on serotonin, SSRIs, serotonin-blockers, and COVID19
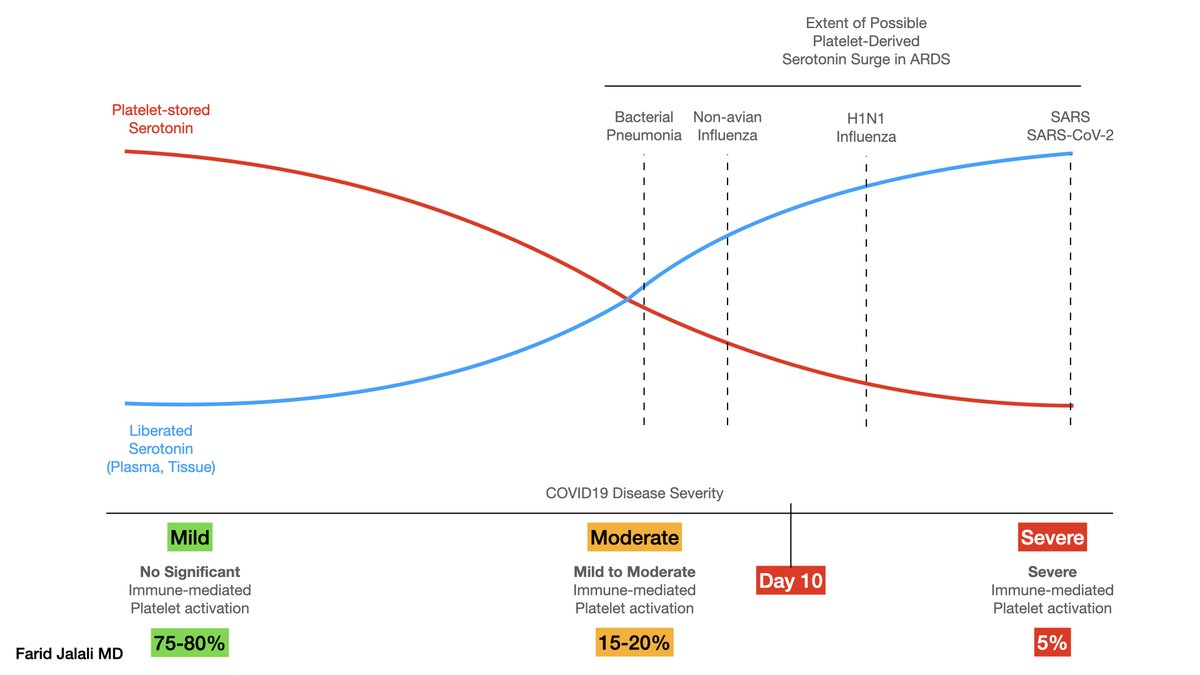
on serotonin, SSRIs, serotonin-blockers, and COVID19All causes of ARDS are associated with activation of resident lung platelets and megakaryocytes. The degree to which this activation occurs differs between various etiologies of ARDS, as demonstrated in ...
... the work by @UofUHealth a few years ago comparing in-vivo platelet activation between H1N1 ARDS and ARDS of bacterial pneumonia, showing platelet activation responses during A(H1N1) are enhanced—exceeding responses in patients with bacterial pneumonia https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3367488/
Similar platelet hyperreactivity, exceeding that of other etiologies of ARDS including bacterial pneumonia, has been demonstrated in COVID19 (in-press, preprint).
While awaiting publication of this data, it is worthwhile to review the ramifications of this hyperreactivity ...
While awaiting publication of this data, it is worthwhile to review the ramifications of this hyperreactivity ...
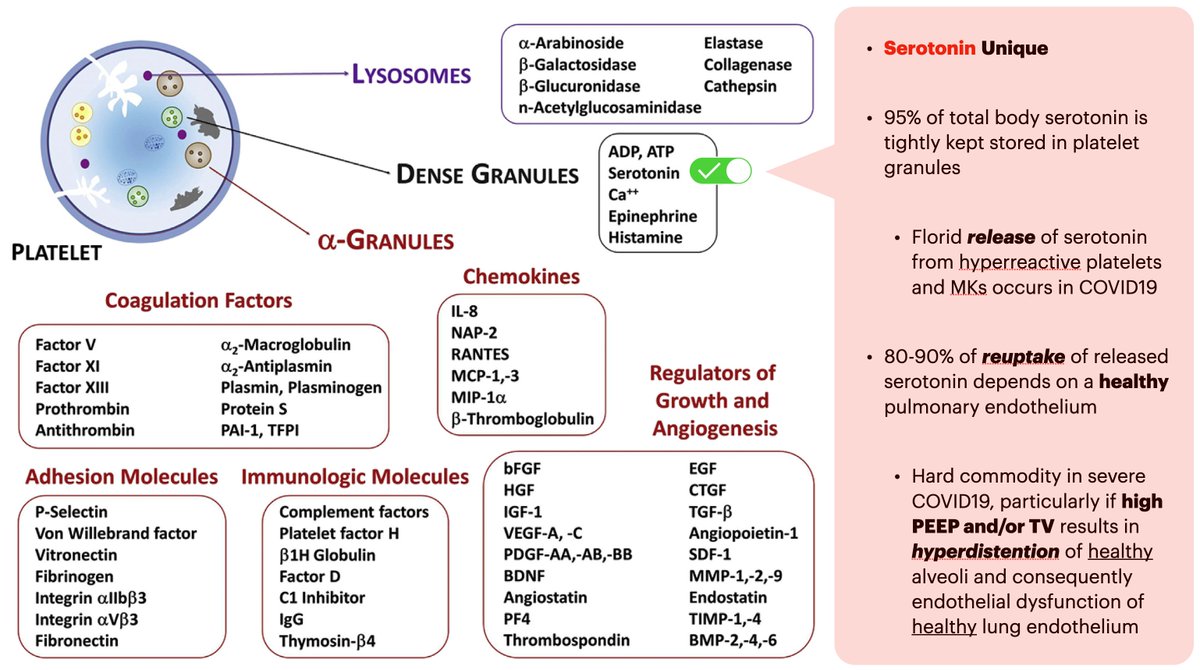
One of the natural results of platelet activation is the release of its granule content.
