One group who deserve more recognition for their efforts over the past year are those doctors who work in the health service but are neither trainees or consultants (non-training speciality doctors, or NTSDs, as the HSE calls them).
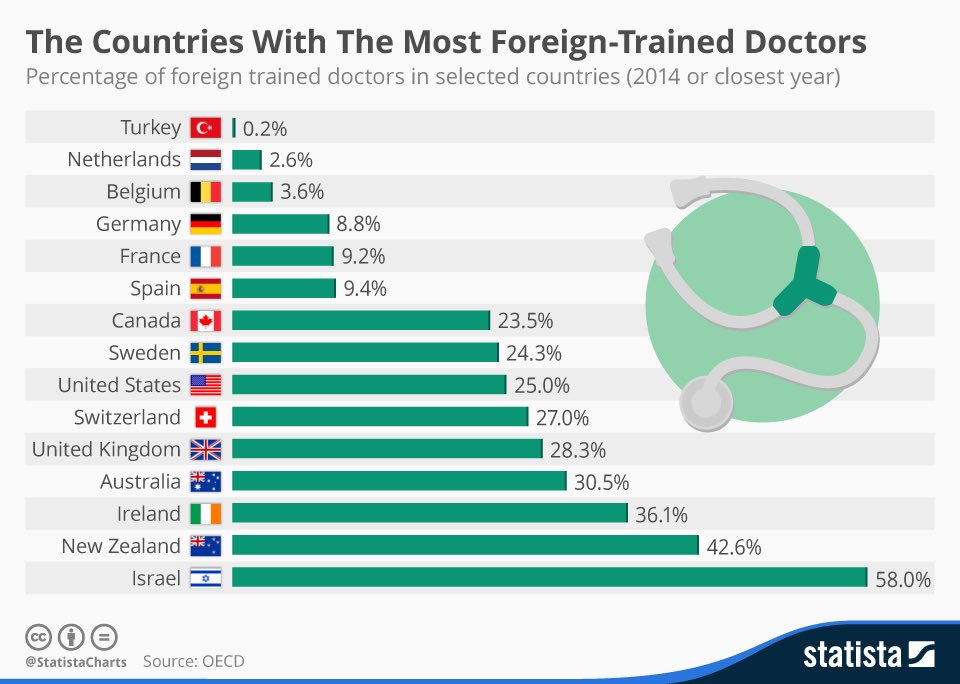
This group is overwhelmingly from outside of Ireland, mostly from low- and middle-income countries, and we are dependent on them to staff our health service.
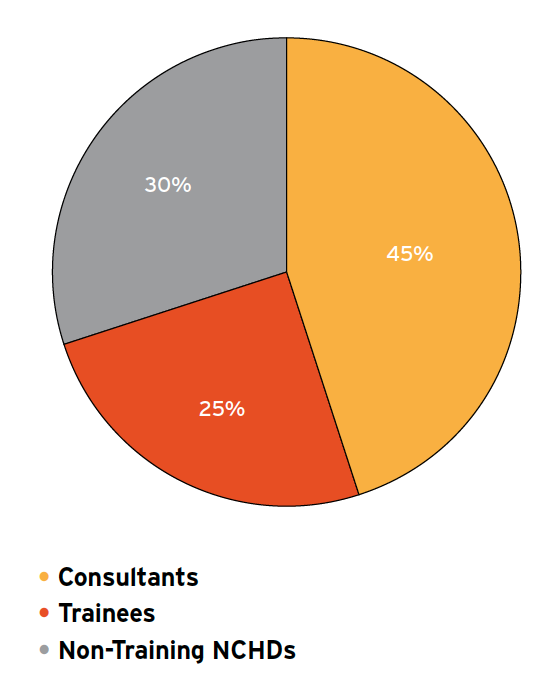
While reliable figures are hard to come by, in anaesthesia alone 30% of doctors in the speciality fall into this group. They are essential to providing anaesthesia and critical care around Ireland, and staff onerous on-call and out-of-hours rosters.
However, we treat this group poorly. Doctors from outside the EU are automatically ranked below ones from the EU when applying for places on our recognised speciality training schemes. As a result, even excellent doctors from outside the EU cannot enter a training programme
Unsurprisingly, that means career development prospects for this group - the hope of becoming a consultant, for instance - are limited. Thus, it is no surprise that we lose many excellent doctors from abroad to more welcoming countries like the US or UK.
What is also means is that those who remain are relegated to working in undesirable locations in undesirable jobs and outside the remit of a training body (other than the CPD-SS required by the medical council). It’s not their fault, we bear responsibility for not training them.
This is not a new issue. In fact, it was one of the key issues highlighted by the MacCraith Report in 2013 to the Department of Health. https://www.gov.ie/en/collection/9ef920-strategic-review-of-medical-training-and-career-structure-maccraith-/
In 2014, the National Clinical Programme for Anaesthesia published a report which also recognised the challenges facing this group, and the challenges to the health service from over-reliance on this group for out-of-hours and on-call cover in particular: https://www.hse.ie/eng/services/publications/clinical-strategy-and-programmes/providing-quality-safe-and-comprehensive-anaesthesia-services-ireland.pdf
However, this group of non-training doctors faces challenges beyond barriers to training. They face an interminable wait for citizenship, punctuated by 6-monthly visits to the GNIB and other hurdles.
Their employment status is precarious. They are reliant on fixed-term contracts, typically of 6 or 12 month duration. Hospitals are careful to ensure that they cannot be granted contracts of indefinite duration, by not renewing these contracts.
Thus, even though they may have dedicated years working in the health service, they are often denied permanent status by their employers (because each hospital is a different employer, even if the money all comes from the same place), and so have very little job security.
Our health service, and our anaesthesia and critical care departments especially, was kept afloat over the past year by this group of doctors. However, we treat them poorly: no training, no career progression, no citizenship, no job security.
I think we owe it to these doctors to treat them with the respect they deserve, not just because of Covid, but the pandemic could provide the catalyst for change. All (or most) NCHD posts should be training posts. Citizenship should be granted. Secure employment should be a given
And we should seek a solution for the thorniest issue: how to provide out-of-hours service without relying on NTSDs? Post-Covid, this will remain one of the biggest issue facing our profession, and we can't continue to kick the can down the road as we have since the Hanly report

 Read on Twitter
Read on Twitter