#Rheumatology Fun
Let’s take a deep dive into a unique subset of rheumatic diseases
This week's RTL guest tweetorial from @MithuRheum!
Let’s take a deep dive into a unique subset of rheumatic diseases

This week's RTL guest tweetorial from @MithuRheum!
CASE 1:
 A 52 yo male presents to clinic w/ 6 months of hand ulcerations on the dorsal surface of the hands & elbow, oral ulcers, a violaceous periorbital rash and mild arthralgias
A 52 yo male presents to clinic w/ 6 months of hand ulcerations on the dorsal surface of the hands & elbow, oral ulcers, a violaceous periorbital rash and mild arthralgias
 CT chest demonstrates nodular opacities
CT chest demonstrates nodular opacities
 A 52 yo male presents to clinic w/ 6 months of hand ulcerations on the dorsal surface of the hands & elbow, oral ulcers, a violaceous periorbital rash and mild arthralgias
A 52 yo male presents to clinic w/ 6 months of hand ulcerations on the dorsal surface of the hands & elbow, oral ulcers, a violaceous periorbital rash and mild arthralgias CT chest demonstrates nodular opacities
CT chest demonstrates nodular opacities
Based on the clinical presentation and photograph of the ulcers, which of the following is the most likely diagnosis?


On exam:
 You note bilateral inspiratory crackles at the
You note bilateral inspiratory crackles at the  bases, although he's breathing comfortably on room air
bases, although he's breathing comfortably on room air
 Musculoskeletal exam reveals no synovitis
Musculoskeletal exam reveals no synovitis
 Manual muscle strength exam is 5/5 throughout all major muscle groups
Manual muscle strength exam is 5/5 throughout all major muscle groups
Which laboratory test do you order next?
 You note bilateral inspiratory crackles at the
You note bilateral inspiratory crackles at the  bases, although he's breathing comfortably on room air
bases, although he's breathing comfortably on room air Musculoskeletal exam reveals no synovitis
Musculoskeletal exam reveals no synovitis Manual muscle strength exam is 5/5 throughout all major muscle groups
Manual muscle strength exam is 5/5 throughout all major muscle groupsWhich laboratory test do you order next?

Inflammatory myopathies:
 Aka idiopathic inflammatory myopathies (IIM); can present with a variety of symptoms & most commonly *symmetric proximal muscle weakness*