Among various molecules stored in platelet granules, serotonin is unique, in that it is predominantly stored in platelets (95% of all serotonin), and ....
Among various molecules stored in platelet granules, serotonin is unique, in that it is predominantly stored in platelets (95% of all serotonin), and ....
... serotonin's reuptake is reliant on a healthy pulmonary endothelium, a commodity that could be scarce during ARDS, particularly in COVID-19, that has been demonstrated to cause such profound pulmonary microangiopathy and endotheliopathy ... https://www.nejm.org/doi/full/10.1056/NEJMoa2015432
As platelets degranulate their serotonin content, serotonin accumulates inside plasma and within the perivascular milieu adjacent to where platelets happen to activate.
In ARDS, this perivascular milieu is within and around the pulmonary capillaries.
In ARDS, this perivascular milieu is within and around the pulmonary capillaries.
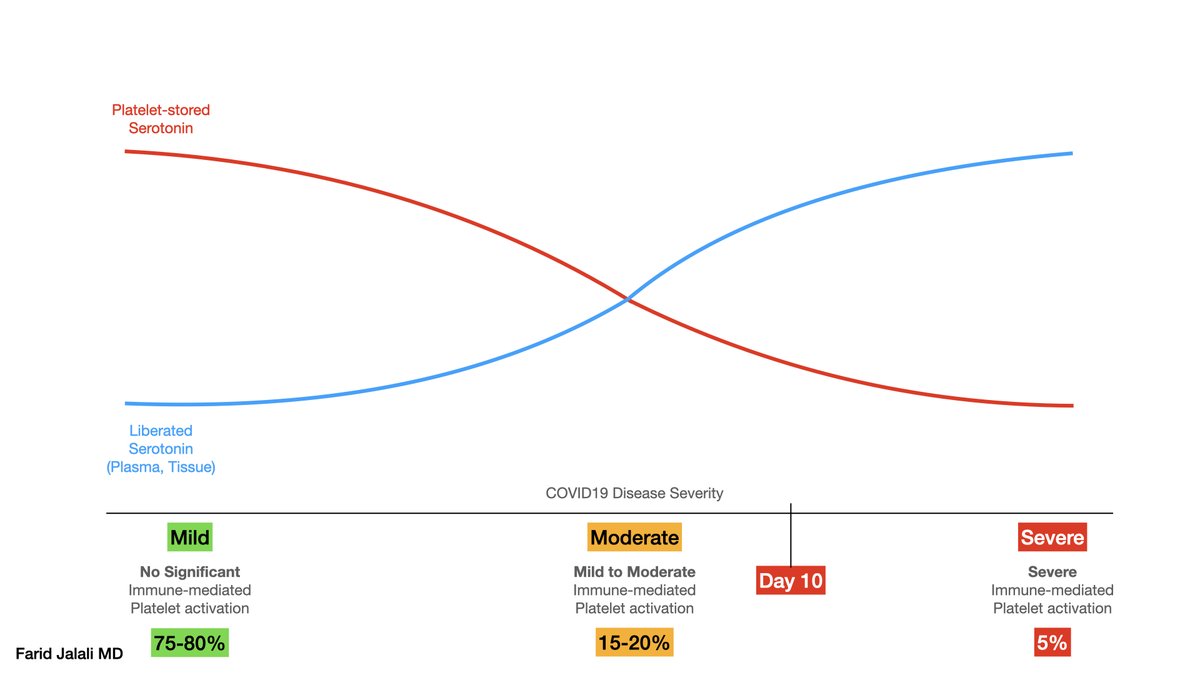
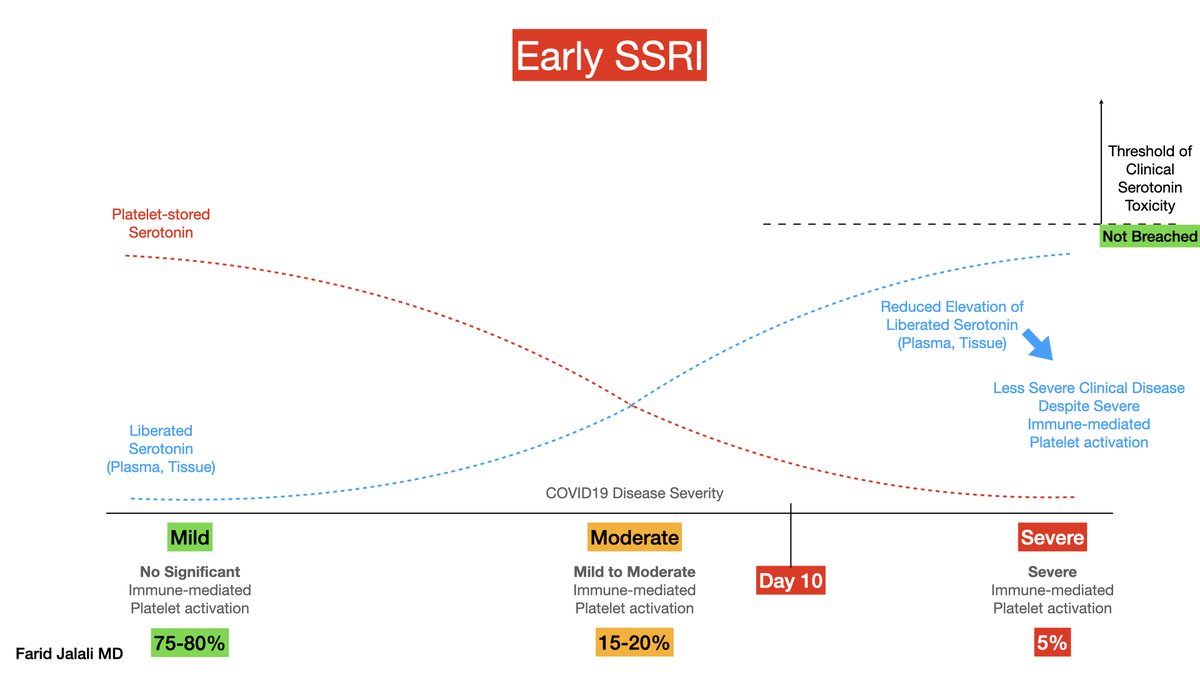
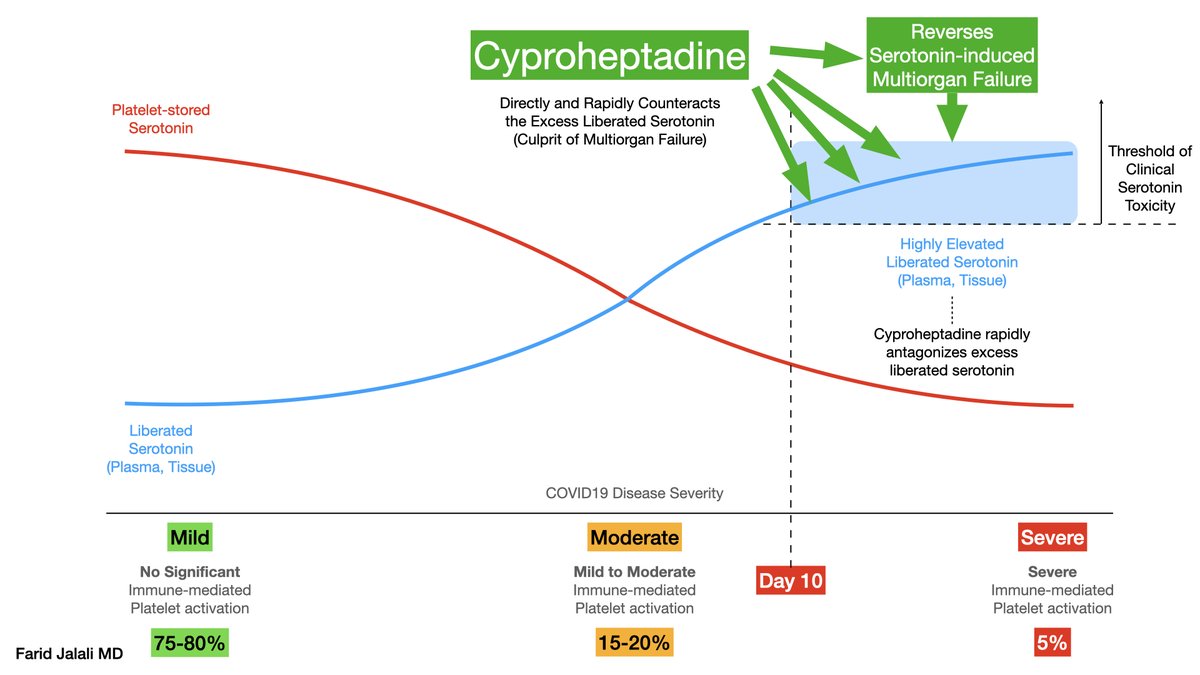
This degranulation of serotonin out of platelets, into the plasma and surrounding tissue, is illustrated in the graph below:
The intensity of platelet activation in COVID19 is dependent on the degree of immune-mediated platelet activation, as demonstrated in many studies, most prominently in the work cited below:
https://doi.org/10.1182/blood.2020008762
https://doi.org/10.1182/blood.2020008762
As the severity of immune-mediated platelet activation increases, the degree of displacement of serotonin out of platelets into the plasma and the perivascular milieu increases, again as demonstrated in below schematic, in the bottom row (x-axis)
