TWEETORIAL and @Blood  :
:
Caplacizumab in TTP has many lessons.
Please RT if you learn something below.
I hope we can have more nuanced discussions about this drug.
Manuscript: https://doi.org/10.1182/blood.2020006052
Commentary by the inspirational Dr. Chaturvedi: https://doi.org/10.1182/blood.2020009250
 :
: Caplacizumab in TTP has many lessons.
Please RT if you learn something below.
I hope we can have more nuanced discussions about this drug.
Manuscript: https://doi.org/10.1182/blood.2020006052
Commentary by the inspirational Dr. Chaturvedi: https://doi.org/10.1182/blood.2020009250
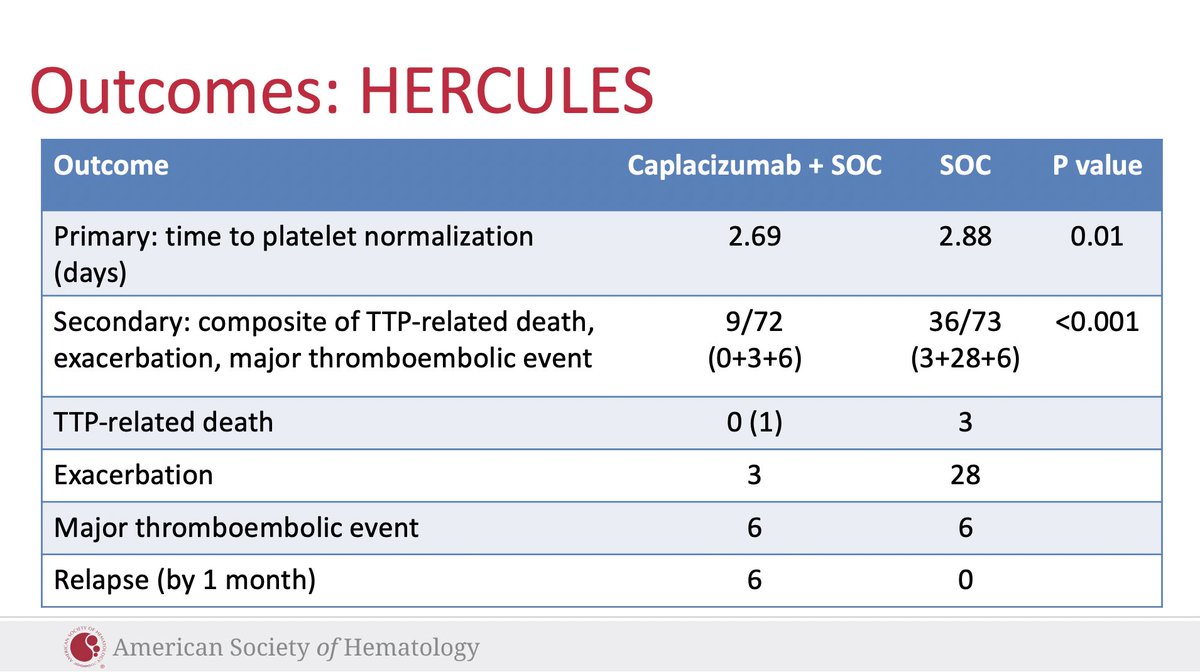
Caplacizumab has taken the #hematology world by storm. It increases the platelet count faster when added to the standard of care (2.69 v 2.88 days; primary outcome) in phase III and improves the secondary composite endpoint, which notably does not include relapse (see below)
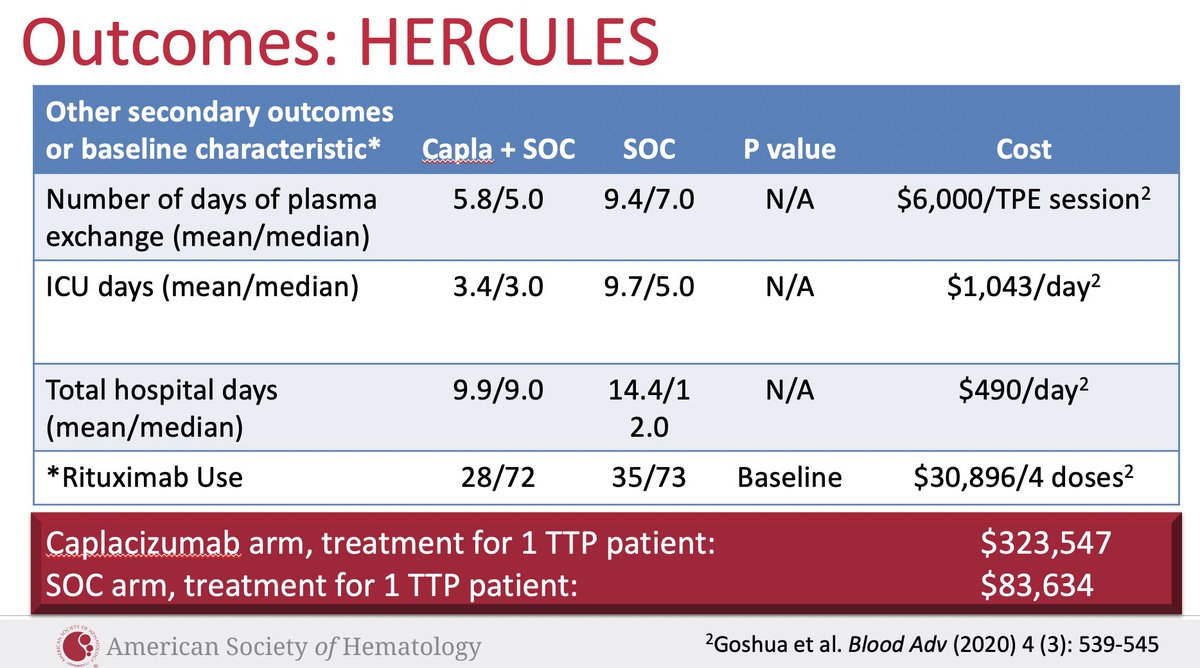
And so patients receive less pheresis and can be discharged sooner. There are cost savings in this