Aka idiopathic inflammatory myopathies (IIM); can present with a variety of symptoms & most commonly *symmetric proximal muscle weakness*
 Other signs include: heliotrope rash
Other signs include: heliotrope rash  , Gottron’s papules (see image), interstitial lung disease, dysphagia
, Gottron’s papules (see image), interstitial lung disease, dysphagia
 Aka idiopathic inflammatory myopathies (IIM); can present with a variety of symptoms & most commonly *symmetric proximal muscle weakness*
Aka idiopathic inflammatory myopathies (IIM); can present with a variety of symptoms & most commonly *symmetric proximal muscle weakness* Other signs include: heliotrope rash
Other signs include: heliotrope rash  , Gottron’s papules (see image), interstitial lung disease, dysphagia
, Gottron’s papules (see image), interstitial lung disease, dysphagia
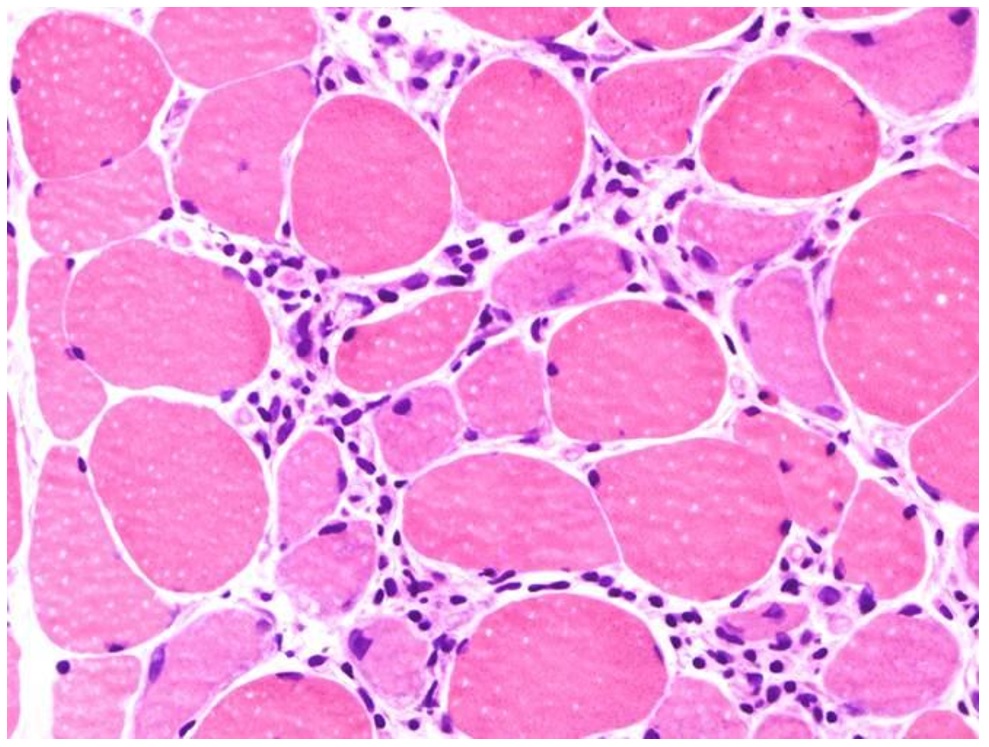
IIM mechanism?
Lymphocytic infiltrates in muscle tissue and expression of autoantibodies against muscle are part of the immune mechanisms contributing to myositis!
T- and B-cell proliferation and activation can be seen on muscle biopsy



Lymphocytic infiltrates in muscle tissue and expression of autoantibodies against muscle are part of the immune mechanisms contributing to myositis!
T- and B-cell proliferation and activation can be seen on muscle biopsy



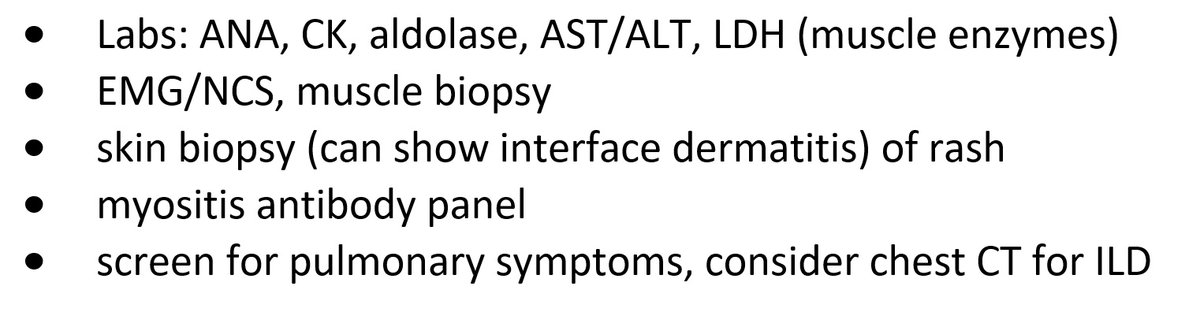
After a comprehensive physical exam, here is some of the diagnostic workup that should be considered if you have a patient and are concerned for myositis:






Laboratory workup reveals:
+ANA 1:160 (homogenous)
Normal CK & aldolase
You suspect this patient has MDA-5 Dermatomyositis (DM), an idiopathic inflammatory myopathy (aka myositis)
MDA-5 DM can be clinically amyopathic w/ rapidly progressive interstitial lung disease (ILD)

+ANA 1:160 (homogenous)
Normal CK & aldolase
You suspect this patient has MDA-5 Dermatomyositis (DM), an idiopathic inflammatory myopathy (aka myositis)
MDA-5 DM can be clinically amyopathic w/ rapidly progressive interstitial lung disease (ILD)


Clinical features in MDA-5 DM include:
 Cutaneous ulcers
Cutaneous ulcers
 Oral ulcers
Oral ulcers
 Alopecia
Alopecia
 Pulmonary symptoms 2/2 ILD
Pulmonary symptoms 2/2 ILD
MDA-5 myositis can be clinically amyopathic!