Building upon the recent preprint and in-press evidence demonstrating a heightened state of platelet hyperreactivity in COVID19 vs other etiologies of ARDS, this diagram is labeled (hypothetically) with various causes of ARDS:
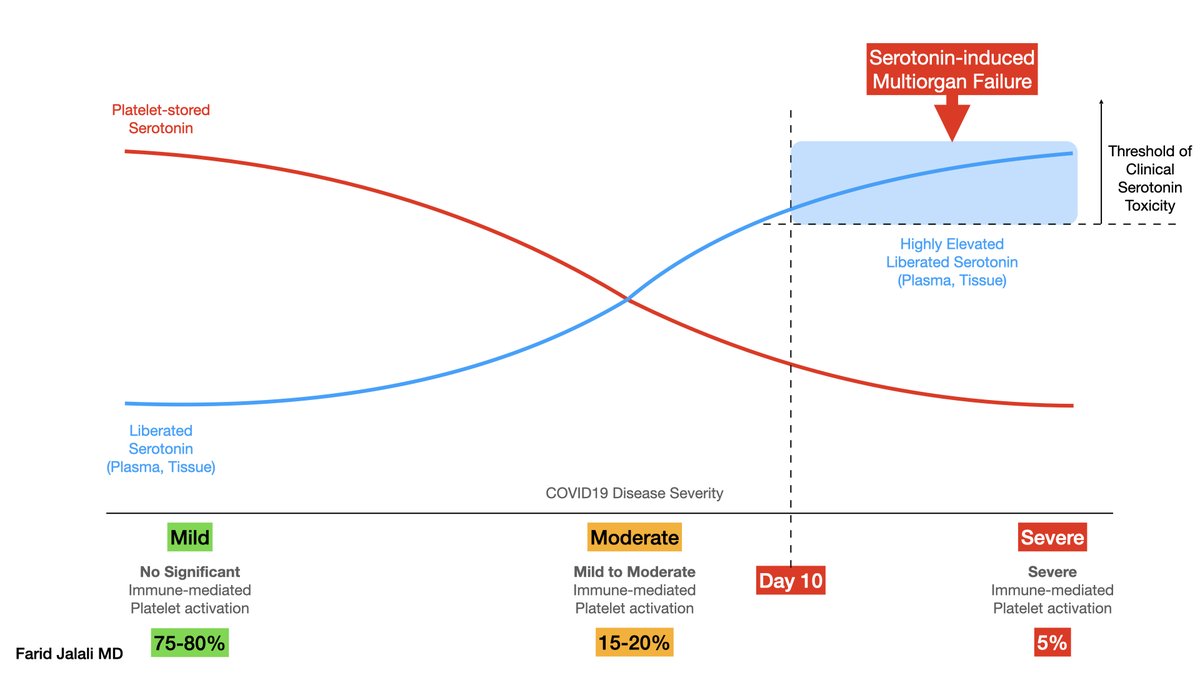
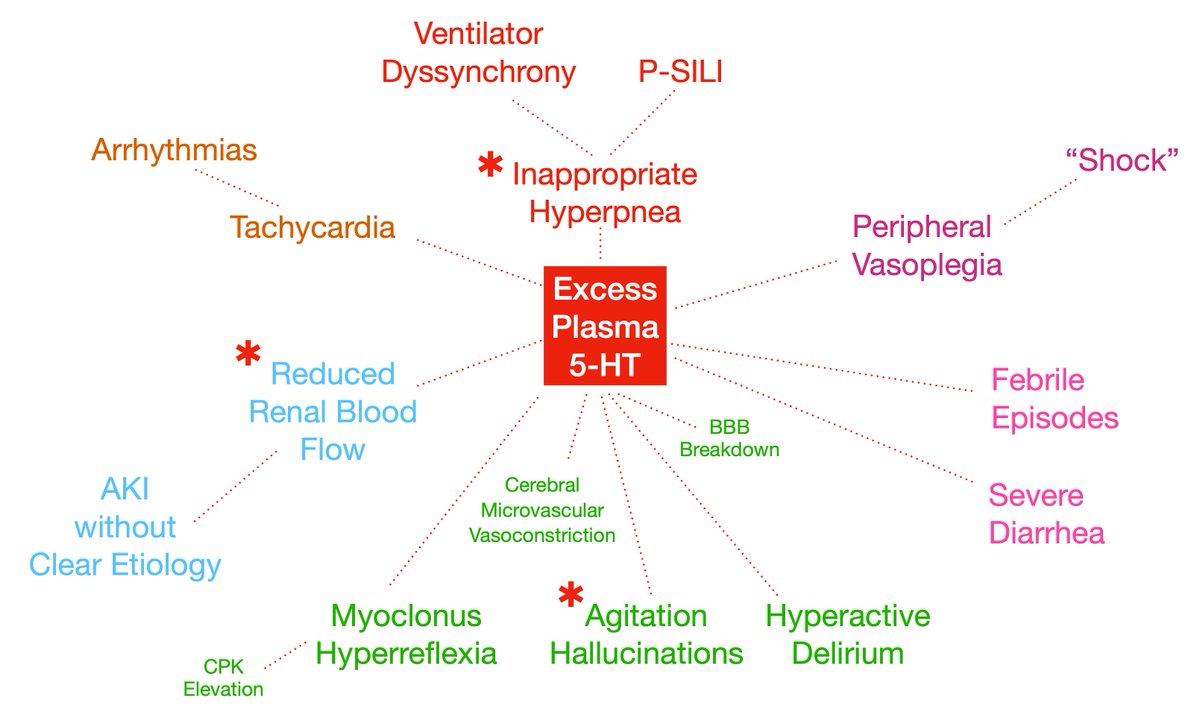
It is hypothesized (and data coming) that SARS-CoV-2 ARDS can cause, in most severe cases, such a heightened state of platelet activation, that the degree of serotonin displacement could reach a pathologic state with clinical manifestations resembling that of serotonin syndrome
The evidence for this hyperserotonergic state has been indirectly present with a significant incidence of inducible clonus and hyperreflexia in severe COVID19, published in NEJM: https://www.nejm.org/doi/full/10.1056/NEJMc2008597
Additionally, more direct association has been demonstrated for this hyperserotonergic state as a possible culprit for the diarrhea associated (and commonly seen) in severe COVID19: https://gut.bmj.com/content/early/2021/01/04/gutjnl-2020-323542