on the hospital length of stay, ICU stay, and TPE saved. In turn Sanofi charges $8,000 per daily dose for a med that, at a median, patients received for 35 days.
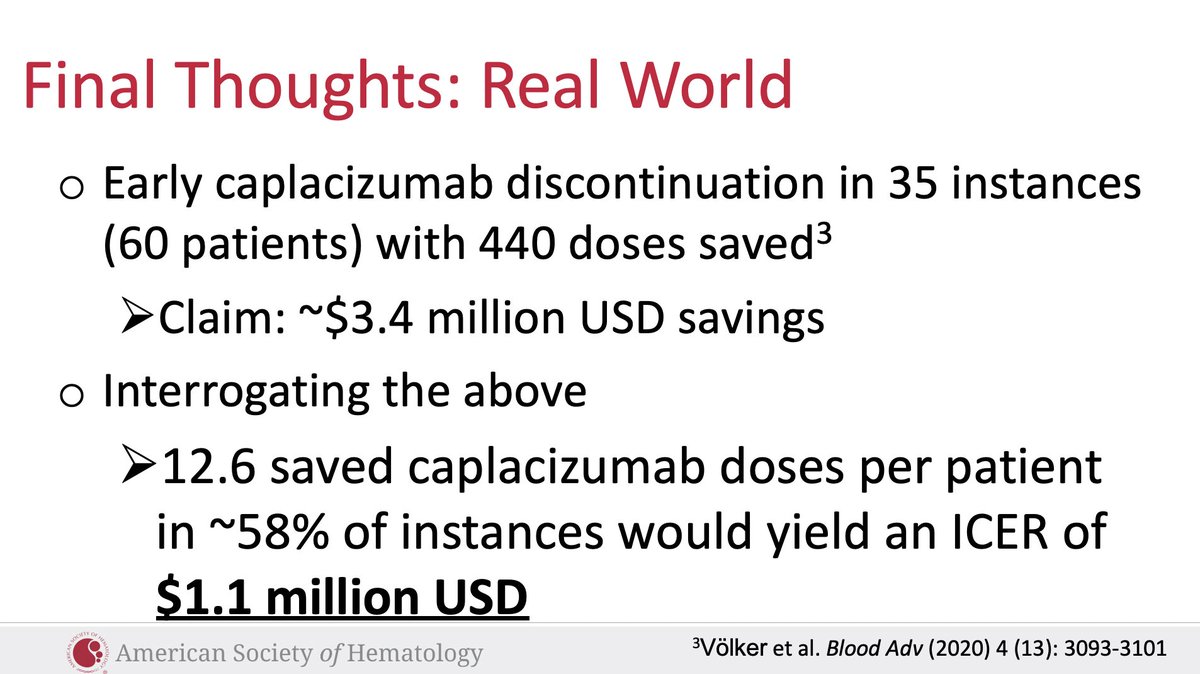
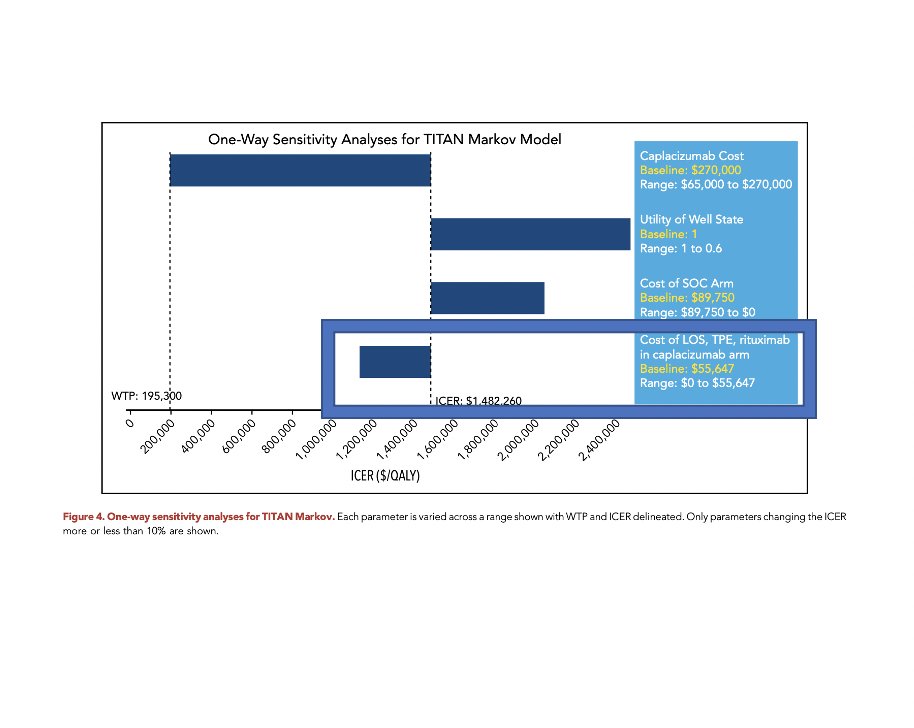
But hey! We can cut down on the amount of capla we use and a German paper reported this cost savings ($3.4 million USD saved) by cutting down to q.o.d dosing. So we interrogated this, turns out the ICER is still north of a million, assuming best case assumptions for caplacizumab.
