Nice interview, @sabrinawong88! There are many questions on ideal settings for COVID-19 rapid testing (aka point-of-care tests, aka rapid antigen tests, or RAT, which I’ll use to save characters here). A few thoughts, and yes I will find a way to talk about paid sick days... 1/ https://twitter.com/UBCNursing/status/1362453082320367617
1/ https://twitter.com/UBCNursing/status/1362453082320367617
 1/ https://twitter.com/UBCNursing/status/1362453082320367617
1/ https://twitter.com/UBCNursing/status/1362453082320367617
Right at the top, if you are interested in this topic I would suggest following @VicLeungIDdoc (BC), @LisaBarrettID (NS) and @michaelmina_lab (Harvard Med/School of Public Health). Victor has been a partner and a leader on implementation here in the Vancouver area. /
/
 /
/
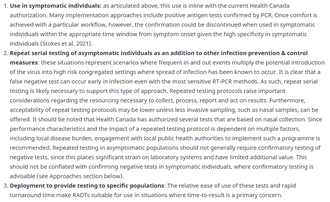
There is also a Health Canada document on the topic: the pithily titled “Interim guidance on the use of rapid antigen detection tests for the identification of SARS-CoV-2 infection” https://bit.ly/3dqgZsB /
With that preamble complete, ‘What are good settings for rapid testing?’ To somewhat simplify a complex question, many major considerations fall into two buckets: risk of onward transmission, and support for the person accessing testing. /
buckets: risk of onward transmission, and support for the person accessing testing. /
 buckets: risk of onward transmission, and support for the person accessing testing. /
buckets: risk of onward transmission, and support for the person accessing testing. /
#1. RISK OF ONWARD TRANSMISSION. A key opportunity offered by RAT is the opportunity to identify people at *the most infectious stage of COVID-19*, and to take immediate action. (Not 12-36h later when a PCR test result comes back, but directly from the site/moment of the test.) /
This can help a person to know their status and isolate sooner, potentially avoiding days of asymptomatic exposure. In VCH we have found LTC staff in outbreaks with no symptoms, who otherwise would have unknowingly worked while infectious that very day. https://twitter.com/VicLeungIDdoc/status/1344805432313872386?s=20 /
Other contexts where risk of transmission is particularly high? Congregate living (shelters, single-room occupancies, prisons, camps, dormitories) – people living or working in these sites can be at high risk of both infection and onward transmission. /
Also, occupations where distancing may not be feasible (due to the nature of the work and/or ‘dynamic’ movements): first responders, construction, manufacturing, food processing, coaching, group learning. (Not an exhaustive list!) Many work types. Which brings us to… /
#2: SUPPORT FOR THE PERSON ACCESSING TESTING. Workers should have sick pay, such that they can isolate at home when sick and access a standard test if necessary, to recover and protect others. /
Without sick pay and a supportive approach to sick leave from the employer, workers are under tremendous pressure to work with symptoms. https://twitter.com/hayman_kate/status/1238596272199614464 /
During contact tracing calls, we already hear that some employers have insisted on staff working with symptoms. (Excuse? ‘They have a mask.’) It would be dangerous to treat a negative rapid test as an added ‘pass’ to insist that sick employees work. /
Job security is likewise important, to avoid the potential impact of employees being terminated if they test positive or choose not to test. /
In the case of a positive test, support for the person testing positive should be adequate to their isolation needs, and may include housing, food support, child care, or funding to address these. Our outreach team works with people this way in Vancouver’s Downtown Eastside... /
…and early on UBC established a program to support campus-dwelling students who test positive. These supports help to make rapid testing feasible—and support infection control since the person tested can isolate safely and successfully. /
There are other auspicious factors for potential RAT implementations. These include engaged site leadership, capacity to manage results (personal health information), and access to confirmatory testing -- and are generally achievable with support from a public health program. /

 Read on Twitter
Read on Twitter