1/15
Why do patients with liver injury or dysfunction have conjugated hyperbilirubinemia?
If hepatocytes conjugate, why doesn't this "liver function" decrease in settings of severe inflammatory or fibrosis?
Before I offer a fuller explanation, I'll ask you: which plays a role?
Why do patients with liver injury or dysfunction have conjugated hyperbilirubinemia?
If hepatocytes conjugate, why doesn't this "liver function" decrease in settings of severe inflammatory or fibrosis?
Before I offer a fuller explanation, I'll ask you: which plays a role?
2/
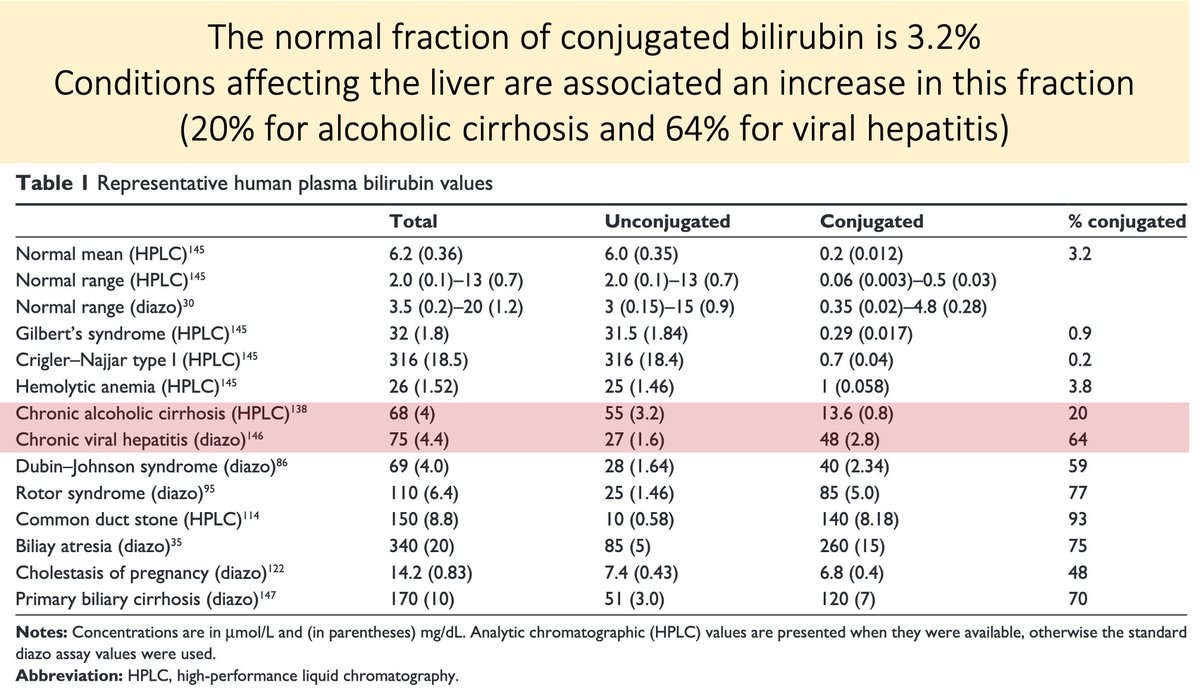
Let's start by confirming that liver diseases present with conjugated hyperbilirubinemia.
Here is the fraction of total bilirubin that is conjugated in 3 situations:
 Normal: 3.2%
Normal: 3.2%
 Chronic alcoholic cirrhosis: 20%
Chronic alcoholic cirrhosis: 20%
 Chronic viral hepatitis: 64%
Chronic viral hepatitis: 64%
https://www.ncbi.nlm.nih.gov/pubmed/25214800
Let's start by confirming that liver diseases present with conjugated hyperbilirubinemia.