 this means that pts may *not* have muscle weakness on exam & can have normal muscle enzymes (CK, AST, ALT, aldolase)
this means that pts may *not* have muscle weakness on exam & can have normal muscle enzymes (CK, AST, ALT, aldolase)
 Cutaneous ulcers
Cutaneous ulcers Oral ulcers
Oral ulcers Alopecia
Alopecia Pulmonary symptoms 2/2 ILD
Pulmonary symptoms 2/2 ILD MDA-5 myositis can be clinically amyopathic!
 this means that pts may *not* have muscle weakness on exam & can have normal muscle enzymes (CK, AST, ALT, aldolase)
this means that pts may *not* have muscle weakness on exam & can have normal muscle enzymes (CK, AST, ALT, aldolase)
 - skin biopsy now shows interface dermatitis
- skin biopsy now shows interface dermatitis because of *new* dyspnea on exertion
because of *new* dyspnea on exertion  , you evaluate the patient and admit for further workup
, you evaluate the patient and admit for further workup Which laboratory marker should be checked to determine prognosis?
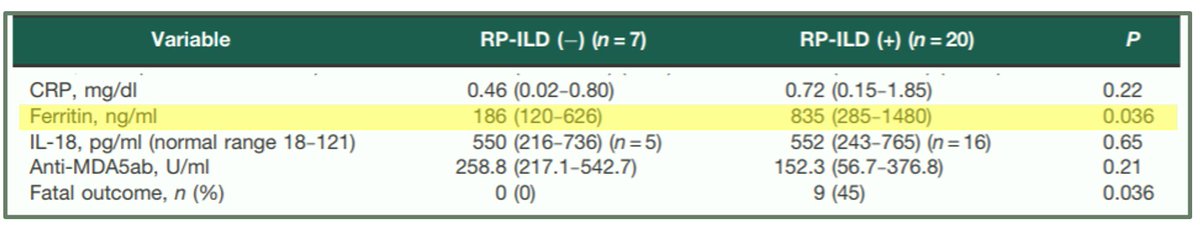
 Ferritin level is an important prognostic marker for development of rapidly progressive ILD (RP-ILD) & mortality
Ferritin level is an important prognostic marker for development of rapidly progressive ILD (RP-ILD) & mortalityFrom a 2012 study:
MDA-5 DM patients with RP-ILD had
 ferritin than those without ILD
ferritin than those without ILDMDA-5 DM patients who died also had
 ferritin than patients who lived
ferritin than patients who lived
Notably, there was *no* difference in CRP levels between these two MDA-5 DM groups: w/ RP-ILD & w/o RP-ILD
 it's possible the hyperferritinemia is not simply a reflection of the acute phase response, but a true pathophysiological mechanism
it's possible the hyperferritinemia is not simply a reflection of the acute phase response, but a true pathophysiological mechanism
 a viral trigger may be associated!
a viral trigger may be associated!
 it's possible the hyperferritinemia is not simply a reflection of the acute phase response, but a true pathophysiological mechanism
it's possible the hyperferritinemia is not simply a reflection of the acute phase response, but a true pathophysiological mechanism a viral trigger may be associated!
a viral trigger may be associated!
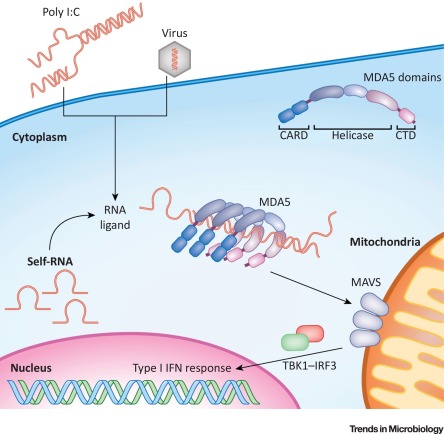
What is MDA-5?
