Women and men have the same risk factors for CVD, right? WRONG!



Keep reading for a tweetorial on CVD in women!
@erinmichos @drmarthagulati @cardiopcimom @gina_lundberg @KBerlacher @shreyarao87 @DrLaxmiMehta @MinnowWalsh @MedTweetorials



Keep reading for a tweetorial on CVD in women!
@erinmichos @drmarthagulati @cardiopcimom @gina_lundberg @KBerlacher @shreyarao87 @DrLaxmiMehta @MinnowWalsh @MedTweetorials
What have we learned about women's CVD disease since 1966?
In light of #wearredday celebrating #WIC, we will explore:
celebrating #WIC, we will explore:
(1) the traditional ASCVD risk score
(2) female-specific ASCVD risk-enhancers
(3) female-predominant ASCVD risk-enhancers
In light of #wearredday
 celebrating #WIC, we will explore:
celebrating #WIC, we will explore:(1) the traditional ASCVD risk score
(2) female-specific ASCVD risk-enhancers
(3) female-predominant ASCVD risk-enhancers
Poll -
I feel comfortable identifying female-specific and –predominant factors that may modify our assessment of an individual's lifetime ASCVD risk.
I feel comfortable identifying female-specific and –predominant factors that may modify our assessment of an individual's lifetime ASCVD risk.
To guide individual prevention recs, we use the Pooled Cohort Equations that  Atherosclerotic Cardiovascular Disease (ASCVD) Risk Score.
Atherosclerotic Cardiovascular Disease (ASCVD) Risk Score.
Using the exact same PMHx, SBP, cholesterol, and smoking history, you get a different risk assessment for men and women.
 Atherosclerotic Cardiovascular Disease (ASCVD) Risk Score.
Atherosclerotic Cardiovascular Disease (ASCVD) Risk Score. Using the exact same PMHx, SBP, cholesterol, and smoking history, you get a different risk assessment for men and women.
But do these factors fully capture our patient's risk? What else should we consider? Let's review the guidelines! 

