Hey @cardionerds! Have you ever been in this situation?
A 60 yo man w/ HTN is incidentally found to have renal artery stenosis (RAS) on imaging. Do we need to call the cath lab? Or is medication the answer?
Check out this #tweetorial on Renal Artery Stenosis to learn more!
A 60 yo man w/ HTN is incidentally found to have renal artery stenosis (RAS) on imaging. Do we need to call the cath lab? Or is medication the answer?
Check out this #tweetorial on Renal Artery Stenosis to learn more!
In this  , we'll cover:
, we'll cover:
1) A primer on RAS pathophysiology
2) The data surrounding revascularization of RAS
3) Current society guidelines on Renal Artery Stenting
 , we'll cover:
, we'll cover: 1) A primer on RAS pathophysiology
2) The data surrounding revascularization of RAS
3) Current society guidelines on Renal Artery Stenting
Poll time!
I feel comfortable with determining which patients may be a candidate for Renal Artery Stenting:
I feel comfortable with determining which patients may be a candidate for Renal Artery Stenting:
Let's start w/ a brief pathophys review!
Atherosclerotic RAS causes renal hypoperfusion. This activates the RAAS system, leading to:
 Renin
Renin
 Angiotensin II (AII)
Angiotensin II (AII)
 SVR
SVR
Remember, RAS is a common cause of secondary HTN!
Atherosclerotic RAS causes renal hypoperfusion. This activates the RAAS system, leading to:
 Renin
Renin Angiotensin II (AII)
Angiotensin II (AII) SVR
SVRRemember, RAS is a common cause of secondary HTN!
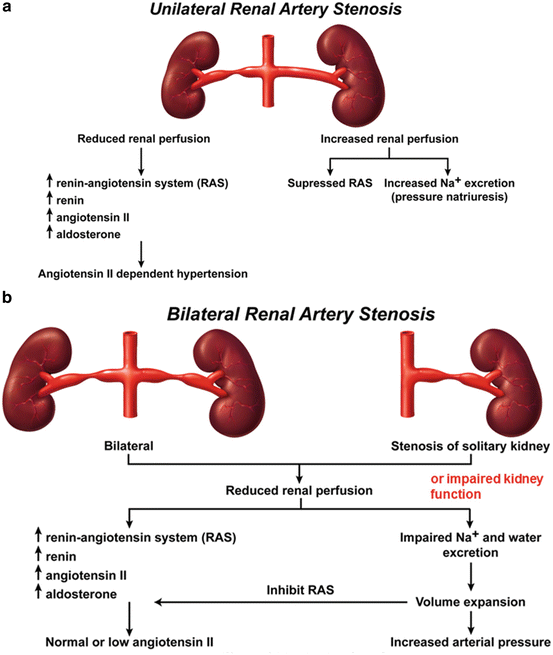
Unilateral RAS leads to HTN via  AII, though increased perfusion of the opposite kidney preserves natriuresis and euvolemia.
AII, though increased perfusion of the opposite kidney preserves natriuresis and euvolemia.
In bilateral RAS, you get volume overload (via natriuresis) and HTN (independent of AII due to relative RAAS inhibition from
natriuresis) and HTN (independent of AII due to relative RAAS inhibition from  volume)!
volume)!
 AII, though increased perfusion of the opposite kidney preserves natriuresis and euvolemia.
AII, though increased perfusion of the opposite kidney preserves natriuresis and euvolemia. In bilateral RAS, you get volume overload (via
 natriuresis) and HTN (independent of AII due to relative RAAS inhibition from
natriuresis) and HTN (independent of AII due to relative RAAS inhibition from  volume)!
volume)!
 PEARL: in b/l RAS, there is decreased flow through the afferent arteriole, & glomerular pressures depend on efferent arteriole constriction via AII.
PEARL: in b/l RAS, there is decreased flow through the afferent arteriole, & glomerular pressures depend on efferent arteriole constriction via AII. If AII is reduced by an ACEi, GFR drops and Crt will


 !
!