 MDA5 is an interferon-induced RNA helicase which senses ssRNA viruses (e.g. SARS-CoV-2!)
MDA5 is an interferon-induced RNA helicase which senses ssRNA viruses (e.g. SARS-CoV-2!)
 Some hypothesize MDA-5 DM as a form of macrophage activation syndrome - given high ferritin & IL-18 levels - that targets skin and lungs related to an infectious trigger
Some hypothesize MDA-5 DM as a form of macrophage activation syndrome - given high ferritin & IL-18 levels - that targets skin and lungs related to an infectious trigger
 MDA5 is an interferon-induced RNA helicase which senses ssRNA viruses (e.g. SARS-CoV-2!)
MDA5 is an interferon-induced RNA helicase which senses ssRNA viruses (e.g. SARS-CoV-2!) Some hypothesize MDA-5 DM as a form of macrophage activation syndrome - given high ferritin & IL-18 levels - that targets skin and lungs related to an infectious trigger
Some hypothesize MDA-5 DM as a form of macrophage activation syndrome - given high ferritin & IL-18 levels - that targets skin and lungs related to an infectious trigger
CASE 2:
Suppose instead you have a patient with:
 Psoriatic-like lesions
Psoriatic-like lesions
 Hyperkeratotic papules on palmar & digital flexor surfaces
Hyperkeratotic papules on palmar & digital flexor surfaces
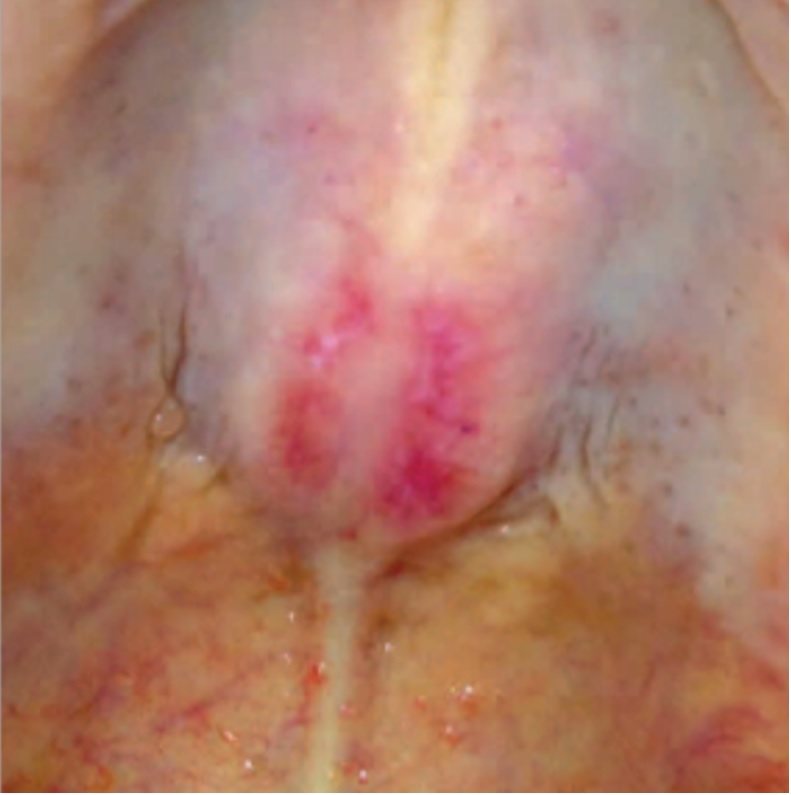
 This lesion
This lesion  on the roof of the mouth
on the roof of the mouth
Suppose instead you have a patient with:
 Psoriatic-like lesions
Psoriatic-like lesions Hyperkeratotic papules on palmar & digital flexor surfaces
Hyperkeratotic papules on palmar & digital flexor surfaces This lesion
This lesion  on the roof of the mouth
on the roof of the mouth
 Which myositis-specific antibody do you suspect will come back positive on the myositis antibody panel in this patient?
Which myositis-specific antibody do you suspect will come back positive on the myositis antibody panel in this patient?
