1. The pre-print (not yet peer reviewed) of recent results from our national, community-based CHASING COVID Cohort study of SARS-CoV-2 is out ( http://bit.ly/3arAvmB ). We looked potential risk factors for SARS-CoV-2 infection and public health outcomes. Here are some highlights:
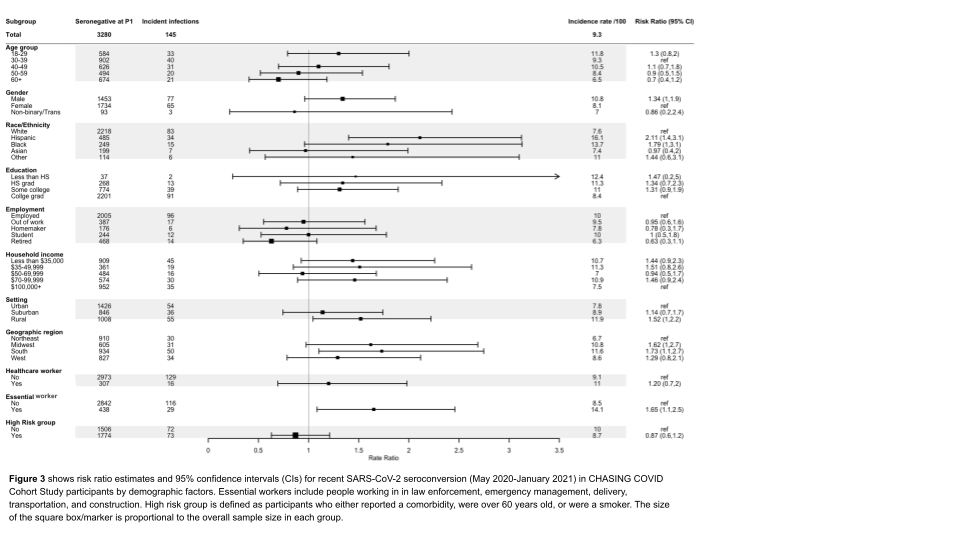
2. We observed 145 seroconversions during May 2020-January 2021 among 3,280 persons who were seronegative during May-August, for an incidence rate of 9.3 per 100 person years (95% CI 7.9-11.0).
3. In this more recent period of the U.S. pandemic, incidence was higher for males than females; among Hispanics and non-Hispanic Blacks compared with non-Hispanic Whites; in rural versus urban areas; in the Midwest, South, and Western US vs. the Northeast.
4. In this more recent period of the pandemic, essential workers had higher incidence than non-essential workers.
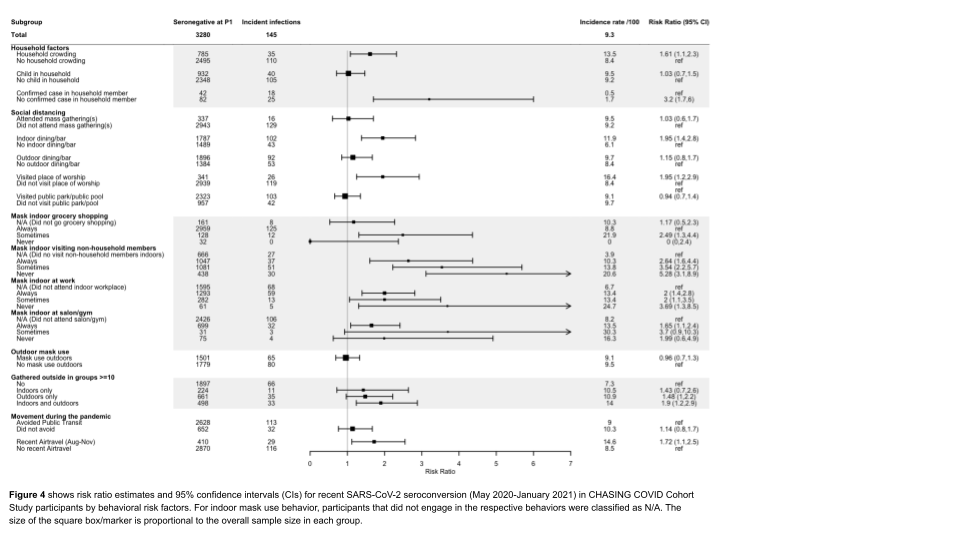
5. We also found several policy-sensitive risk factors to be associated with a higher incidence of recent SARS-CoV-2 seroconversion, including household crowding, visiting places of worship, indoor dining at restaurants and bars; inconsistent mask use while grocery shopping...
