1) Only measure lipase once!
2) Diagnosis:
2 out of three:
1) Lipase >3xUNL
2) typical belted abdominal pain
3) typical image of pancreatitis in CT or sono
2 out of three:
1) Lipase >3xUNL
2) typical belted abdominal pain
3) typical image of pancreatitis in CT or sono
3) Why meassure lipase only once?
4) If the lipase increases, it provides no further information. If it decreases neither. It does not show that it gets better. Maybe the pancreas is so destroyed, that it can’t produce it anymore.
Be aware: Normal lipase in acute on chronic pancreatitis possible!
Be aware: Normal lipase in acute on chronic pancreatitis possible!
5) Imaging
6) Typical signs of acute pancreatitis appear after days. No need for a fast pancreas image.
But ultrasound to look for a biliary cause!
But ultrasound to look for a biliary cause!
7) Differential diagnoses: MI, cholangitis, cholecystitis, choledicholithiasis, ulcus, perforation, mesenterial ischemia, hepatitis intestinal obstruction
8) Etiology
9) I GET SMASHED
Idiopathic
Gallstones
Ethanol
Trauma
Steroids
Mumps
Autoimmun
Scorpion Venom
Hypercalzemia, Hypertryglyceridemia
ERCP
Drugs
(COVID-19?)
Idiopathic
Gallstones
Ethanol
Trauma
Steroids
Mumps
Autoimmun
Scorpion Venom
Hypercalzemia, Hypertryglyceridemia
ERCP
Drugs
(COVID-19?)
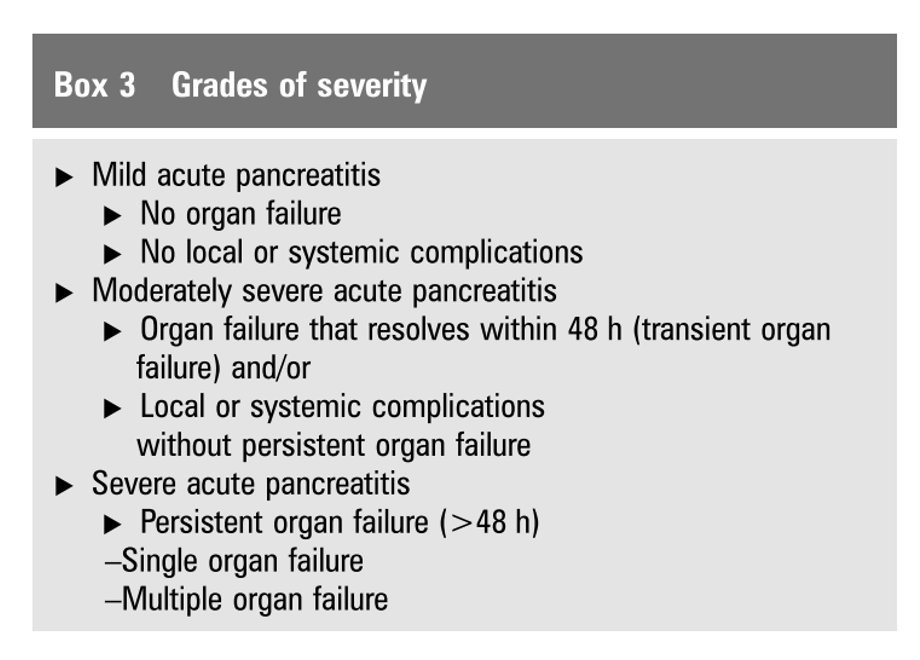
11) Prognosis
12)Severe:
Urea > 25mg/dl (admission/first 24 hours)
CRP>150 mg/dl
SIRS
Hypocalzemia
Mild:
Normoglykemia
Normal haematocrit (<44%)
Urea > 25mg/dl (admission/first 24 hours)
CRP>150 mg/dl
SIRS
Hypocalzemia
Mild:
Normoglykemia
Normal haematocrit (<44%)
13) Scores:
-BISAP (Bedside Index for Severity in Acute Pancreatitis)
-Ranson-Kriterien
-Harmless Acute Pankcreatitis Score
-BISAP (Bedside Index for Severity in Acute Pancreatitis)
-Ranson-Kriterien
-Harmless Acute Pankcreatitis Score
14) Therapy
15)
3 (-4) modules:
1) Fluids
2) Analgesia
3)Nutrition (!)