 ... this patient has TIF1y dermatomyositis
... this patient has TIF1y dermatomyositis TIF1y DM can cause psoriasis-like lesions & this finding of an ovoid palatal patch (symmetric curved erythema on hard palate w/ white macules)
TIF1y DM can cause psoriasis-like lesions & this finding of an ovoid palatal patch (symmetric curved erythema on hard palate w/ white macules) It's important to screen patients w/ DM for malignancy, especially if TIF1y positive!
It's important to screen patients w/ DM for malignancy, especially if TIF1y positive!
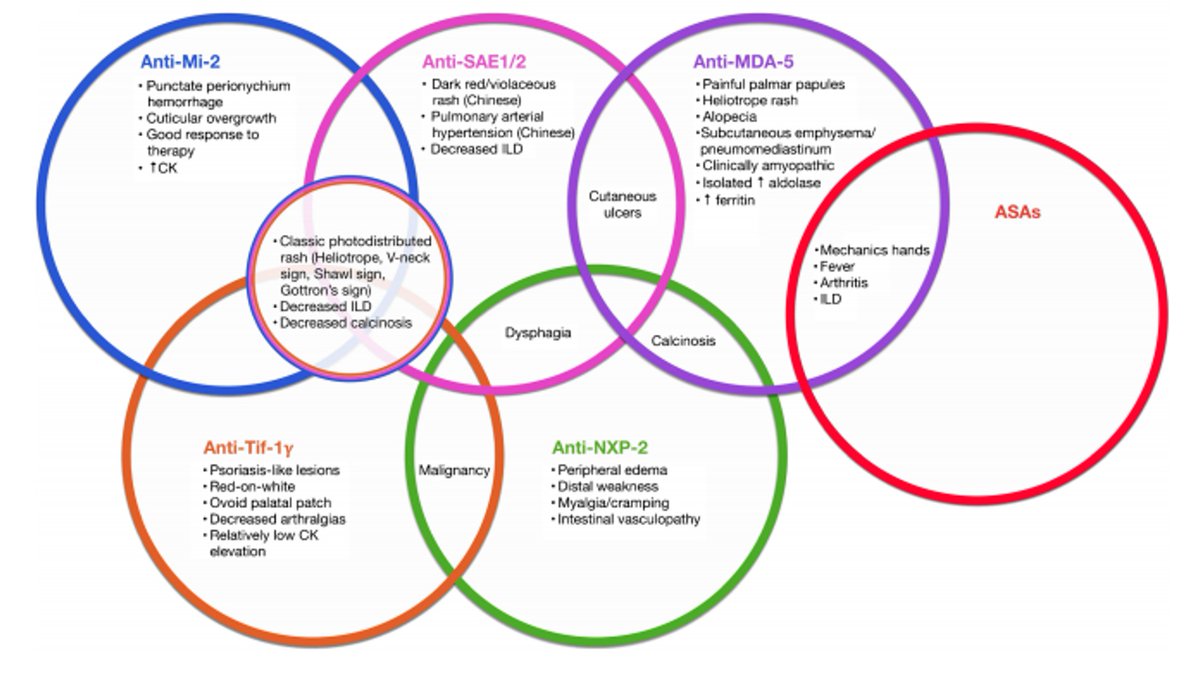
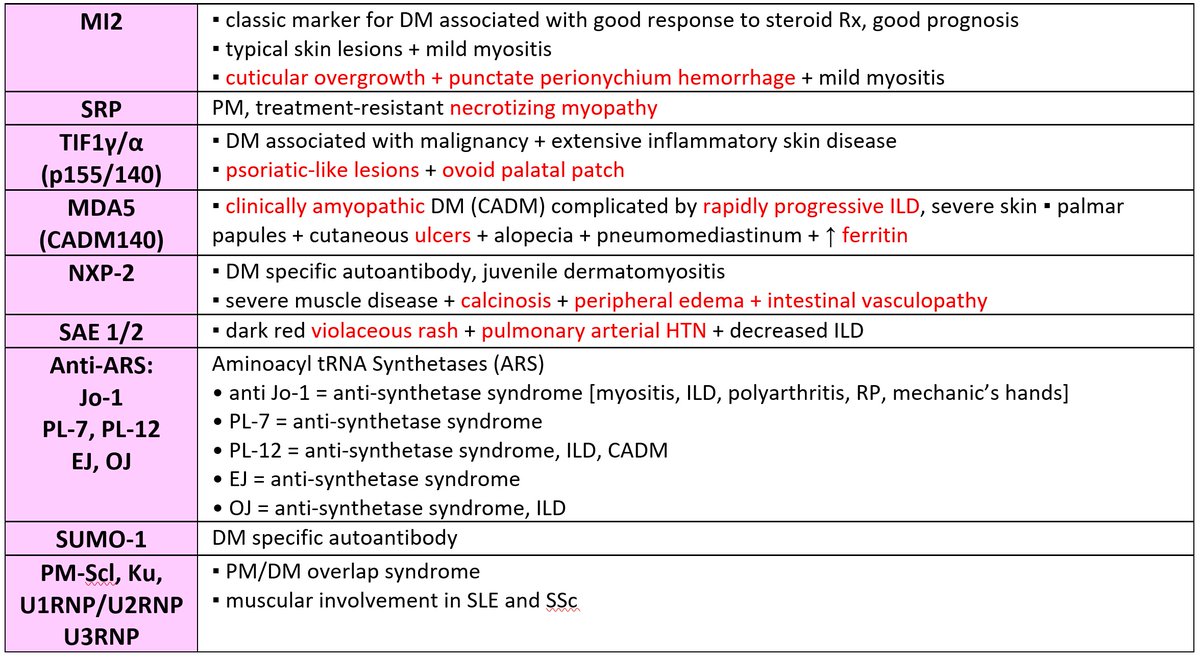
So... why do these antibodies matter, clinically?
 recognizing specific phenotypes associated with myositis-specific antibodies (MSAs) can help identify the particular IIM subtype and its various systemic manifestations