Here is the fraction of total bilirubin that is conjugated in 3 situations:
 Normal: 3.2%
Normal: 3.2% Chronic alcoholic cirrhosis: 20%
Chronic alcoholic cirrhosis: 20% Chronic viral hepatitis: 64%
Chronic viral hepatitis: 64%https://www.ncbi.nlm.nih.gov/pubmed/25214800
3/
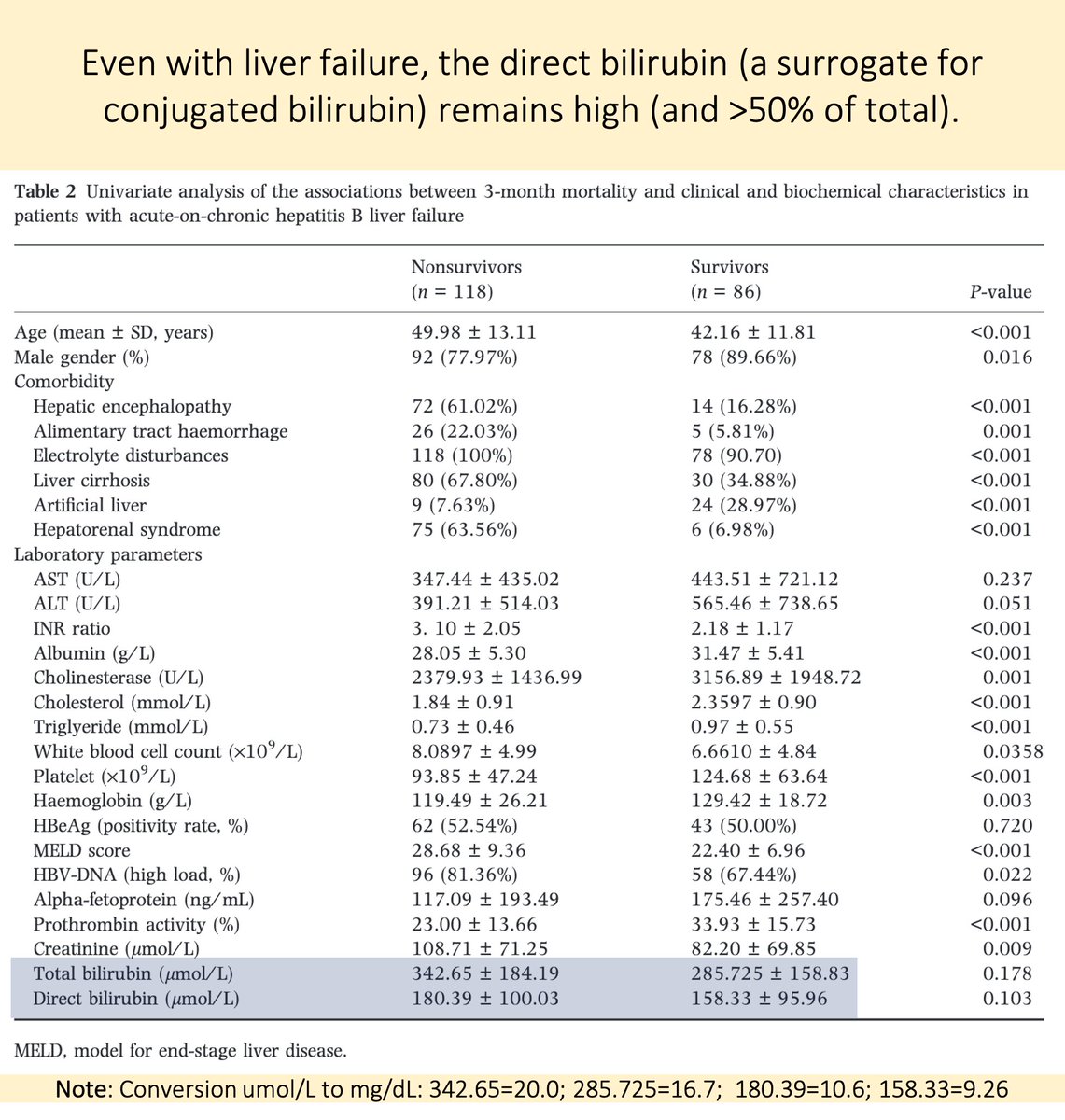
Even as the liver fails, its ability to conjugate bilirubin remains.
In one study of liver failure from hepatitis B, patients still had elevated conjugated bilirubin levels:
10.6 mg/dL for nonsurvivors
9.3 mg/dL for survivors
https://www.ncbi.nlm.nih.gov/pubmed/28440304
Even as the liver fails, its ability to conjugate bilirubin remains.