4) ERCP
Usually no antibiotics, it's a sterile inflammation primary!
3 (-4) modules:
1) Fluids
2) Analgesia
3)Nutrition (!)
4) ERCP
Usually no antibiotics, it's a sterile inflammation primary!
16) Fluids
controlled and target-oriented
200-250 ml/h, maybe a bolus before
Stop when necessary, we don't want edema
Look for: haematocrit, BUN, hemodynamics, SIRS
controlled and target-oriented
200-250 ml/h, maybe a bolus before
Stop when necessary, we don't want edema
Look for: haematocrit, BUN, hemodynamics, SIRS
17) Analgesia
18)
Mild pain: in Germany we like to use metamizol, not available for example in USA. Look what you have
Severe Pain: Opioids --> don't be afraid of spinster odd spastic. The patient must not have pain; in general and for the next point: nutrition!
Mild pain: in Germany we like to use metamizol, not available for example in USA. Look what you have
Severe Pain: Opioids --> don't be afraid of spinster odd spastic. The patient must not have pain; in general and for the next point: nutrition!
19) Nutrition
20)
-Try to start within the first 24 hours. Patient should have no pain.
- if possible oral
- gastric tube if necessary, maybe jejunal tube (prefer gastric tube if possible)
- enteral nutrition decreases risk of infection in comparison to total parenteral nutrition
-Try to start within the first 24 hours. Patient should have no pain.
- if possible oral
- gastric tube if necessary, maybe jejunal tube (prefer gastric tube if possible)
- enteral nutrition decreases risk of infection in comparison to total parenteral nutrition
21)
A while ago, we didn't feed the patients:
Background: We thought it makes the pancreas produce more lipase and worse it.
Now we know: the pancreas is damaged, it hardly produces any lipase.
A while ago, we didn't feed the patients:
Background: We thought it makes the pancreas produce more lipase and worse it.
Now we know: the pancreas is damaged, it hardly produces any lipase.
22) ERCP
If biliary cause
Only urgent in case of cholangitis (within 24 hours)
Otherwise no early ERCP! --> more complications, more infections!
If biliary cause
Only urgent in case of cholangitis (within 24 hours)
Otherwise no early ERCP! --> more complications, more infections!
23) Antibiotics
24) Antibiotics
Acute pancreatitis is primary sterile --> no AB
- AB when there are other infections you need to treat
- infected necrosis
- sepsis
AB of choice: carbapenems --> go well into the pancreas
Acute pancreatitis is primary sterile --> no AB
- AB when there are other infections you need to treat
- infected necrosis
- sepsis
AB of choice: carbapenems --> go well into the pancreas
25) It's not easy with antibiotics
- long time administration of AB on ICU increase risk for multi resistant bacteria and fungi
- early administration of AB increase risk for Candida infections
- long time administration of AB on ICU increase risk for multi resistant bacteria and fungi
- early administration of AB increase risk for Candida infections
26)
Rare: hypertriglyceridemia as cause
Think about it especially in young people with no other risks
Therapy: consider plasmapheresis
Rare: hypertriglyceridemia as cause
Think about it especially in young people with no other risks
Therapy: consider plasmapheresis
27) About after 72-96 hours look for complications:
- necrosis
- pseudocysts
- intraabdominal compartment
- necrosis
- pseudocysts
- intraabdominal compartment
28) intraabdominal compartment:
Bladder pressure measurement
Healthy: 0 mmHg
ICU: 5-7 mmHg
Obesity: 7-14 mmHg
intraabdominal copartment: >20 mmHg and new organ failure (I personally think, new organ failure not necessary in ICU patients, they often have enough organ failures.