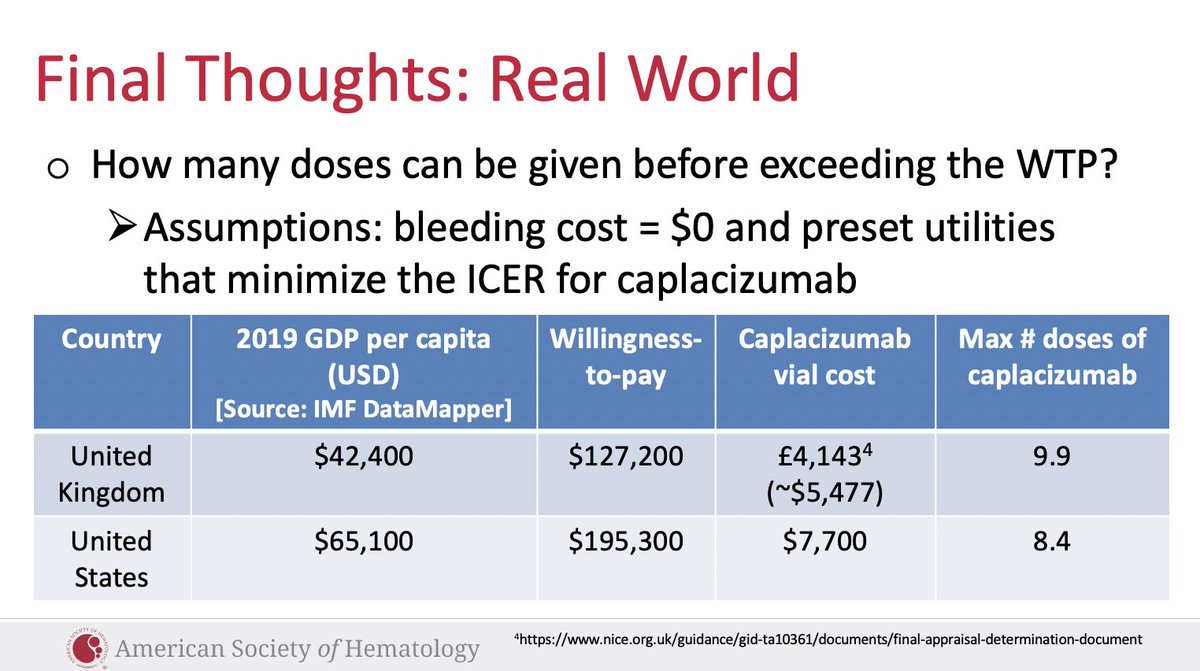
OK well then can we quantify when things start to go broke? Surely we can give some caplacizumab. Yes (the below assumes significant assumptions in favor of caplacizumab yet again):
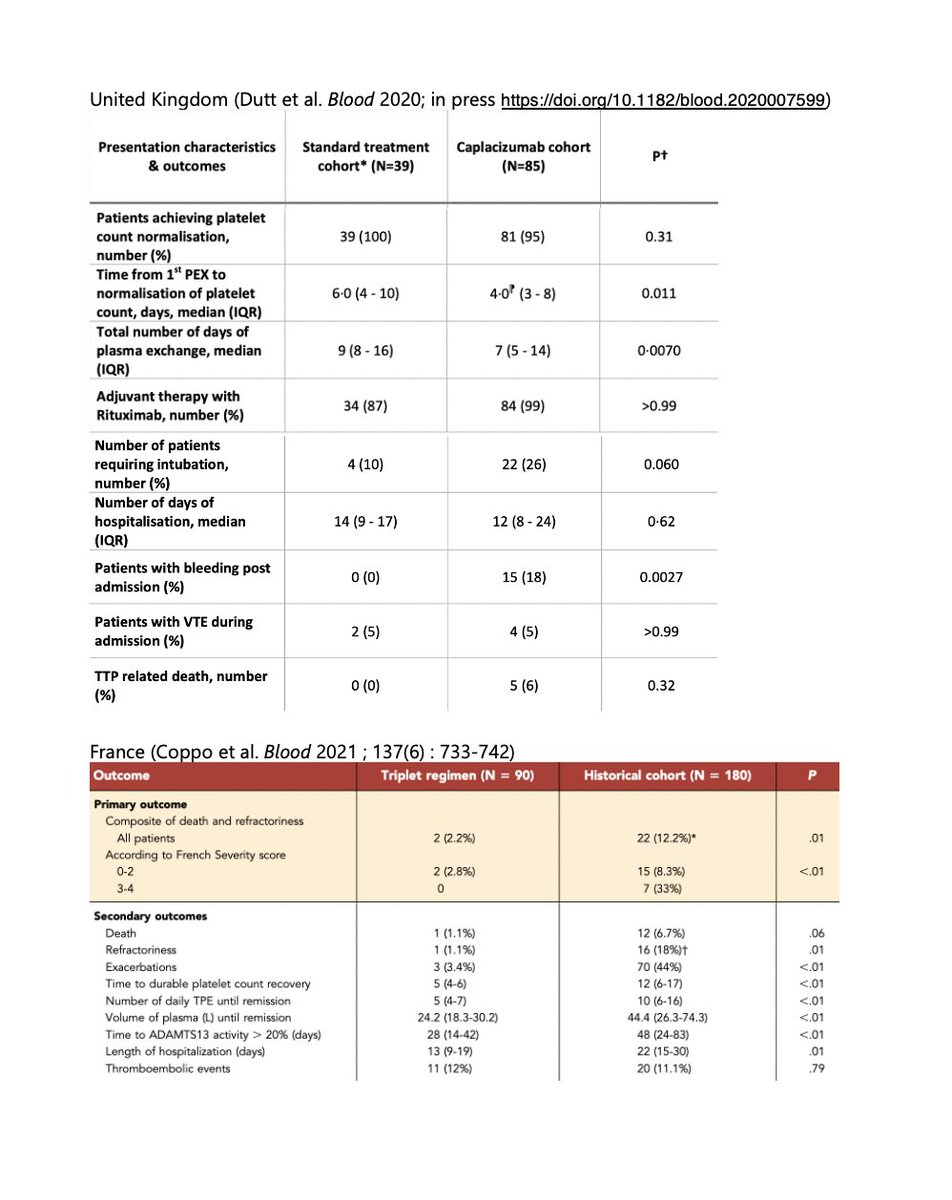
Let’s update this further. The British and French groups both published their observations in Blood comparing caplacizumab added to SOC vs historical cohorts.