6. ...visiting non-household members indoors; attending a salon or gym; working indoors at a place of employment; gathering in groups of 10 or more people; and air travel during the pandemic. We assessed associations for many of these risk factors with and without mask use.
7. In addition to the 145 recent seroconverters, we identified 158 past seroconverters in the first round of serologic testing our cohort in May-August, for a total of 303 persons with serologic evidence of past SARS-CoV-2 infection.
8. During each study interview we queried all participants about symptoms and public health outcomes, like whether they tested, isolated, or were contacted by a contact tracer. 83/303 (27.4%) recalled no symptoms of COVID-like illness (i.e., were likely asymptomatic cases).
9. In terms of public health outcomes, 64.4% (195/303) said that they were tested for SARS-CoV-2 outside the study; However, only half (32% of total) reported having a positive SARS-CoV-2 PCR test.
10. Only 30.7% of the 303 seropositives said that they had isolated themselves from people outside their household because of their infection, and even fewer (13.5% overall) said they isolated themselves from others within their household.
11. In terms of contact tracing, only 17.8% of all seropositives were asked about contacts and 12.2% of all seropositives had been informed by a contact tracer that they may have had contact with someone confirmed to have SARS-CoV-2.
12. Given large proportion with asymptomatic infection, and given the overlap of the pre-symptomatic period with the infectious period of SARS-CoV-2, contact tracing is likely not a viable strategy to control community spread in the US or elsewhere.
13. To be sure, contact tracing has an important role for control of SARS-CoV-2 (e.g., schools, congregate settings), but not to control community spread when the rates are so high. This poor match of strategy with pathogen is dictated by the biology of the SARS-CoV-2 virus.
14. Caveat for our study: We did not control for any potential confounders via multivariate models. Confounders can differ by risk factor... lots more epidemiology to do here.
NB: We report on cumulative incidence for all 303 seropositive participants who seroconverted since the start of the pandemic. Estimates (crude and adjusted for laboratory test error) were 6.8% (95% CI6.1%-7.6%) and 6.3% (95%CI 5.5%-7.1%), respectively. More details in pre-print.
16. A key strength of our study is its prospective design, allowing direct observation of seroconversions and incident SARS-CoV-2 infection among those who had no serologic evidence of prior infection.
17. Key limitations include possible overestimation of causal associations due to uncontrolled confounding for some risk factors, and limited statistical power. More potential limitations covered in discussion section of pre-print.
18. We conclude that modifiable risk factors and poor reach of public health strategies (testing/diagnosis, isolation, contact tracing) are what drives SARS-CoV-2 transmission and inequities across the U.S. today.
19. Thanks for reading this far! I'd like to acknowledge the CHASING COVID Cohort study participants for contributing their time, information, and blood specimens to our study. This work would not be happening without you!
20. I'd also like to acknowledge the amazing CHASING COVID Cohort research team, who launched this national prospective study of nearly 7K participants on March 28th, 2020 and delivered the above results in less than a year! Thanks also to MTL for all that serologic testing!
21. Finally, I'd like to thank our funder @NIH @NIAIDFunding for supporting our work.
@cunyisph @CUNYSPH @CUNY @ETEDashboardNY @iedeaglobal @MonicaGandhi9 @elvingeng @CharlesBHolmes @angie_rasmussen @CarlosdelRio7 @jbkrell
@threadreaderapp unroll

 Read on Twitter
Read on Twitter