In one study of liver failure from hepatitis B, patients still had elevated conjugated bilirubin levels:
10.6 mg/dL for nonsurvivors
9.3 mg/dL for survivors
https://www.ncbi.nlm.nih.gov/pubmed/28440304
4/
Next, we need to review a few key features of bilirubin handling:
 Unconjugated bilirubin is taken by hepatocytes via facilitated and simple diffusional processes
Unconjugated bilirubin is taken by hepatocytes via facilitated and simple diffusional processes
 Bilirubin is conjugated to glucuronic acid by uridine diphosphate glycosyltransferase 1A1 (UGT1A1)
Bilirubin is conjugated to glucuronic acid by uridine diphosphate glycosyltransferase 1A1 (UGT1A1)
Next, we need to review a few key features of bilirubin handling:
 Unconjugated bilirubin is taken by hepatocytes via facilitated and simple diffusional processes
Unconjugated bilirubin is taken by hepatocytes via facilitated and simple diffusional processes Bilirubin is conjugated to glucuronic acid by uridine diphosphate glycosyltransferase 1A1 (UGT1A1)
Bilirubin is conjugated to glucuronic acid by uridine diphosphate glycosyltransferase 1A1 (UGT1A1)
5/
 Soluble conjugated bilirubin (CB) is transported into bile via ATP-dependent multidrug resistance-associated protein 2 (MRP2)
Soluble conjugated bilirubin (CB) is transported into bile via ATP-dependent multidrug resistance-associated protein 2 (MRP2)
 CB is then excreted from the body
CB is then excreted from the body
 Conjugation occurs within the endoplasmic reticulum of hepatocytes. So, we need hepatocytes to conjugate!