An FYI deaths flip arms between the two studies (more with capla in UK, more with historical cohort in France). This is useful commentary on the limitations of comparison using historical cohorts. This said, in rare disease research we often may not have better options.
The field has seen case reports of our Jehovah’s Witness (and other) patients forgoing TPE. The inimitable Dr. James George (pictured below with @johnmatt+I at #ASH 2018) looks forward to a day when we no longer have to perform TPE. We do too. Would *this* be cost effective?
We answered this question in our sensitivity analyses. Answer: no. In a future world where TPE is not performed and there is no hospital stay (treat acute TTP flares as outpatients), caplacizumab is not cost effective.
So what do we do? It can start with the giants in the field advocating for pricing more commensurate with the value of the medication. And the rest of us using the power of the prescription pad + clinical decision making at the bedside on a case by case basis.
Caplacizumab cannot be sustained as frontline therapy for all patients with TTP as currently recommended in @ISTH guidelines. Beyond this, we need to diagnose TTP within 24 hours wherever possible (ie invest in robust and rapid turnaround ADAMTS13 testing,  @joshuamuia).
@joshuamuia).
 @joshuamuia).
@joshuamuia).
Even in the French paper there were 6 patients who received caplacizumab for a couple of days before it turned out their severe thrombocytopenia was not due to TTP. The worst case end result would be major bleeding in a thrombocytopenic patient, induced into an acquired VWD state
What else can we do? We can help our colleagues around the globe. The assumptions Sanofi made in their cost effectiveness analysis that led to NICE’s approval in the UK are publicly available. We have major concerns and a short piece outlining these will be published soon.
Thank you to all inspirations in the field of TTP and hematologist oncologists tackling one problem at a time to help make the system work for all patients. A huge kudos the best colleagues I can wish for in @Pranay_md @Yale_LabMed @ChrisTormey3 #TemBendapudi and #AlfredLee
@guptaarjun90 @ProfMakris @joshuamuia @DrXLongZheng @redcell_doc @heme_fan @acweyand @KaminskiMed @Clotmaster @PishkoMD @VPrasadMDMPH @MarkDSiegel1 @JenniferYuiMD @annap_MD @NTConnell @AMarshallMD @PantepAng @MaryCushmanMD @G_GUPTAMD @davidrosenthal @justine_ryu @jd_beckman
@DevikaDasMD @SonalAPharmD @LisaSandersmd @CatGaoHow @marklewismd @fumikochino @gretchemaben @SSukumarMD @tarsheen2 @amarkelkar @fniainle @Cihan_Ay_MD @xako22 @fredhow @timilpatel @NazliDizman @Jme_os @SorachaWard @tmprowell @HeavnerPharmD @DiMengyang @Dr_AmerZeidan @YaleHemOnc
And @VincentRK your relentless activism and education on this platform surrounding fairer prices in our health system (in hematology oncology and beyond with insulin) is so important for trainees and attendings alike. And most of all for patients.

 Read on Twitter
Read on Twitter