Additionally, a JAMA double-blind placebo-controlled RCT of fluvoxamine has been demonstrated to prevent severe COVID19 manifestations. This trial was done by @AngelaReiersen and colleagues, and a larger trial is ongoing to confirm the earlier results: https://jamanetwork.com/journals/jama/fullarticle/2773108
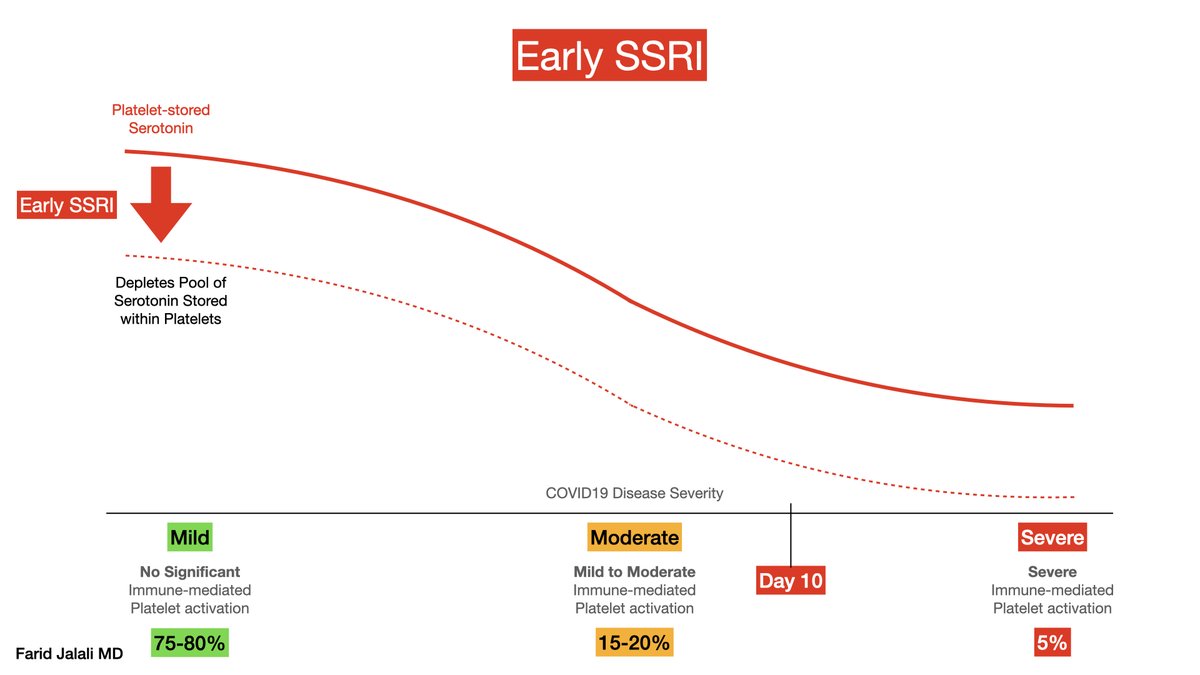
The question that is often asked is: why would an SSRI improve an alleged hyperserotonergic state (that I so often tweet about).
Shouldn't an SSRI, believed to "increase serotonin" in popular culture (and among many medical professionals), exert an opposite and harmful effect?
Shouldn't an SSRI, believed to "increase serotonin" in popular culture (and among many medical professionals), exert an opposite and harmful effect?
The answer is No!