Conjugation occurs within the endoplasmic reticulum of hepatocytes. So, we need hepatocytes to conjugate!
 Soluble conjugated bilirubin (CB) is transported into bile via ATP-dependent multidrug resistance-associated protein 2 (MRP2)
Soluble conjugated bilirubin (CB) is transported into bile via ATP-dependent multidrug resistance-associated protein 2 (MRP2) CB is then excreted from the body
CB is then excreted from the body Conjugation occurs within the endoplasmic reticulum of hepatocytes. So, we need hepatocytes to conjugate!
Conjugation occurs within the endoplasmic reticulum of hepatocytes. So, we need hepatocytes to conjugate!
6/
Ok, so we have identified the paradox that requires explanation:
 How can a process (conjugation) that requires hepatocellular function continue when it appears that the liver is otherwise inflamed, fibrotic, or failing?
How can a process (conjugation) that requires hepatocellular function continue when it appears that the liver is otherwise inflamed, fibrotic, or failing?
Ok, so we have identified the paradox that requires explanation:
 How can a process (conjugation) that requires hepatocellular function continue when it appears that the liver is otherwise inflamed, fibrotic, or failing?
How can a process (conjugation) that requires hepatocellular function continue when it appears that the liver is otherwise inflamed, fibrotic, or failing?
7/
To understand an answer, recall that compounds may undergo two phases of biotransformation in the liver:
