I agree this change in focus from deductibles to providers seems like the obvious solution — to health policy analysts & economists. But not to employers (the ones who would need to implement this). We spoke to dozens of large employers about why this is: https://www.healthsystemtracker.org/brief/employer-strategies-to-reduce-health-costs-and-improve-quality-through-network-configuration/ https://twitter.com/zackcooperyale/status/1359484580730966019
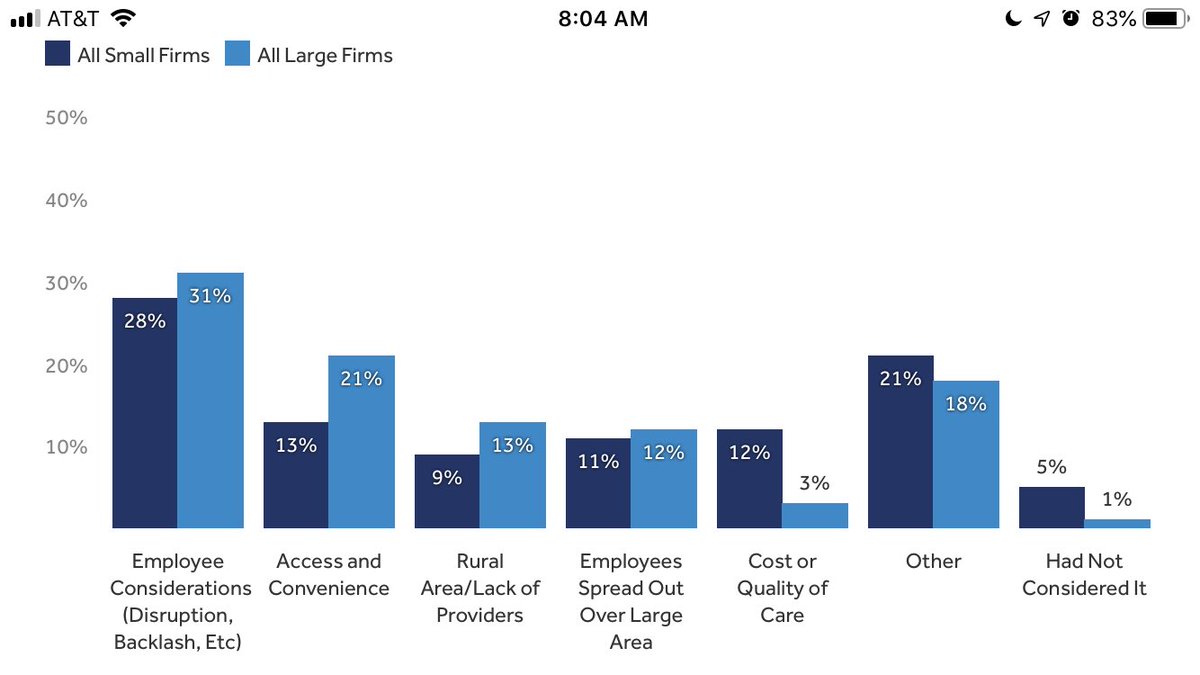
Even large employers face a lot of constraints when it comes to doing anything creative with provider networks. Some of the problem is about capacity/knowledge, but also geography and logistics.
There were also several HR directors/benefit managers in our focus groups who did not understand that prices/reimbursement rates are driving their health costs up. I stayed after to explain more and they kept talking about wellness plans driving down utilization rates.
Many HR directors who did grasp the concept of leveraging provider networks to lower their health costs said their insurers, brokers, or consultants had never brought this up to them. Most people in our focus groups had never heard of most of these options.
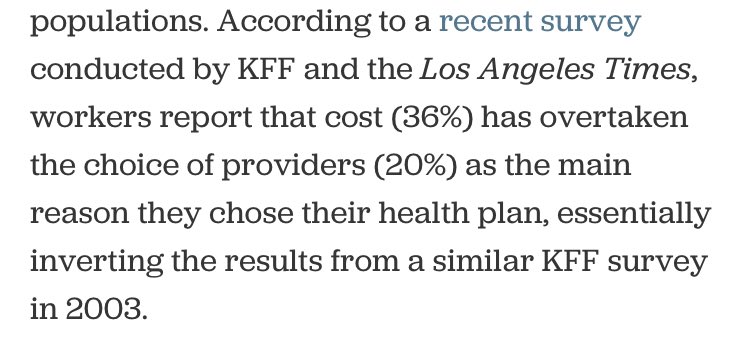
One other challenge: I heard a mismatch between what employers think employees want (provider choice) vs what employees increasingly say they want (lower costs). Employers fear employee backlash against network changes, so they raise deductibles instead.

 Read on Twitter
Read on Twitter