And let me explain below:
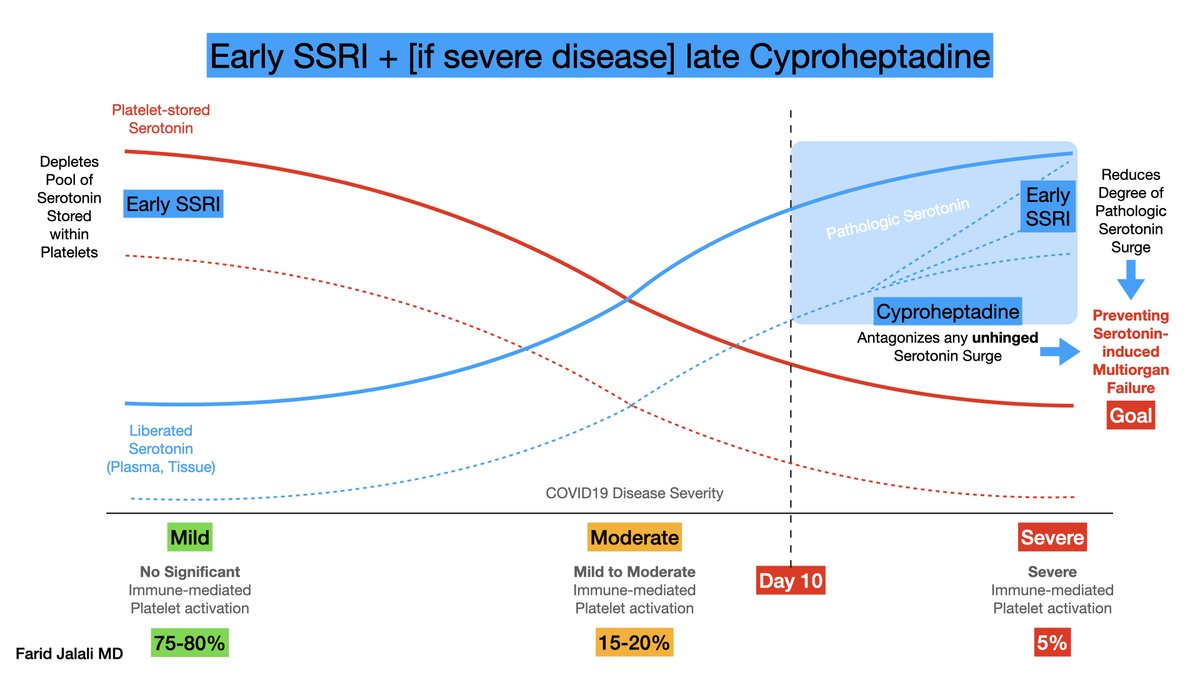
SSRIs, when started early in the course of disease, or if used chronically, in fact *deplete* the serotonin stores of platelets.
And let me explain below:
SSRIs, when started early in the course of disease, or if used chronically, in fact *deplete* the serotonin stores of platelets.
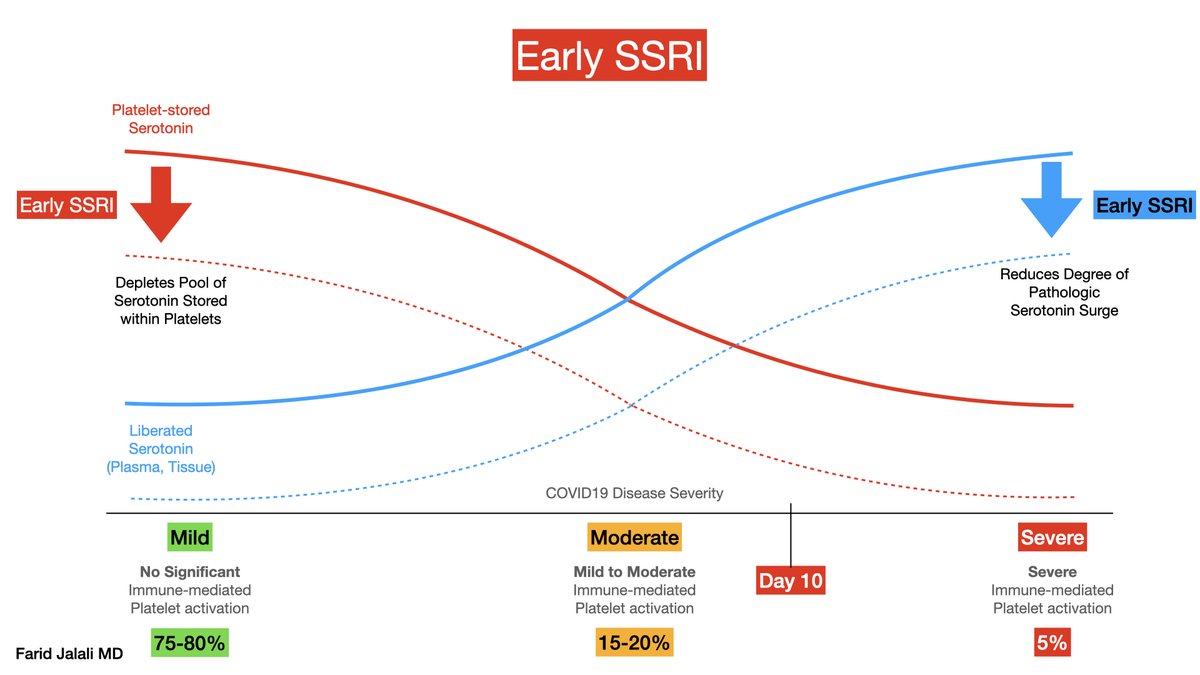
This pre-emptive depletion of serotonin within platelets means that if - and when - intense immune-mediated platelet activation (of severe COVID19) occurs, then there is LESS serotonin bioavailable for *pathologic* displacement into the plasma and the perivascular milieu.