 Phase 1: oxidation/reduction/hydrolysis/hydration (via CYP450)
Phase 1: oxidation/reduction/hydrolysis/hydration (via CYP450)
 Phase 2: conjugation
Phase 2: conjugation
Xenobiotics typically use Phases I and II
Bilirubin only undergoes Phase II
To understand an answer, recall that compounds may undergo two phases of biotransformation in the liver:
 Phase 1: oxidation/reduction/hydrolysis/hydration (via CYP450)
Phase 1: oxidation/reduction/hydrolysis/hydration (via CYP450) Phase 2: conjugation
Phase 2: conjugationXenobiotics typically use Phases I and II
Bilirubin only undergoes Phase II
8/
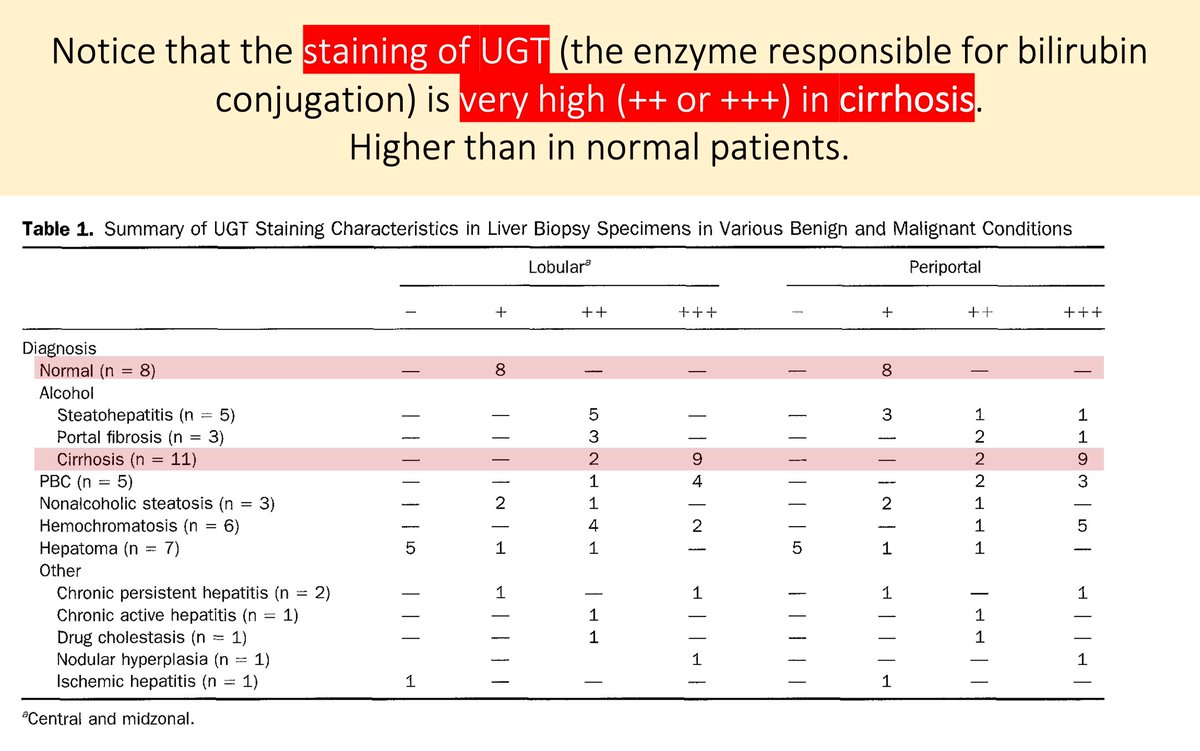
Here's the first part of the answer to our question:
In some liver diseases, there is upregulation of UGT enzyme content in the remaining viable hepatocytes.
i.e., Phase II function remains. It's worth noting that Phase I is often quite affected.
https://www.ncbi.nlm.nih.gov/pubmed/7729639
Here's the first part of the answer to our question:
In some liver diseases, there is upregulation of UGT enzyme content in the remaining viable hepatocytes.
i.e., Phase II function remains. It's worth noting that Phase I is often quite affected.
https://www.ncbi.nlm.nih.gov/pubmed/7729639
9/
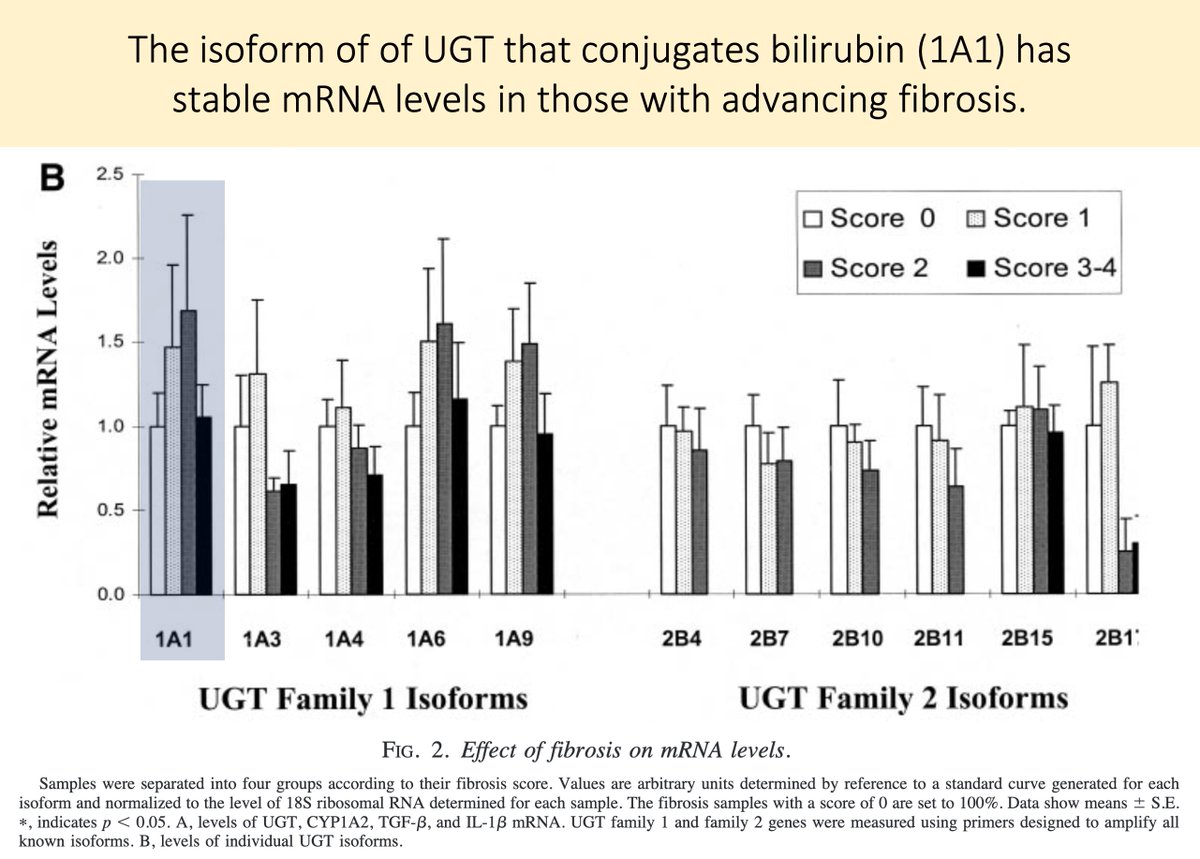
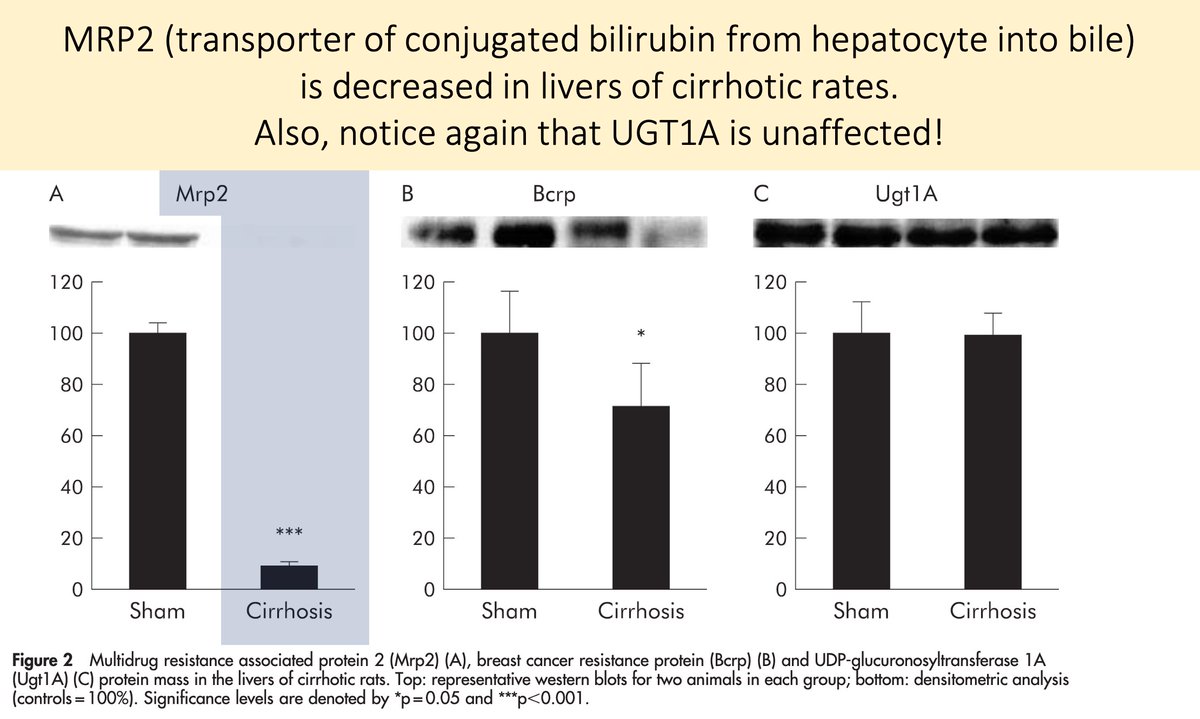
Furthermore, the levels of the specific isoform of UGT that conjugates bilirubin (UGT1A1) are stable as the degree of liver fibrosis progresses.
