Minor burns are a common Paeds ED presentation.
Do you know how to assess them and treat them?
Do you deroof your blisters?
Do you know how to calculate the total body surface area of the burn?
See http://DFTBSkinDeep.com for more burns pictures
A thread
1/12
Do you know how to assess them and treat them?
Do you deroof your blisters?
Do you know how to calculate the total body surface area of the burn?
See http://DFTBSkinDeep.com for more burns pictures
A thread
1/12
Get a clear history. Pulling a cup of tea off the counter is a common causes of burns in young children.
How long ago had the tea been made?
Was there milk in it?
What was the child wearing?
Get all the details including who was there at the time.
2/12
How long ago had the tea been made?
Was there milk in it?
What was the child wearing?
Get all the details including who was there at the time.
2/12
Has simple first aid been completed? Run the burn under cool water (15-18°C for 20 mins) within 3 hours.
Toothpaste/jam/honey don’t work.
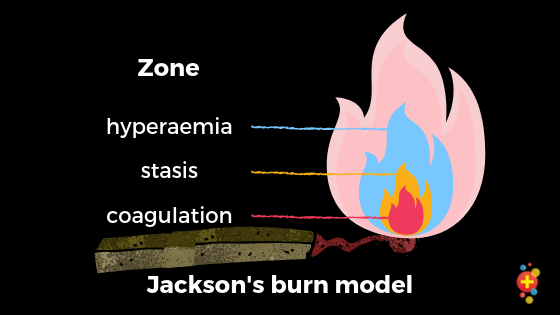
The zone of stasis has potentially reversible damage. Don’t let the patient burn more. Cool the burn.
https://dontforgetthebubbles.com/cool-runnings/
3/12
Toothpaste/jam/honey don’t work.
The zone of stasis has potentially reversible damage. Don’t let the patient burn more. Cool the burn.
https://dontforgetthebubbles.com/cool-runnings/
3/12
It’s easy to forget analgesia. They will likely be in pain + distress. Give paracetamol + ibuprofen. Consider IN options (fentanyl, diamorphine) or get IV access.
Use a play therapist if you have one. Offer reassurance to the child + parent. It’s a stressful time.
4/12
Use a play therapist if you have one. Offer reassurance to the child + parent. It’s a stressful time.
4/12
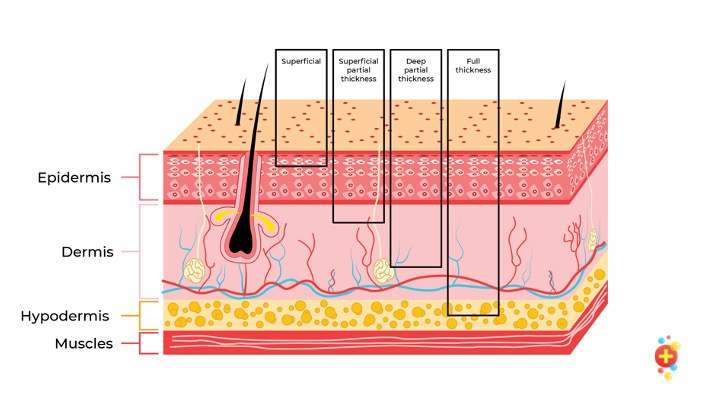
Assess depth
Superficial: red, no blisters, brisk cap refill, sore.
Sup partial: pale pink/red, brisk cap refill, exudate, blisters, sore.
Deep dermal: dark red/white, mottled, delayed cap refill.
Full thickness: dry/leathery, no cap refill, no sensation.
5/12
Superficial: red, no blisters, brisk cap refill, sore.
Sup partial: pale pink/red, brisk cap refill, exudate, blisters, sore.
Deep dermal: dark red/white, mottled, delayed cap refill.
Full thickness: dry/leathery, no cap refill, no sensation.
