There are now several studies out there that together give a useful indication of the possible role of pre-existing immunity (antibodies/T-cells etc.) in SARS-CoV-2 dynamics. A few thoughts/links... 1/
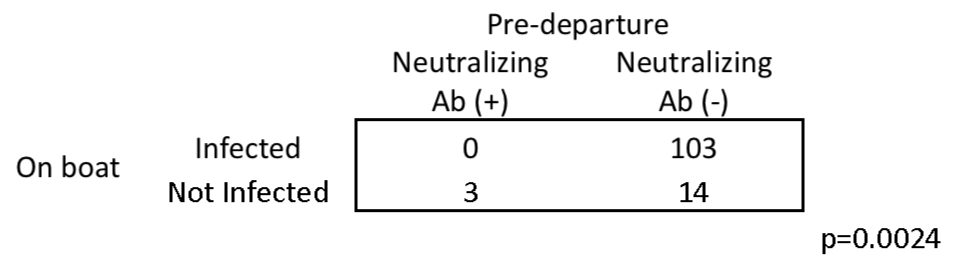
First, there are several well-defined outbreaks in which very large % of people had detectable infection (i.e. PCR or developed antibodies). E.g. 103/117 on boat ( https://www.medrxiv.org/content/10.1101/2020.08.13.20173161v1), 11/13 at meeting ( https://wwwnc.cdc.gov/eid/article/26/8/20-1235_article), 7/8 & 8/8 at meals ( https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30462-1/fulltext) 2/
This would suggest there isn't substantial % of adult population that can't get infected if exposed. This is consistent with data from healthcare ( https://www.medrxiv.org/content/10.1101/2020.06.08.20120584v1)& care homes ( https://www.medrxiv.org/content/10.1101/2020.08.10.20171413v1). If enough exposure & look hard enough, seems will find infections 3/
But that doesn't mean nobody at all is immune from infection. In that fishing boat study ( https://www.medrxiv.org/content/10.1101/2020.08.13.20173161v1), a small number (3 out of 120) had neutralising antibodies, perhaps from earlier SARS-CoV-2 infection, and they didn't get infected again. 4/
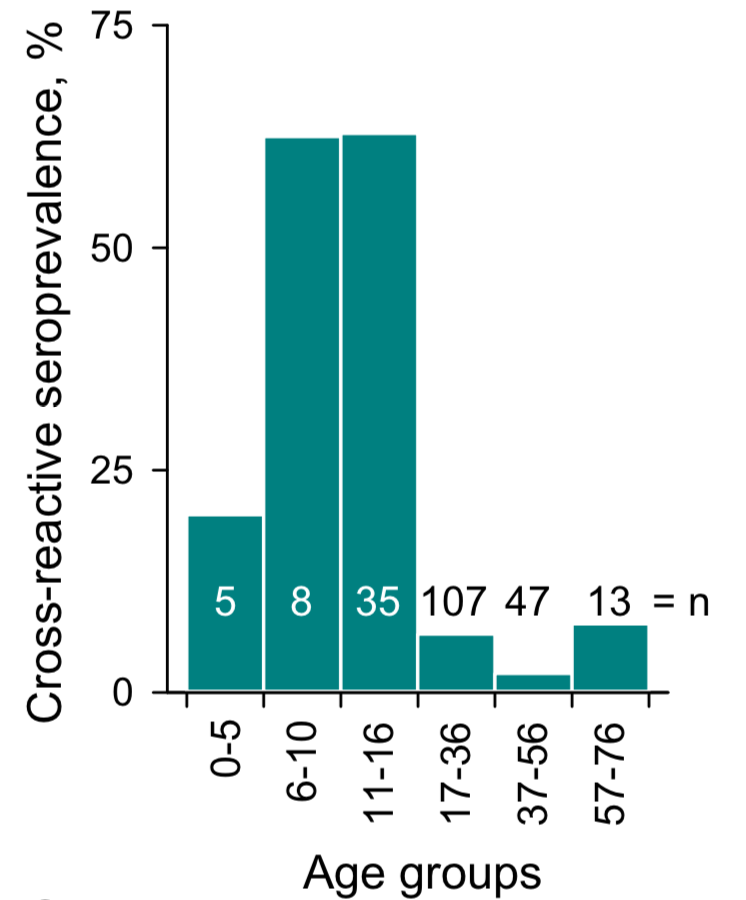
Then there's children. There's evidence they may be less susceptible to infection ( https://www.nature.com/articles/s41591-020-0962-9) and younger groups not previously exposed to SARS-CoV-2 have cross-reactive antibodies, which may help explain reduced risk ( https://www.biorxiv.org/content/10.1101/2020.05.14.095414v1). 5/
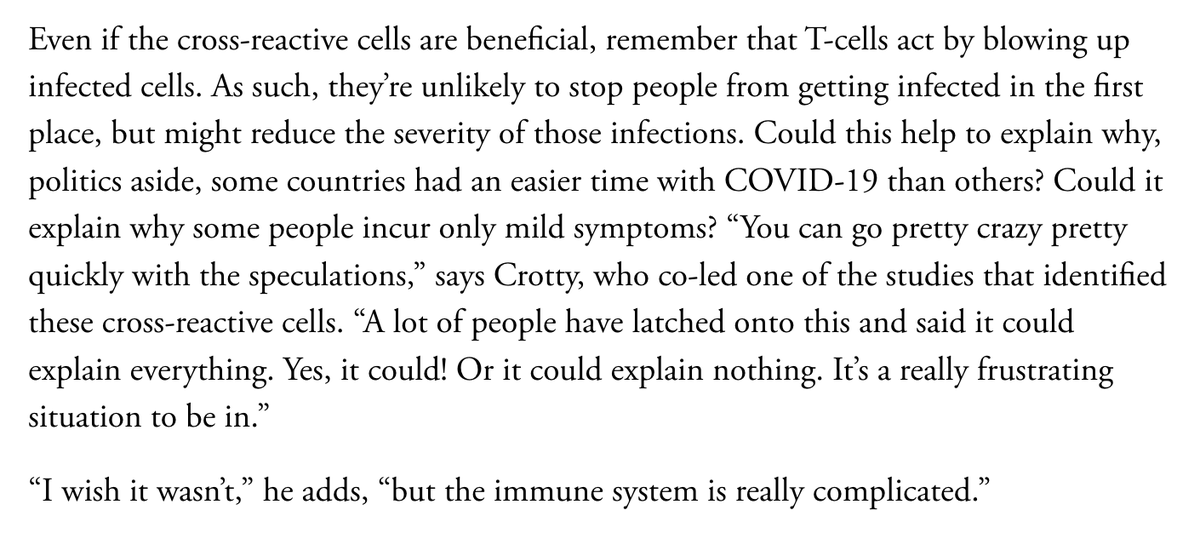