Even in severe fibrosis and cirrhosis.
https://www.ncbi.nlm.nih.gov/pubmed/11792680
Furthermore, the levels of the specific isoform of UGT that conjugates bilirubin (UGT1A1) are stable as the degree of liver fibrosis progresses.
Even in severe fibrosis and cirrhosis.
https://www.ncbi.nlm.nih.gov/pubmed/11792680
10/
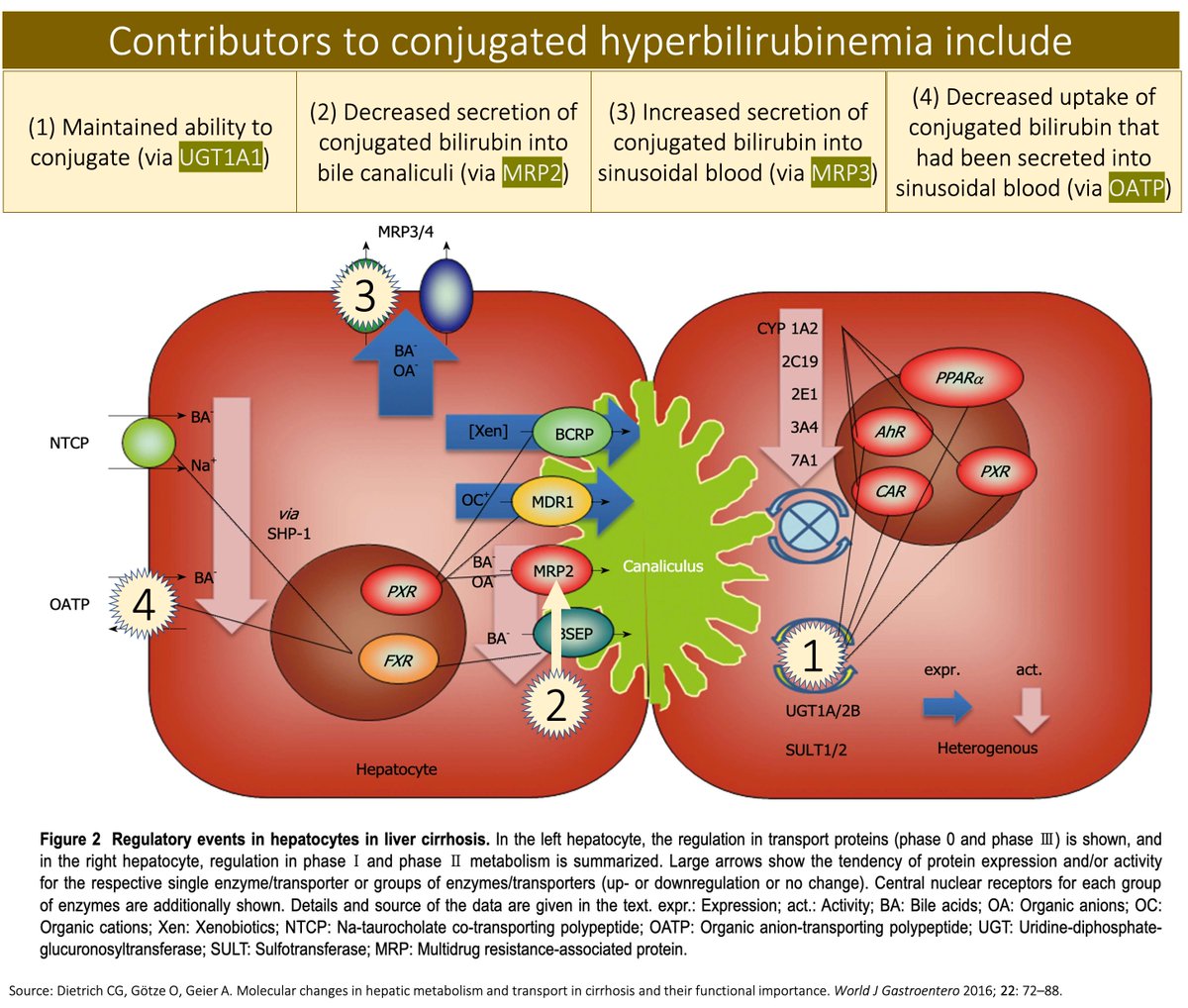
That UGT1A1 function remains despite liver disease explains the preserved ability to conjugate.