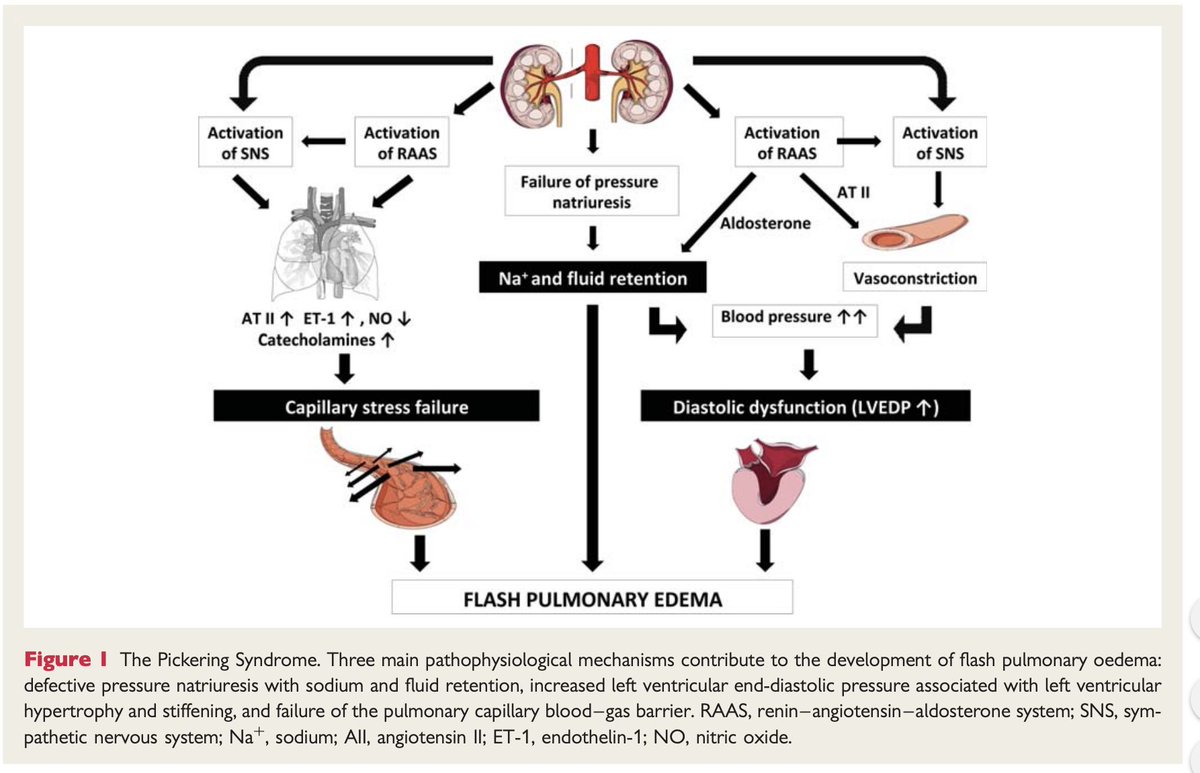
Volume overload and HTN lead to several cardiac destabilizing syndromes, including:
 ACS
ACS
 Decompensated Heart Failure
Decompensated Heart Failure
 Flash Pulmonary Edema/Pickering Syndrome
Flash Pulmonary Edema/Pickering Syndrome
 ACS
ACS  Decompensated Heart Failure
Decompensated Heart Failure  Flash Pulmonary Edema/Pickering Syndrome
Flash Pulmonary Edema/Pickering Syndrome
1st line management in these settings are anti-hypertensives;
However, since the pathology is 2/2 decreased renal perfusion, does improving perfusion via stenting make a difference?
However, since the pathology is 2/2 decreased renal perfusion, does improving perfusion via stenting make a difference?

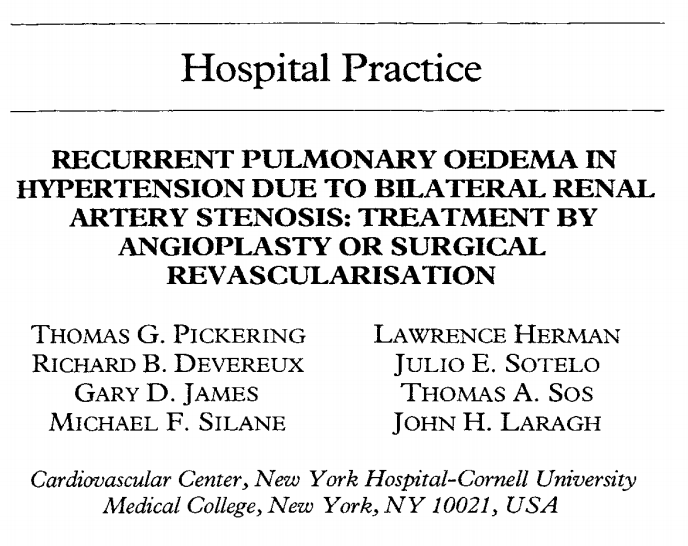
3 Trials of RA stenting v.  : all negative!
: all negative!
 STAR: 140 pts w/CrCl ≤80, RAS ≥ 50%, but controlled BP
STAR: 140 pts w/CrCl ≤80, RAS ≥ 50%, but controlled BP
 ASTRAL: 806 pts w/RAS+clinical dz (HTN, Kidney Dz) where potential clinical benefit of stenting was unclear
ASTRAL: 806 pts w/RAS+clinical dz (HTN, Kidney Dz) where potential clinical benefit of stenting was unclear
 CORAL: 948 pts with RAS 60-100%, HTN on ≥ 2 drugs or GFR<60
CORAL: 948 pts with RAS 60-100%, HTN on ≥ 2 drugs or GFR<60
 : all negative!
