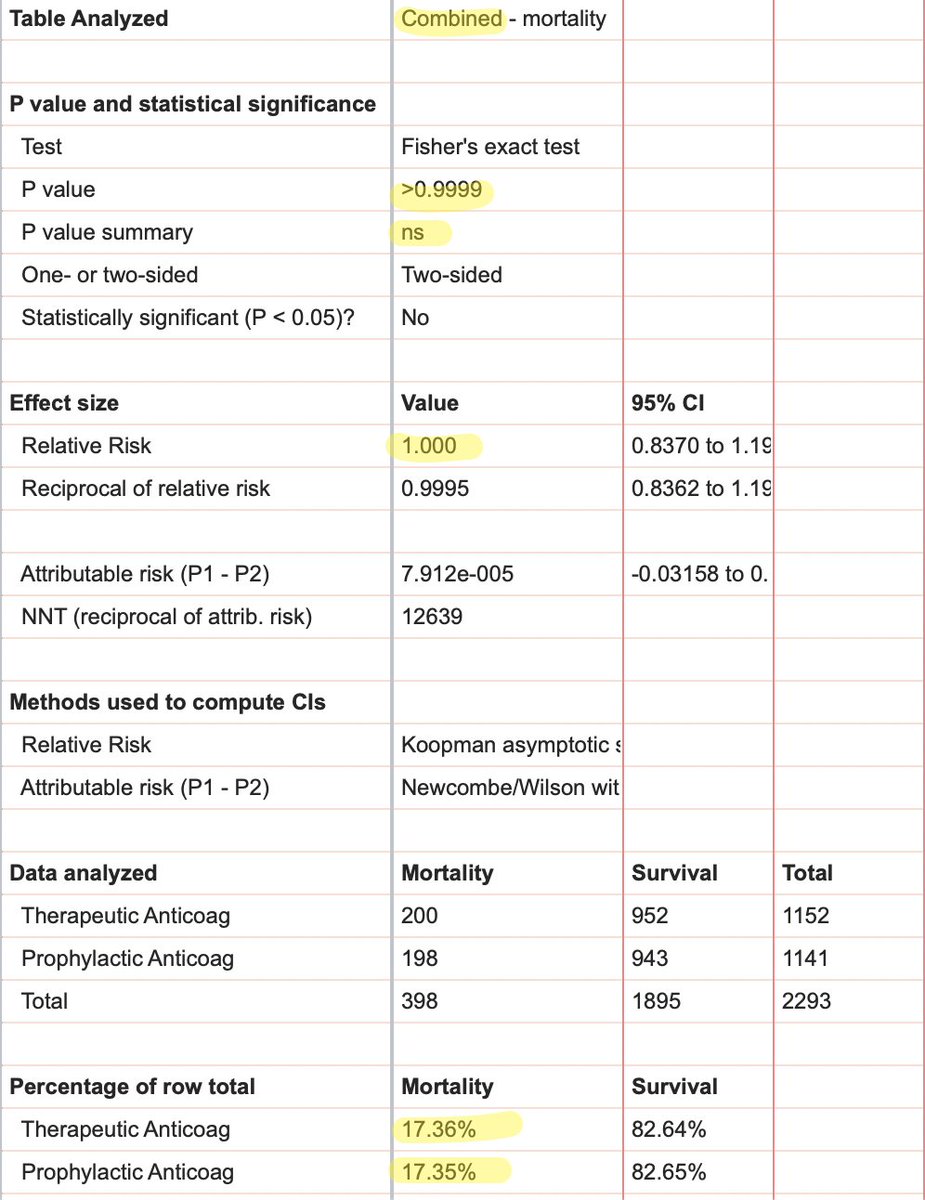
We do have some info about mortality.