But why do these patients have conjugated hyperbilirubinemia? Why isn't it just cleared in the normal manner?
One problem is with the decreased transfer of bilirubin into bile.
That UGT1A1 function remains despite liver disease explains the preserved ability to conjugate.
But why do these patients have conjugated hyperbilirubinemia? Why isn't it just cleared in the normal manner?
One problem is with the decreased transfer of bilirubin into bile.
11/
Recall that MRP2 transports conjugated bilirubin from the hepatocyte into the bile.
Part of the explanation for conjugated hyperbilirubinemia in liver disease is DOWNregulation of MRP2.
This is best described in primary biliary cholangitis.
https://www.ncbi.nlm.nih.gov/pubmed/15542527
Recall that MRP2 transports conjugated bilirubin from the hepatocyte into the bile.
Part of the explanation for conjugated hyperbilirubinemia in liver disease is DOWNregulation of MRP2.
This is best described in primary biliary cholangitis.
https://www.ncbi.nlm.nih.gov/pubmed/15542527
12/
We have now explained why:
 Conjugation persists (stable UGT1A1)
Conjugation persists (stable UGT1A1)
 Conjugated bilirubin remains within hepatocytes (↓MRP2)
Conjugated bilirubin remains within hepatocytes (↓MRP2)
In order for a patient to have conjugated hyperbilirubinemia this conjugated bilirubin must somehow make it back into the blood.
We need more.
We have now explained why:
 Conjugation persists (stable UGT1A1)
Conjugation persists (stable UGT1A1) Conjugated bilirubin remains within hepatocytes (↓MRP2)
Conjugated bilirubin remains within hepatocytes (↓MRP2)In order for a patient to have conjugated hyperbilirubinemia this conjugated bilirubin must somehow make it back into the blood.
We need more.
13/
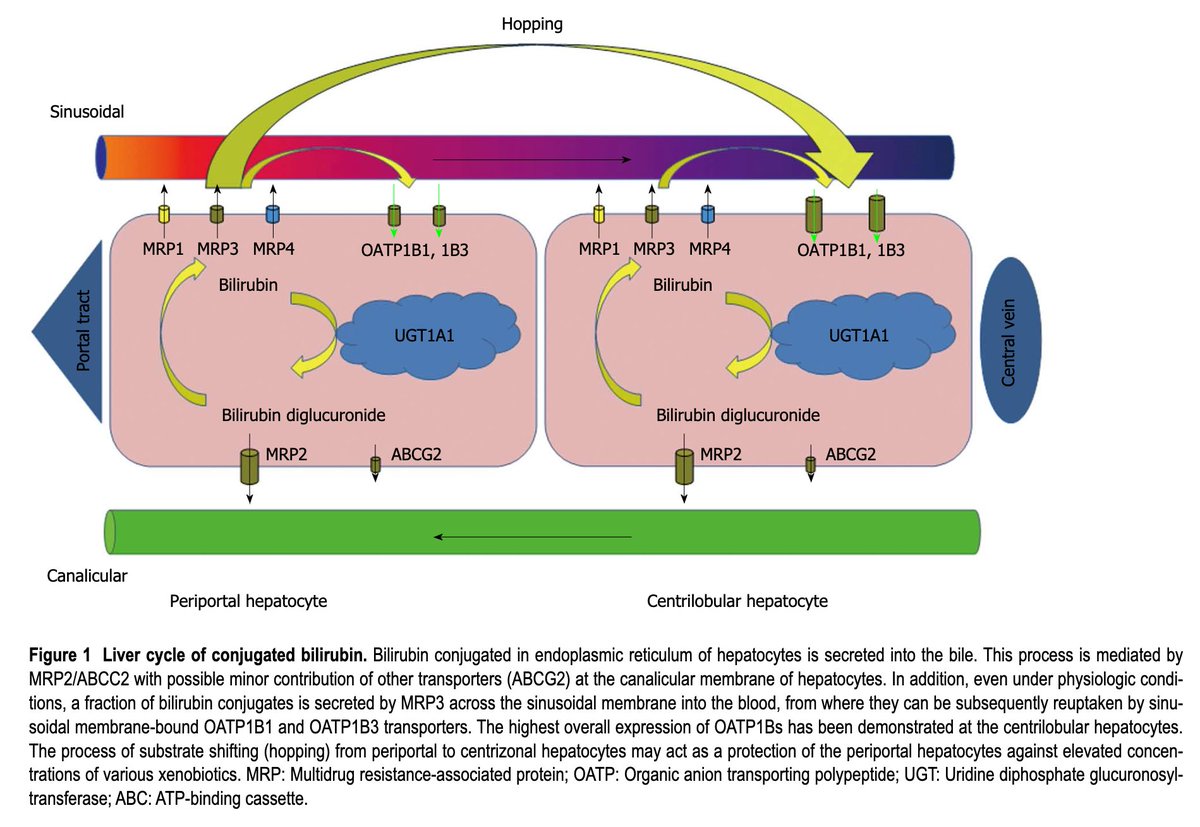
Interestingly, conjugated bilirubin is ROUTINELY secreted back into the sinusoidal blood by MRP3.