5/12
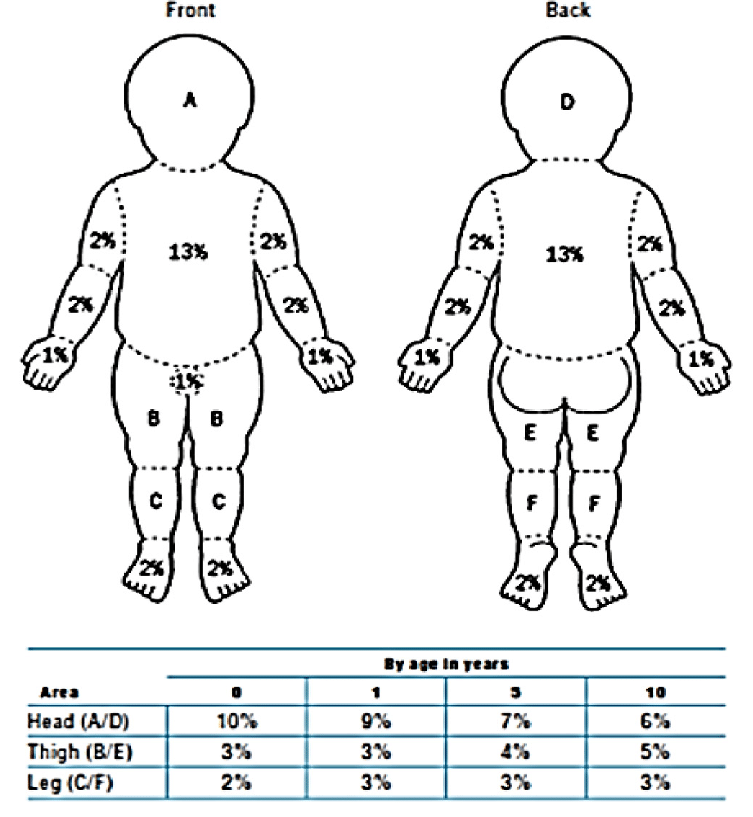
Assess the total body surface area affected.
Erythema doesn’t count when calculating the %.
Only include superficial partial thickness or more.
Use the Mersey Burns app or Lund + Browder chart.
The palm is 1%.
You are aiming for an estimate, so do your best.
6/12
Erythema doesn’t count when calculating the %.
Only include superficial partial thickness or more.
Use the Mersey Burns app or Lund + Browder chart.
The palm is 1%.
You are aiming for an estimate, so do your best.
6/12
Always think safeguarding. Is the burn in keeping with the description?
Are there splash marks around the edges or clearly demarcated edges?
Is it a specific pattern e.g. linear or a particular shape.
Ask about social history.
7/12
Are there splash marks around the edges or clearly demarcated edges?
Is it a specific pattern e.g. linear or a particular shape.
Ask about social history.
7/12
Deroofing (not every centre does the same here). We deroof all of ours.
Sometimes the burn looks much larger after deroofing + you can clean it, get a better view + assessment.
Dress with a non-adherent dressing then gauze to soak up the exudate.
Review in 2-3 days.
8/12
Sometimes the burn looks much larger after deroofing + you can clean it, get a better view + assessment.
Dress with a non-adherent dressing then gauze to soak up the exudate.
Review in 2-3 days.
8/12
Refer to the burns service for burns on the face, hands, joints, feet, genitalia, or scalp. Refer if circumferential, chemical, or NAI. Refer if >1% TBSA in children (LSEBN guidelines)
Refer also if it gets infected or doesn’t heal within two weeks
https://www.lsebn.nhs.uk/page1.aspx?p=16&t=1
9/12
Refer also if it gets infected or doesn’t heal within two weeks
https://www.lsebn.nhs.uk/page1.aspx?p=16&t=1
9/12
The Parkland formula is really for kids with >10% TBSA burns (NOT minor burns + so just getting a brief mention here)
The calc is 4ml/kg/%TBSA
The 1st half is over 8h; the 2nd half over the next 16h (Hartmann's).
This is ON TOP of maintenance + any resus boluses needed
10/12
The calc is 4ml/kg/%TBSA
The 1st half is over 8h; the 2nd half over the next 16h (Hartmann's).
This is ON TOP of maintenance + any resus boluses needed
10/12
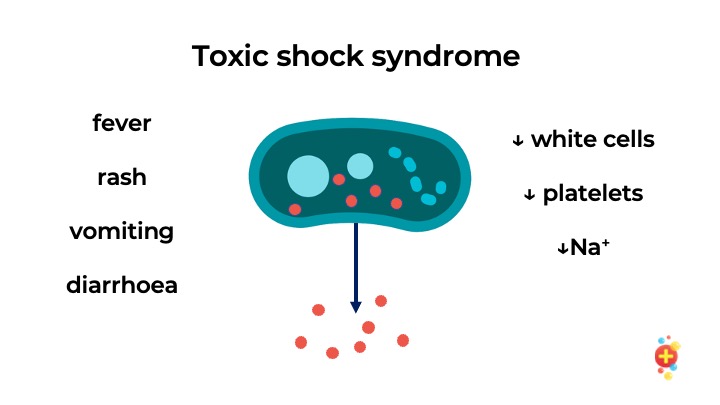
When sending minor burns home, tell them about signs of toxic shock – diarrhoea, fever, rash, vomiting. Usually develops Day 2-4
The burn might look clean – it’s colonised, not infected. Commonly caused by staph, strep, MRSA
If toxic shock signs, admit for IV antibiotics
11/12
The burn might look clean – it’s colonised, not infected. Commonly caused by staph, strep, MRSA
If toxic shock signs, admit for IV antibiotics
11/12

 Read on Twitter
Read on Twitter