This in return means that a hyperserotonergic state associated with severe COVID19 is less likely to occur with early/chronic SSRI, should a patient proceed to severe immune-mediated platelet activation.
This is beneficial, as excess serotonin release is often pathologic.
This is beneficial, as excess serotonin release is often pathologic.
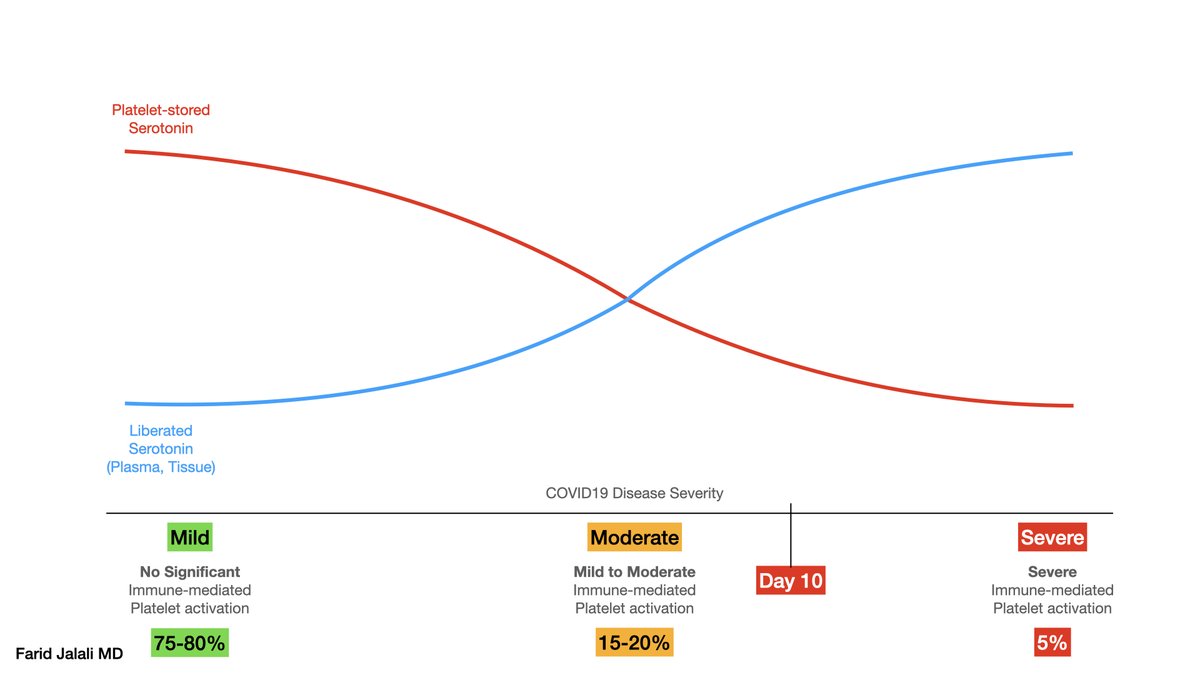
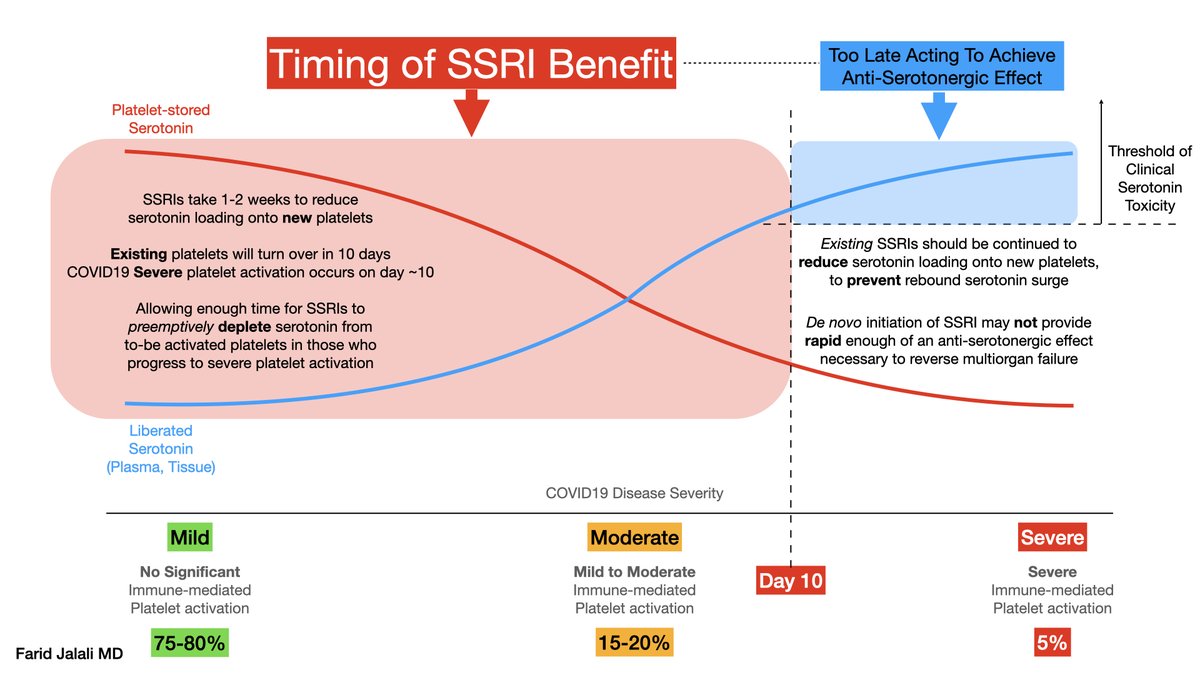
Now the question is, how late can SSRIs be administered to exert their protective effect in COVID19, this enigmatic severely-platelet-activating disease?