: all negative! STAR: 140 pts w/CrCl ≤80, RAS ≥ 50%, but controlled BP
STAR: 140 pts w/CrCl ≤80, RAS ≥ 50%, but controlled BP ASTRAL: 806 pts w/RAS+clinical dz (HTN, Kidney Dz) where potential clinical benefit of stenting was unclear
ASTRAL: 806 pts w/RAS+clinical dz (HTN, Kidney Dz) where potential clinical benefit of stenting was unclear CORAL: 948 pts with RAS 60-100%, HTN on ≥ 2 drugs or GFR<60
CORAL: 948 pts with RAS 60-100%, HTN on ≥ 2 drugs or GFR<60
However! These trials may have under-represented pts with very severe, hemodynamically significant stenoses. How do we identify these pts?
This review by @MPrinceMD suggests trans-lesional pressure gradients can confirm hemodynamic significance, and aid in patient selection.
This review by @MPrinceMD suggests trans-lesional pressure gradients can confirm hemodynamic significance, and aid in patient selection.
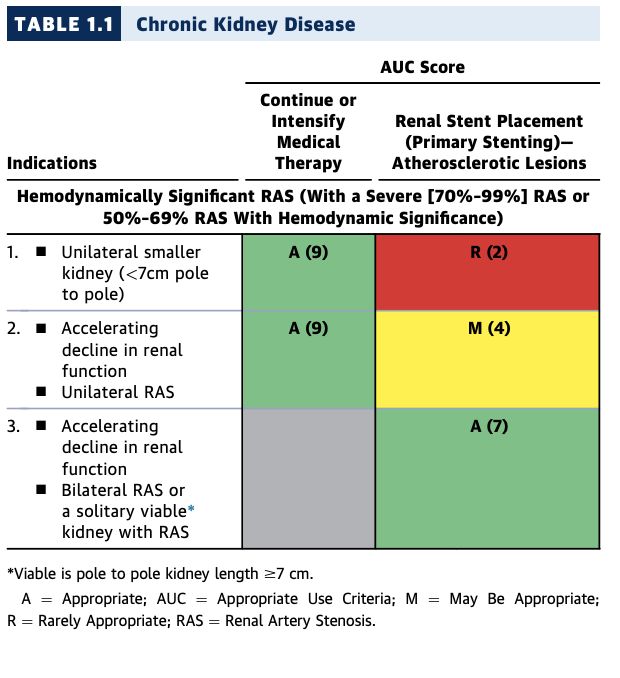
Given the controversy, what are the current guidelines on RAS revascularization?
Current AHA/ACC appropriate use criteria (AUC) list the following indications for revascularization of hemodynamically significant RAS:
Current AHA/ACC appropriate use criteria (AUC) list the following indications for revascularization of hemodynamically significant RAS:
 Accelerating
Accelerating  in renal function in b/l RAS (or RAS of solitary kidney)
in renal function in b/l RAS (or RAS of solitary kidney) Failure to control BP despite max doses of 3 agents (including a diuretic)
Failure to control BP despite max doses of 3 agents (including a diuretic) Recurrent heart failure despite max medical therapy
Recurrent heart failure despite max medical therapy  Sudden pulmonary edema
Sudden pulmonary edema Uncontrolled UA despite max medical therapy
Uncontrolled UA despite max medical therapy
Lets summarize!
 RAS
RAS 
 destabilization syndromes via
destabilization syndromes via  BP ±
BP ±  volume
volume
 Current data shows
Current data shows  benefit for RAS stenting, though lacks physiologic assessment
benefit for RAS stenting, though lacks physiologic assessment
 AUC support stenting in settings of hemodynamically significant RAS, including
AUC support stenting in settings of hemodynamically significant RAS, including  destabilization, resistant HTN, CKD
destabilization, resistant HTN, CKD
 RAS
RAS 
 destabilization syndromes via
destabilization syndromes via  BP ±
BP ±  volume
volume Current data shows
Current data shows  benefit for RAS stenting, though lacks physiologic assessment
benefit for RAS stenting, though lacks physiologic assessment AUC support stenting in settings of hemodynamically significant RAS, including
AUC support stenting in settings of hemodynamically significant RAS, including  destabilization, resistant HTN, CKD
destabilization, resistant HTN, CKD
Poll Time, part 2!
I feel comfortable with determining which patients may be a candidate for Renal Artery Stenting:
I feel comfortable with determining which patients may be a candidate for Renal Artery Stenting:
I learned something in this Tweetorial that may change my clinical practice.
This is the tip of the iceberg of renovascular hypertension! Much more could be said about RAS due to fibromuscular dysplasia (which typically DOES respond to revascularization), methods of determining RAS physiologic significance, and renal denervation!
As always, big thanks to the @cardionerds team (especially @AmitGoyalMD and @karanpdesai) for their assistance in this #tweetorial; any and all feedback or thoughts are appreciated!

 Read on Twitter
Read on Twitter