Pts w/ contralateral carotid occlusion (CCO) are high-risk for carotid revasc. How does CCO impact outcomes for undergoing carotid artery stenting (CAS) vs CEA?
Check out our paper http://bit.ly/3tZCTJ7 in @JACCJournals and Tweetorial ! @EricSecemskyMD
! @EricSecemskyMD
Check out our paper http://bit.ly/3tZCTJ7 in @JACCJournals and Tweetorial
 ! @EricSecemskyMD
! @EricSecemskyMD
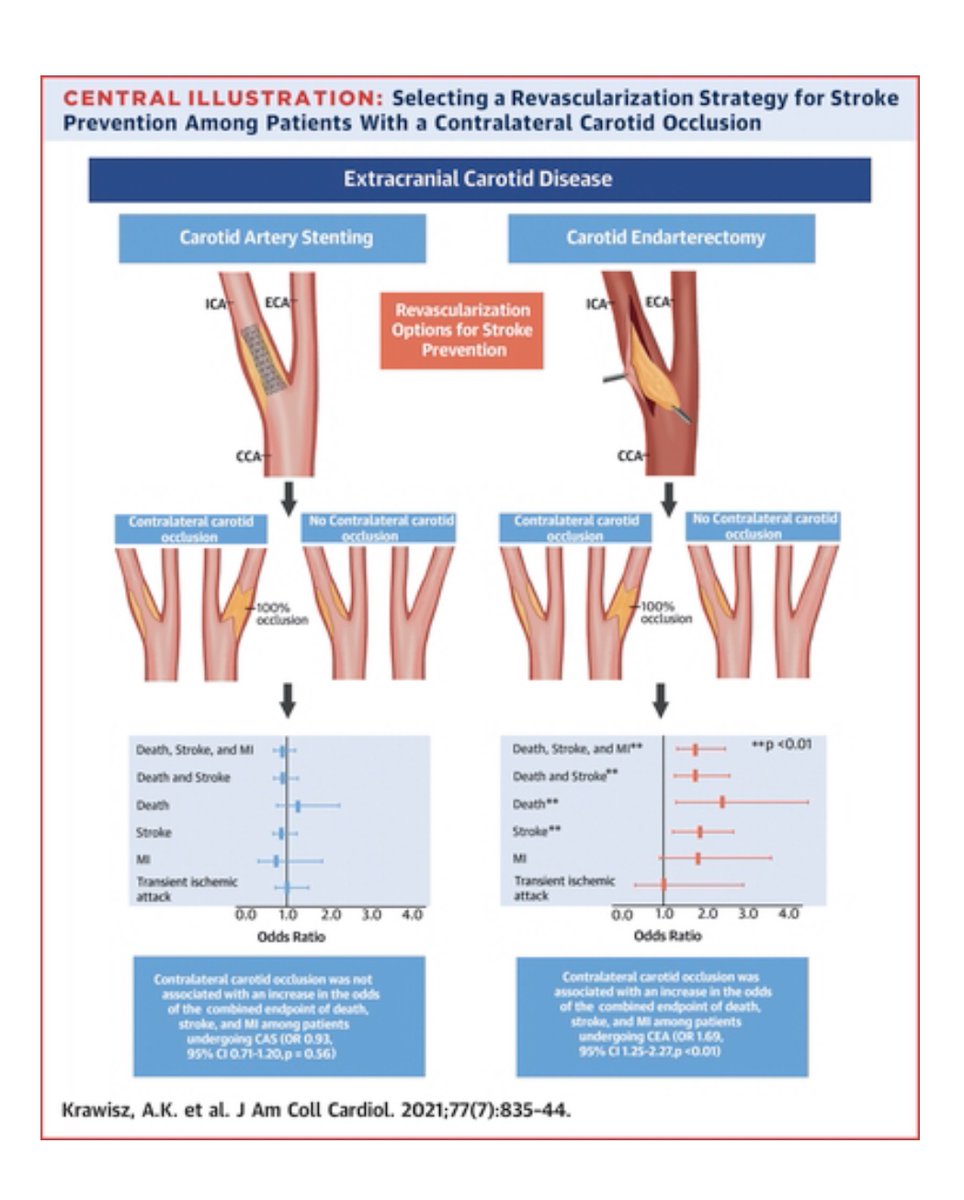
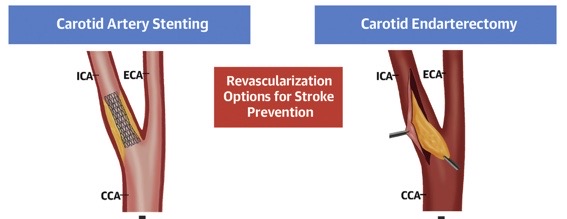
CCO is traditionally a high-risk feature for CEA and a reason to refer patients for CAS. Recent observational data contradicts this and suggests that CCO should no longer be considered high-risk for CEA in contemporary practice.