So far we've been talking about immunity against *infection*, but there is also the question of protection against *disease*. Clearly some people get less severe symptoms/disease, suggesting some role of immunity... 6/
There's evidence of pre-existing T-cell responses in uninfected people ( https://www.sciencedirect.com/science/article/pii/S0092867420306103) and that responses persist after infection ( https://www.cell.com/cell/fulltext/S0092-8674(20)31008-4). 7/
This would be good news, and consistent with circulating seasonal 'common cold' coronaviruses, which can reinfect people but seem to result in milder symptoms on reinfection (e.g. https://pubmed.ncbi.nlm.nih.gov/2170159/ ). 8/
But important to note protection from infection affects epidemic dynamics more than protection from disease. In herd immunity calculations etc, what matters is whether people transmit, not how ill they get. So immunity against disease won't necessarily stop outbreaks. 9/
It's also worth remembering that any pre-existing immunity from infection (e.g. among children) is already 'priced in' to the reproduction number. So need to be careful about interpreting how immunity might influence dynamics. https://twitter.com/AdamJKucharski/status/1286643105001811968?s=20 10/
Obviously there's still a lot more we to need to learn about SARS-CoV-2 immunity (e.g. https://www.nature.com/articles/s41577-020-0389-z), so would be interested to hear about any other emerging studies that shed light on this issue (or if immunologists want to flag anything I've missed). 11/
I'd also recommend this useful primer by @edyong209 about why these immunological questions are important – but also very challenging https://www.theatlantic.com/health/archive/2020/08/covid-19-immunity-is-the-pandemics-central-mystery/614956/ 12/12

 Read on Twitter
Read on Twitter