-TA non-significantly mortality in moderate disease (5.7% vs 7.7%)
mortality in moderate disease (5.7% vs 7.7%)
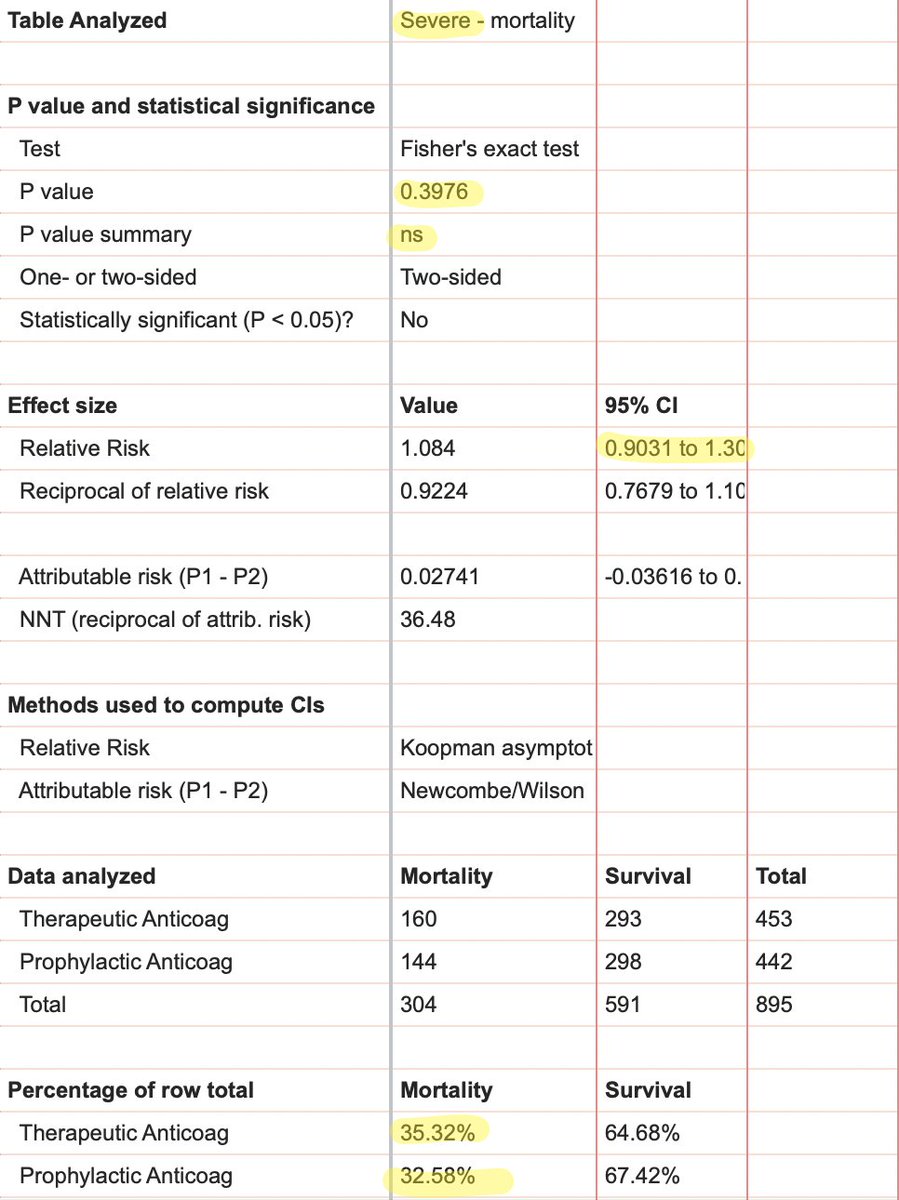
-TA non-significantly mortality in severe disease (35.3% vs 32.6%)
mortality in severe disease (35.3% vs 32.6%)
-mortality is darn near identical when severe & moderate groups are combined (17.36% vs 17.35%)
5/
-TA non-significantly
 mortality in moderate disease (5.7% vs 7.7%)
mortality in moderate disease (5.7% vs 7.7%)-TA non-significantly
 mortality in severe disease (35.3% vs 32.6%)
mortality in severe disease (35.3% vs 32.6%)-mortality is darn near identical when severe & moderate groups are combined (17.36% vs 17.35%)
5/
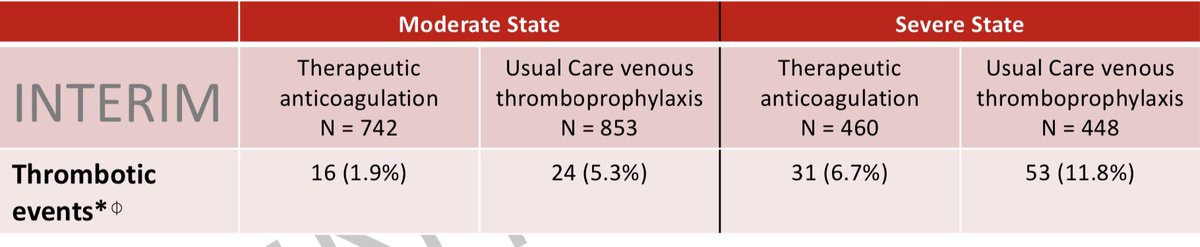
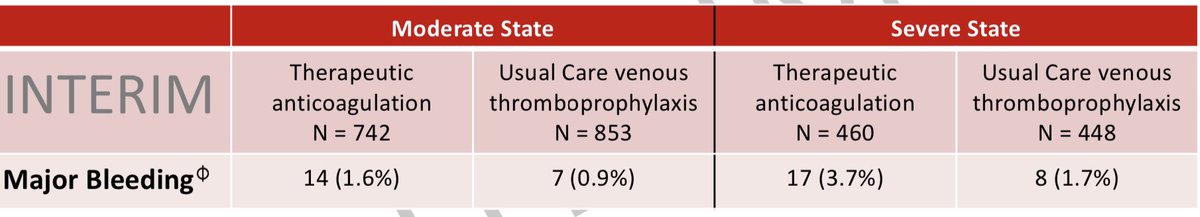
Unsurprisingly, TA deceased rates of thrombosis but increased rates of major bleeding compared to usual care.
Crossover may be a problem; presumably they stopped TA in pts who bled & started it in usual care pts who developed thrombosis. This could bias the results either way.
Crossover may be a problem; presumably they stopped TA in pts who bled & started it in usual care pts who developed thrombosis. This could bias the results either way.
What can we conclude from these large, well-done RCTs of therapeutic anticoagulation in COVID19?
Not much until we read the actual peer-reviewed paper, I'm afraid. Many key details are missing from the interim release. (& that's totally reasonable btw; it's a pre-pre-pub)
7/
Not much until we read the actual peer-reviewed paper, I'm afraid. Many key details are missing from the interim release. (& that's totally reasonable btw; it's a pre-pre-pub)
7/
I think based on this interim data we can say that TA probably has a small benefit in moderate disease & no benefit (or even harm) in severe disease
On the spectrum of game-changer (dexamethasone) to nothing burger (remdesivir), therapeutic anticoagulation seems more like a
8
On the spectrum of game-changer (dexamethasone) to nothing burger (remdesivir), therapeutic anticoagulation seems more like a

8
Lingering questions:
-so should we all abandon TA for COVID pts in the ICU & embrace it on the wards? Let's wait for the pub
-what to do if a pt with moderate disease on TA gets sicker & requires ICU care; continue TA or not? The investigators are exploring this subgroup now
9/9
-so should we all abandon TA for COVID pts in the ICU & embrace it on the wards? Let's wait for the pub
-what to do if a pt with moderate disease on TA gets sicker & requires ICU care; continue TA or not? The investigators are exploring this subgroup now
9/9

 Read on Twitter
Read on Twitter