It is almost all reclaimed by hepatocytes via organic anion-transporting polypeptides (OATP).
The exact role of this "bilirubin hopping" is not clear.
https://www.ncbi.nlm.nih.gov/pubmed/24151358
Interestingly, conjugated bilirubin is ROUTINELY secreted back into the sinusoidal blood by MRP3.
It is almost all reclaimed by hepatocytes via organic anion-transporting polypeptides (OATP).
The exact role of this "bilirubin hopping" is not clear.
https://www.ncbi.nlm.nih.gov/pubmed/24151358
14/
So, alongside the decrease in the usual portal of exit from the hepatocyte (MRP2) is there is concomitant:
↑MRP3
↓OATP
Thus: secretion and trapping of conjugated bilirubin in the blood
Result: conjugated hyperbilirubinemia!
https://www.ncbi.nlm.nih.gov/pubmed/11774951
So, alongside the decrease in the usual portal of exit from the hepatocyte (MRP2) is there is concomitant:
↑MRP3
↓OATP
Thus: secretion and trapping of conjugated bilirubin in the blood
Result: conjugated hyperbilirubinemia!
https://www.ncbi.nlm.nih.gov/pubmed/11774951
15/15
 UGT1A1 conjugates bilirubin; this remains stable in liver disease
UGT1A1 conjugates bilirubin; this remains stable in liver disease
 MRP2 transports conjugated bilirubin from hepatocytes into bile; this is ↓ in liver disease
MRP2 transports conjugated bilirubin from hepatocytes into bile; this is ↓ in liver disease
 As an alternative exit, conjugated bilirubin enters sinusoidal blood → conjugated hyperbilirubinemia!
As an alternative exit, conjugated bilirubin enters sinusoidal blood → conjugated hyperbilirubinemia!
 UGT1A1 conjugates bilirubin; this remains stable in liver disease
UGT1A1 conjugates bilirubin; this remains stable in liver disease MRP2 transports conjugated bilirubin from hepatocytes into bile; this is ↓ in liver disease
MRP2 transports conjugated bilirubin from hepatocytes into bile; this is ↓ in liver disease As an alternative exit, conjugated bilirubin enters sinusoidal blood → conjugated hyperbilirubinemia!
As an alternative exit, conjugated bilirubin enters sinusoidal blood → conjugated hyperbilirubinemia!
I want to extend a HUGE thank you to...
 Nneka Ufere ( @NnekaUfereMD), GI Fellow, @MGH_GI
Nneka Ufere ( @NnekaUfereMD), GI Fellow, @MGH_GI
 Elliot Tapper ( @ebtapper), Hepatologist, @MichiganLiver
Elliot Tapper ( @ebtapper), Hepatologist, @MichiganLiver
...for their peer review of this tweetorial!
 Nneka Ufere ( @NnekaUfereMD), GI Fellow, @MGH_GI
Nneka Ufere ( @NnekaUfereMD), GI Fellow, @MGH_GI Elliot Tapper ( @ebtapper), Hepatologist, @MichiganLiver
Elliot Tapper ( @ebtapper), Hepatologist, @MichiganLiver...for their peer review of this tweetorial!

 Read on Twitter
Read on Twitter