Bladder pressure measurement
Healthy: 0 mmHg
ICU: 5-7 mmHg
Obesity: 7-14 mmHg
intraabdominal copartment: >20 mmHg and new organ failure (I personally think, new organ failure not necessary in ICU patients, they often have enough organ failures.
29) Therapy of intraabdominal compartment
Relieve the gut, start with mild interventions, step up.
E.g. Gastric tube on drain, enema, drainage of intraabominal processes.
Last step: Surgery: No surgeon wants to to surgery in that mess. But inform him about the patient!
Relieve the gut, start with mild interventions, step up.
E.g. Gastric tube on drain, enema, drainage of intraabominal processes.
Last step: Surgery: No surgeon wants to to surgery in that mess. But inform him about the patient!
30) Necrosis - early
- early necrosis: local fluid (acute perpancreatic fluid collection, APFC)
- local necrosis without capsule (acute necrotic collecition; ANC)
- early necrosis: local fluid (acute perpancreatic fluid collection, APFC)
- local necrosis without capsule (acute necrotic collecition; ANC)
31) Necrosis late, Pseudocysts
- encapsulated necrosis (Walled-off Necrose)
- pancreas pseudocyst
- encapsulated necrosis (Walled-off Necrose)
- pancreas pseudocyst
32) Therapy of necrosis: Step up Antibiotics, drainage, surgery In 30% drainage sufficient But Walled-off Nekrose often needs necrosectomy
33) Therapy of fluid content --> endoscopy Therapy of necrosis --> endoscopic step up, then surgical step up
34) Sum it up (1):
- Fluids, Analgesia, Nutrition (oral->enteral->parenteral)
- AB only when there is an infection
- ERCP if biliary (not too early, only early, if cholangitis)
- Drainage for infected, complicated or symptomatic necrosis
- Fluids, Analgesia, Nutrition (oral->enteral->parenteral)
- AB only when there is an infection
- ERCP if biliary (not too early, only early, if cholangitis)
- Drainage for infected, complicated or symptomatic necrosis
35) Sum it up (2)
-Debrediment: not early, after 4 weeks about, individual
-Debrediment: not early, after 4 weeks about, individual
36) One word to Covid-19
It seems, that acute pancreatitis is not a sign of COVID-19, but can appear in sepsis.
Intersting: In Japan, camostat mesylate is used for treatment of acute pancreatitis and there are trials (or one trial?) for its use in COVID-19
It seems, that acute pancreatitis is not a sign of COVID-19, but can appear in sepsis.
Intersting: In Japan, camostat mesylate is used for treatment of acute pancreatitis and there are trials (or one trial?) for its use in COVID-19
37) Well, two words to COVID-19
Maybe more diabetes after COVID-19 --> pancreas affected?
Maybe more diabetes after COVID-19 --> pancreas affected?
38) Personal opinion (1)
American guidelines suggest in biliary pancreatitis cholecystectomy during the initial admission rather than after discharge. I personally think, it is better to do it later, when patients have no symptoms. An acute pancreatitis abdomen is a mess.
American guidelines suggest in biliary pancreatitis cholecystectomy during the initial admission rather than after discharge. I personally think, it is better to do it later, when patients have no symptoms. An acute pancreatitis abdomen is a mess.
39) Personal opinion (2)
Should we make a surgery in such an abdomen and after the patient had a severe illness? I think, later is better (of course there remains the risk for acute pancreatitis and cholangitis as long as the gall bladder is in).
Should we make a surgery in such an abdomen and after the patient had a severe illness? I think, later is better (of course there remains the risk for acute pancreatitis and cholangitis as long as the gall bladder is in).
40) Thank you for your attention!
Feel free to comment, criticize and ask!
Feel free to comment, criticize and ask!

 Read on Twitter
Read on Twitter