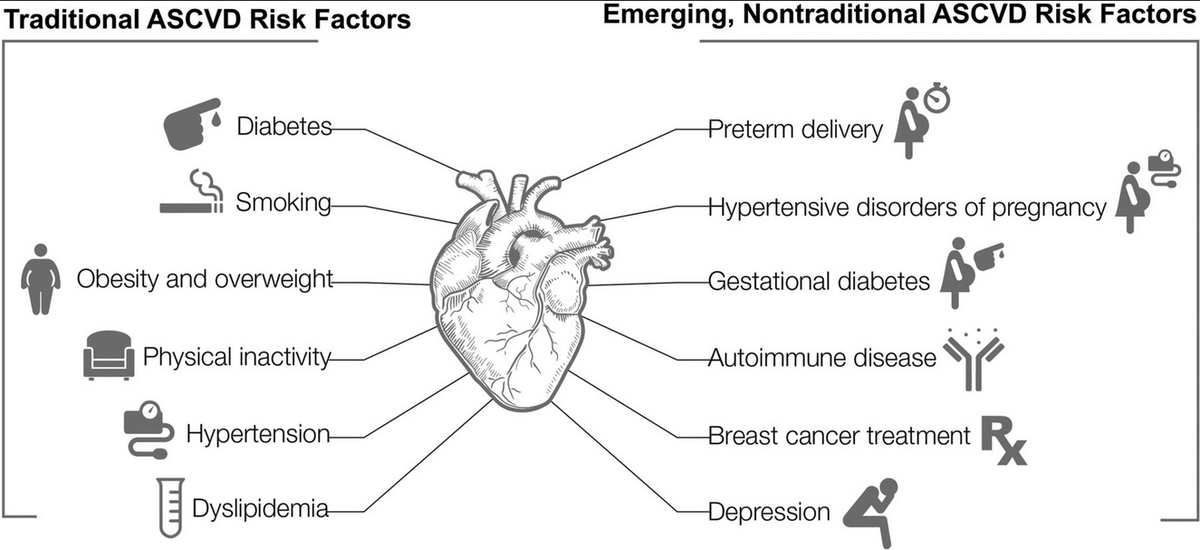
New in 2019, the ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease called for physicians to consider RISK-ENHANCING FACTORS specific to women.
So what are some of these risk-enhancers? https://www.sciencedirect.com/science/article/pii/S073510971933877X?via%3Dihub
So what are some of these risk-enhancers? https://www.sciencedirect.com/science/article/pii/S073510971933877X?via%3Dihub
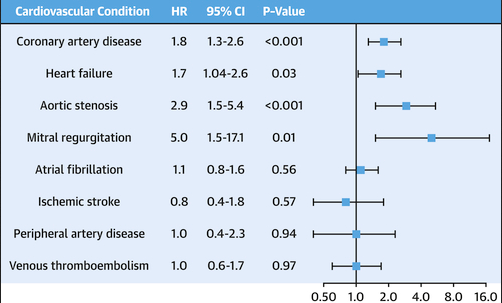
Let's start with gestational hypertension and preeclampsia. In this study, preeclampsia was assc with a HR of 1.8 for incidence of CAD vs those w/o preeclampsia.
Thought due to accelerated cardiovascular aging and persistent arterial stiffness
https://www.jacc.org/cms/asset/1d0d8a4c-99a6-4f48-a55f-c6ec219999ec/gr3.jpg
Thought due to accelerated cardiovascular aging and persistent arterial stiffness
https://www.jacc.org/cms/asset/1d0d8a4c-99a6-4f48-a55f-c6ec219999ec/gr3.jpg
Keep in mind, hypertensive disorders in pregnancy are not only associated with increased incidence of CAD but also other cardiovascular conditions including valvular disease and heart failure -- NOT entirely mediated by ongoing chronic hypertension
https://www.cardionerds.com/66-case-report-severe-pre-eclampsia-cardio-obstetrics-upmc/
https://www.cardionerds.com/66-case-report-severe-pre-eclampsia-cardio-obstetrics-upmc/
Other pregnancy related risk-enhancers = preterm delivery ( <37 weeks +
<37 weeks + 
 <32 weeks) and small for gestational size infants.
<32 weeks) and small for gestational size infants.
 <37 weeks +
<37 weeks + 
 <32 weeks) and small for gestational size infants.
<32 weeks) and small for gestational size infants.
Pathophys still not clear – but thought due to
1) systemic inflammation
2) vascular disease
3) dysregulation in cardiometabolic factors. https://www.ahajournals.org/doi/full/10.1161/JAHA.117.007809#:~:text=Preterm%20delivery%20is%20associated%20with,cardiovascular%20risk%20assessment%20in%20women
1) systemic inflammation
2) vascular disease
3) dysregulation in cardiometabolic factors. https://www.ahajournals.org/doi/full/10.1161/JAHA.117.007809#:~:text=Preterm%20delivery%20is%20associated%20with,cardiovascular%20risk%20assessment%20in%20women
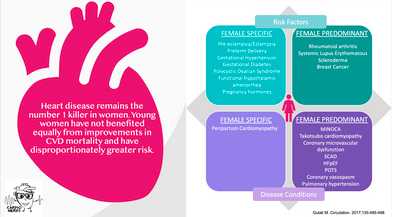
Inflammatory + autoimmune conditions that largely affect women AND confer  CVD risk include:
CVD risk include:
-rheumatoid arthritis
-scleroderma
-SLE
Related to underlying inflammation + oxidative stress, as well as treatments (I.e. steroids)
…https://pubmed-ncbi-nlm-nih-gov.ucsf.idm.oclc.org/29685876/#&gid=article-figures&pid=fig-3-uid-2
 CVD risk include:
CVD risk include: -rheumatoid arthritis
-scleroderma
-SLE
Related to underlying inflammation + oxidative stress, as well as treatments (I.e. steroids)
…https://pubmed-ncbi-nlm-nih-gov.ucsf.idm.oclc.org/29685876/#&gid=article-figures&pid=fig-3-uid-2
Early menopause also confers an increased risk of coronary artery disease.
Despite the risk, remember that the Women's Health Initiative did NOT show that HRT is cardioprotective
risk, remember that the Women's Health Initiative did NOT show that HRT is cardioprotective
Despite the
 risk, remember that the Women's Health Initiative did NOT show that HRT is cardioprotective
risk, remember that the Women's Health Initiative did NOT show that HRT is cardioprotective
A good obstetrics history is critical to accurately assessing CV risk! Make sure to ask about PCOS, OCP use, hormone replacement therapy, and oncologic history including history of breast cancer +/- treatment
https://www.ahajournals.org/cms/asset/7d5fc228-477a-4196-91c8-d3e00c0a893e/1273fig01.jpeg
https://www.ahajournals.org/cms/asset/7d5fc228-477a-4196-91c8-d3e00c0a893e/1273fig01.jpeg
In summary, in light of #wearredday  , let's remember to screen women for female-specific and female-predominant conditions that may modify CVD risk and are not included in the PCE!
, let's remember to screen women for female-specific and female-predominant conditions that may modify CVD risk and are not included in the PCE!
For applied cases, see expert discussion by @DrMarthaGulati here -
https://www.cardionerds.com/18-womens-cardiovascular-health-with-dr-martha-gulati/
 , let's remember to screen women for female-specific and female-predominant conditions that may modify CVD risk and are not included in the PCE!
, let's remember to screen women for female-specific and female-predominant conditions that may modify CVD risk and are not included in the PCE! For applied cases, see expert discussion by @DrMarthaGulati here -
https://www.cardionerds.com/18-womens-cardiovascular-health-with-dr-martha-gulati/
Poll:
I feel comfortable identifying female-specific and –predominant factors that may modify our assessment of an individual's lifetime ASCVD risk.
I feel comfortable identifying female-specific and –predominant factors that may modify our assessment of an individual's lifetime ASCVD risk.
I learned something in this Tweetorial that may change my clinical practice.
Thanks for reading! Would love to hear any thoughts and feedback.
As always, thank you to the @cardionerds family for support and feedback – particularly @ThomasMDas!
As always, thank you to the @cardionerds family for support and feedback – particularly @ThomasMDas!
To learn more about women's CV health, click  to hear from experts @drmarthagulati, Dr. Leslie Cho, + Dr. Nanette Wenger
to hear from experts @drmarthagulati, Dr. Leslie Cho, + Dr. Nanette Wenger
https://www.cardionerds.com/episodes/womens-cv-health/
@amitgoyalmd @dr_danmd @carinehamo @karanpdesai
@justinberk @EuniceDuganMD @RichardAFerraro @CBlumenthal2 @EvelynSongMD
 to hear from experts @drmarthagulati, Dr. Leslie Cho, + Dr. Nanette Wenger
to hear from experts @drmarthagulati, Dr. Leslie Cho, + Dr. Nanette Wenger https://www.cardionerds.com/episodes/womens-cv-health/
@amitgoyalmd @dr_danmd @carinehamo @karanpdesai
@justinberk @EuniceDuganMD @RichardAFerraro @CBlumenthal2 @EvelynSongMD

 Read on Twitter
Read on Twitter