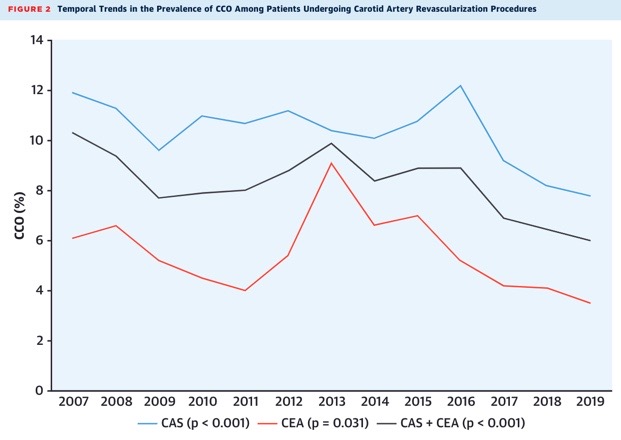
First, we found a significant decline (by 42%) in the prevalence of CCO among patients undergoing CAS + CEA from 2007-2019.
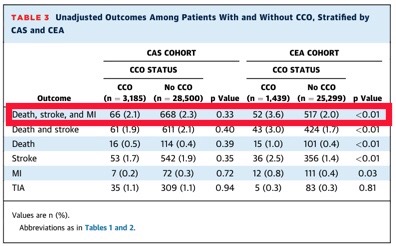
Second, we found that unadjusted rates of the composite endpoint of death, stroke, and MI were higher in patients with CCO who underwent CEA (3.6%) than patients with CCO who underwent CAS (2.1%).
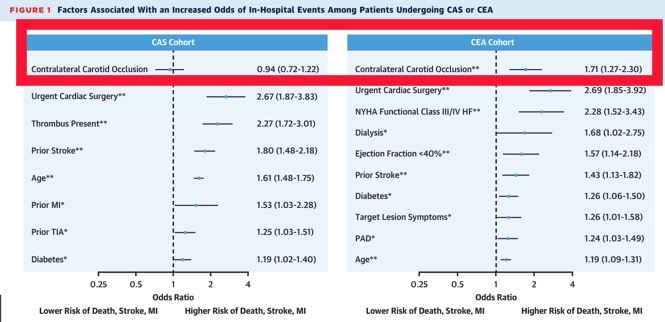
Third, after multivariable regression, CCO was assoc w/ 71%  in odds of death/stroke/MI in pts undergoing CEA (95% CI 1.27-2.30, p<0.01), but was not assoc with an
in odds of death/stroke/MI in pts undergoing CEA (95% CI 1.27-2.30, p<0.01), but was not assoc with an  in odds of adverse events for patients undergoing CAS.
in odds of adverse events for patients undergoing CAS.
 in odds of death/stroke/MI in pts undergoing CEA (95% CI 1.27-2.30, p<0.01), but was not assoc with an
in odds of death/stroke/MI in pts undergoing CEA (95% CI 1.27-2.30, p<0.01), but was not assoc with an  in odds of adverse events for patients undergoing CAS.
in odds of adverse events for patients undergoing CAS.
Fourth, after inverse-probability of treatment weighting, CCO was assoc w/ an  in odds of death/stroke/MI in pts undergoing CEA (red) (OR 1.69, 95% CI 1.25-2.27, p<0.01), but was not assoc w/ an
in odds of death/stroke/MI in pts undergoing CEA (red) (OR 1.69, 95% CI 1.25-2.27, p<0.01), but was not assoc w/ an  in odds of adverse events for pts undergoing CAS (blue).
in odds of adverse events for pts undergoing CAS (blue).
 in odds of death/stroke/MI in pts undergoing CEA (red) (OR 1.69, 95% CI 1.25-2.27, p<0.01), but was not assoc w/ an
in odds of death/stroke/MI in pts undergoing CEA (red) (OR 1.69, 95% CI 1.25-2.27, p<0.01), but was not assoc w/ an  in odds of adverse events for pts undergoing CAS (blue).
in odds of adverse events for pts undergoing CAS (blue).
Fifth, signif variation exists among centers in revasc of pts w/ CCO: MOR of 1.71 (95% CI: 1.59-1.82) for likelihood of having CCO in pts who underwent CAS; MOR of 2.01 (95% CI: 1.76-2.25) for likelihood of having CCO in patients who underwent CEA
Conclusion: CCO remains an important predictor of increased risk among patients undergoing CEA, but not CAS.
Thank you very much for the support of my amazing mentor @EricSecemskyMD and everyone at @SmithBIDMC!
Thank you very much for the support of my amazing mentor @EricSecemskyMD and everyone at @SmithBIDMC!

 Read on Twitter
Read on Twitter