The answer is: earlier is better, chronic is protective, and late is often too late to exert a protective effect.
The answer is: earlier is better, chronic is protective, and late is often too late to exert a protective effect.
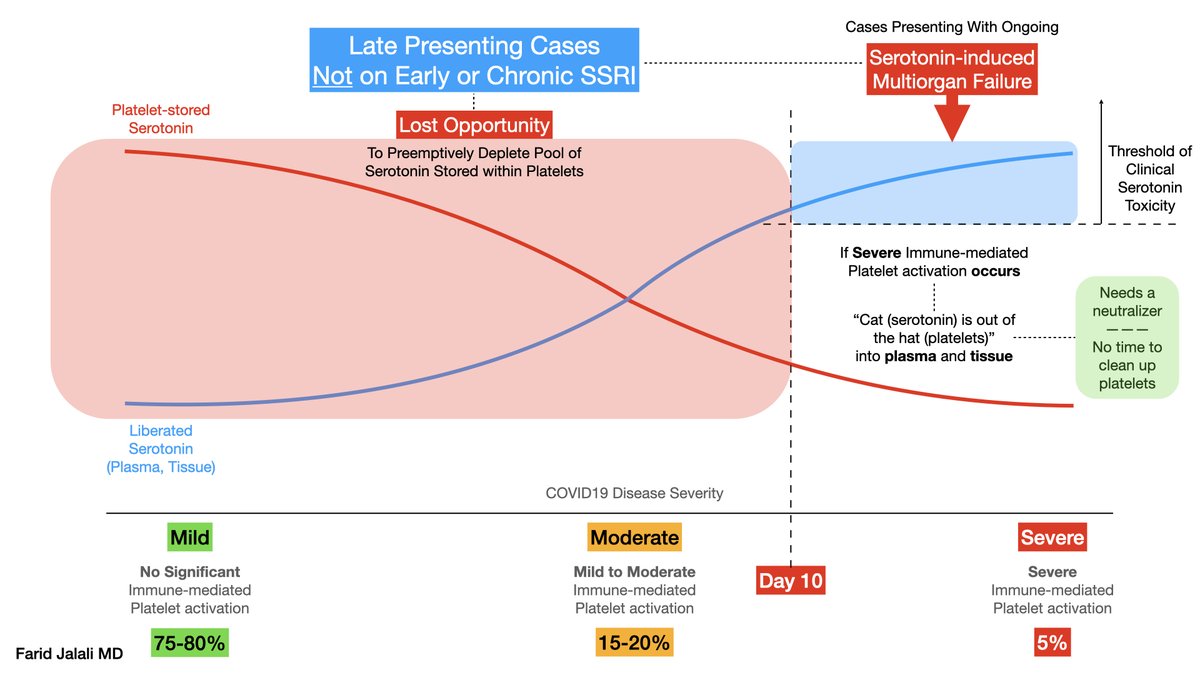
Unfortunately, where we are in this pandemic, is a stage where patients are presenting very frequently at a severe stage, often very late, to the hospitals.
At that stage (day 10+), the "cat" (serotonin) is out of the "hat" (platelets) ... A neutralizer may be needed.
At that stage (day 10+), the "cat" (serotonin) is out of the "hat" (platelets) ... A neutralizer may be needed.
In other words, no amount of "vacuuming" serotonin out of platelets (e.g. SSRI) will resolve the carnage created by the *already liberated* serotonin soaking up the plasma and perivascular (lung) tissue.
This needs an intervention that acts rapidly and directly to prevent below:
This needs an intervention that acts rapidly and directly to prevent below:
Here is where direct serotonin blockade, in the form of cyproheptadine, comes in.
Anecdotally, cyproheptadine has reversed multiple puzzling facets of severe COVID19, indicating a serotonin mediation at play:
- Hyperpnea
- Renal failure
- Agitation
- Diarrhea
- Fever
- Shock
Anecdotally, cyproheptadine has reversed multiple puzzling facets of severe COVID19, indicating a serotonin mediation at play:
- Hyperpnea
- Renal failure
- Agitation
- Diarrhea
- Fever
- Shock
So in essence, early SSRI is achieving the same effect (preemptively) as late direct serotonin antagonism such as with Cyproheptadine.
As @gattinon and many others have tried to teach us since the beginning, various stages of this disease require various interventions.
As @gattinon and many others have tried to teach us since the beginning, various stages of this disease require various interventions.
An ideal scenario to prevent the hyperserotonergic multi-organ failure that is inherent to severe COVID19 would be a combination of reducing pool of bioavailable serotonin (early SSRI) combined with, if severe disease occurs, a direct serotonin antagonist (cyproheptadine)

 Read on Twitter
Read on Twitter