recognizing specific phenotypes associated with myositis-specific antibodies (MSAs) can help identify the particular IIM subtype and its various systemic manifestations
More examples?
see
 recognizing specific phenotypes associated with myositis-specific antibodies (MSAs) can help identify the particular IIM subtype and its various systemic manifestations
recognizing specific phenotypes associated with myositis-specific antibodies (MSAs) can help identify the particular IIM subtype and its various systemic manifestationsMore examples?
see

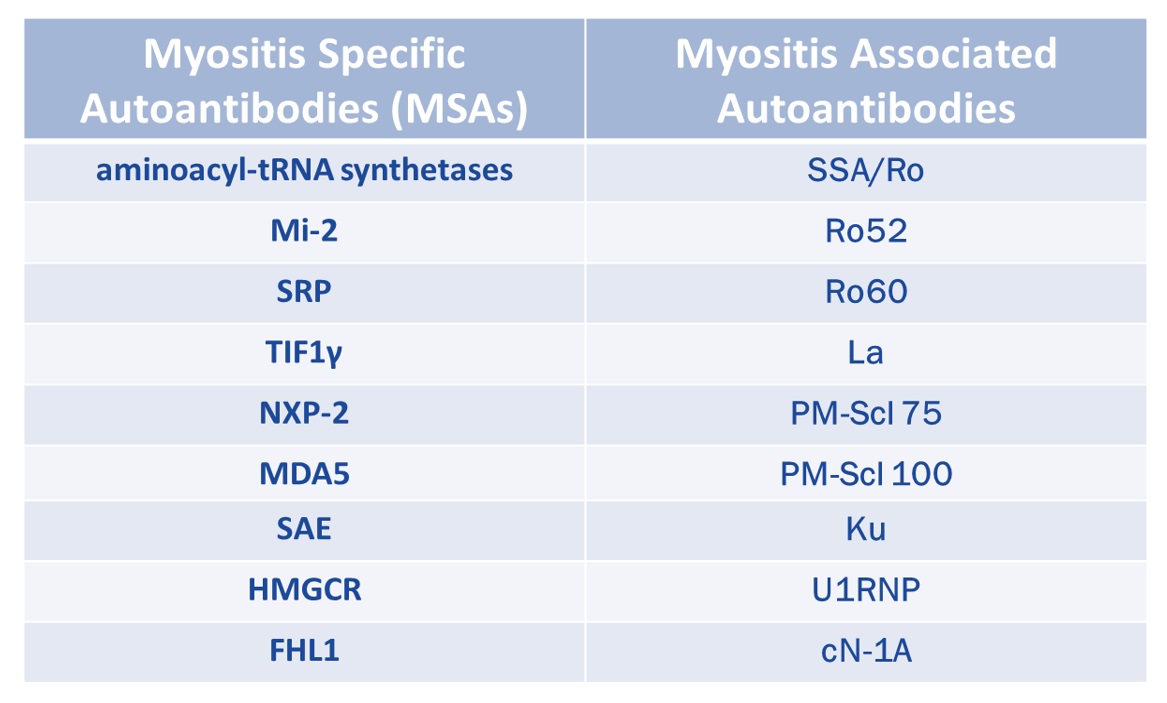
Here's a reference chart to keep the different types of myositis-specific antibodies (MSAs) organized!






Keep in mind that some autoantibodies are *non-specific*
While they can be detected in patients with myositis, they are also seen in other autoimmune disorders (e.g. Ro52 in scleroderma)!
 these are called myositis-associated antibodies (MAAs)
these are called myositis-associated antibodies (MAAs)
MSAs vs MAAs:
While they can be detected in patients with myositis, they are also seen in other autoimmune disorders (e.g. Ro52 in scleroderma)!
 these are called myositis-associated antibodies (MAAs)
these are called myositis-associated antibodies (MAAs)
MSAs vs MAAs:
One can check the myositis antibody panel to see which of the MSAs are included at their institution
Of note: specific types of inflammatory myopathies – such as HMGCR necrotizing myopathy – are *not* included in the MyoMarker 3 panel (most commonly used myositis Ab panel)
Of note: specific types of inflammatory myopathies – such as HMGCR necrotizing myopathy – are *not* included in the MyoMarker 3 panel (most commonly used myositis Ab panel)
To learn more about the identification of myositis-specific antibodies (MSAs) and association with distinct clinical phenotypes, check out this article by myself and @LisaCriscione:
https://www.the-rheumatologist.org/article/myositis-specific-antibodies-identified/
https://www.the-rheumatologist.org/article/myositis-specific-antibodies-identified/
REFs (1/2):
(1) https://pubmed.ncbi.nlm.nih.gov/31365803/
(2) Gono et. al. Rheumatology (Oxford). 2012 Sep;51(9):1563-70.
(3) Gono et. al. Rheumatology (Oxford). 2010 Jul;49(7):1354-60.
(4) Fiorentino et. al. J Am Acad Dermatol. 2011 Jul;65(1):25-34.
(1) https://pubmed.ncbi.nlm.nih.gov/31365803/
(2) Gono et. al. Rheumatology (Oxford). 2012 Sep;51(9):1563-70.
(3) Gono et. al. Rheumatology (Oxford). 2010 Jul;49(7):1354-60.
(4) Fiorentino et. al. J Am Acad Dermatol. 2011 Jul;65(1):25-34.
REFs (2/2):
(5) Moghadam-Kia S et al. Curr Rheumatol Rep. 2018 Oct 31;20(12):78.
(6) Bernet et. al. JAMA Dermatol. 2016 Sep 1;152(9):1049-51.
(7) Wolstencroft PW & Fiorentino DF. Curr Rheumatol Rep. 2018 Apr 10;20(5):28.
(8) https://www.sciencedirect.com/science/article/pii/S0966842X18301793
(5) Moghadam-Kia S et al. Curr Rheumatol Rep. 2018 Oct 31;20(12):78.
(6) Bernet et. al. JAMA Dermatol. 2016 Sep 1;152(9):1049-51.
(7) Wolstencroft PW & Fiorentino DF. Curr Rheumatol Rep. 2018 Apr 10;20(5):28.
(8) https://www.sciencedirect.com/science/article/pii/S0966842X18301793

 Read on Twitter
Read on Twitter