(1/10) Pt on D7 daptomycin (DAP) for MRSA  BSI develops dyspnea, fever
BSI develops dyspnea, fever  , diffuse bilateral infiltrates on CXR. Intubated
, diffuse bilateral infiltrates on CXR. Intubated  Bronch w/BAL NGTD. WBC 12 (Neuts 0.6 / Eos 0.3 /Lymphs 0.18). Likely diagnosis?
Bronch w/BAL NGTD. WBC 12 (Neuts 0.6 / Eos 0.3 /Lymphs 0.18). Likely diagnosis?
 BSI develops dyspnea, fever
BSI develops dyspnea, fever  , diffuse bilateral infiltrates on CXR. Intubated
, diffuse bilateral infiltrates on CXR. Intubated  Bronch w/BAL NGTD. WBC 12 (Neuts 0.6 / Eos 0.3 /Lymphs 0.18). Likely diagnosis?
Bronch w/BAL NGTD. WBC 12 (Neuts 0.6 / Eos 0.3 /Lymphs 0.18). Likely diagnosis?
Let's start by exploring the DAP MOA DAP binds and depolarizes the cell membrane, allowing efflux of K+
DAP binds and depolarizes the cell membrane, allowing efflux of K+  . https://www.cubicin.com/mechanism-of-action/moa/
. https://www.cubicin.com/mechanism-of-action/moa/
 DAP binds and depolarizes the cell membrane, allowing efflux of K+
DAP binds and depolarizes the cell membrane, allowing efflux of K+  . https://www.cubicin.com/mechanism-of-action/moa/
. https://www.cubicin.com/mechanism-of-action/moa/
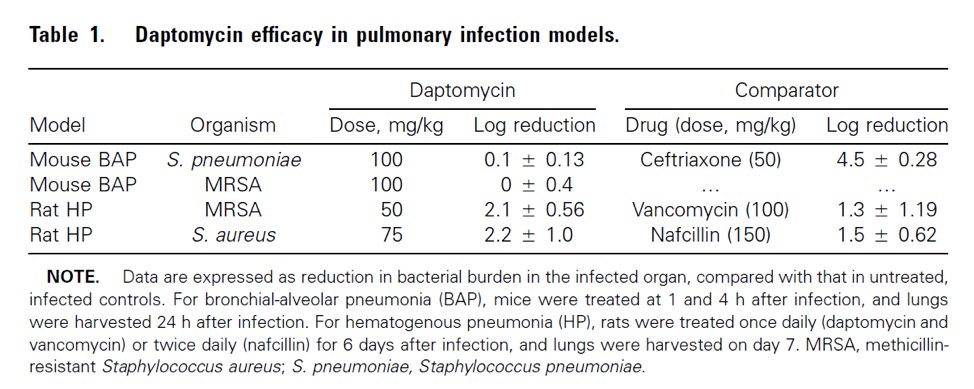
(4/10) #1 DAP is deactivated by lung surfactant making it ineffective for PNA. This  model demonstrates little/no DAP lung activity.
model demonstrates little/no DAP lung activity.  https://pubmed.ncbi.nlm.nih.gov/15898002/
https://pubmed.ncbi.nlm.nih.gov/15898002/
 model demonstrates little/no DAP lung activity.
model demonstrates little/no DAP lung activity.  https://pubmed.ncbi.nlm.nih.gov/15898002/
https://pubmed.ncbi.nlm.nih.gov/15898002/
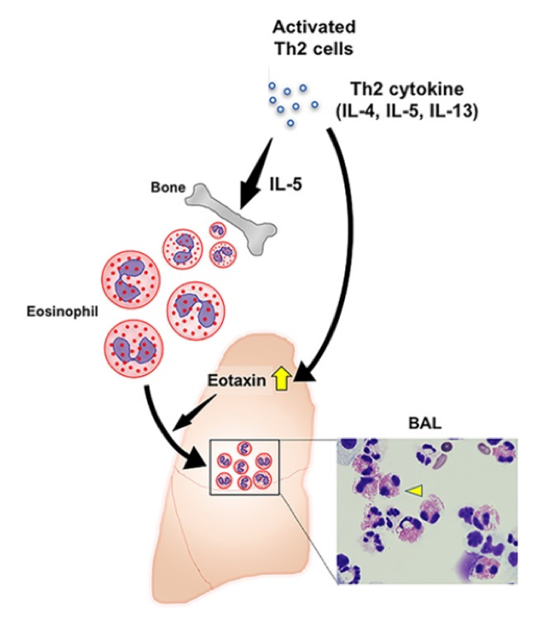
(5/10) #2: DAP interaction with surfactant  inflammation
inflammation  T-cell activation
T-cell activation  IL-5 release
IL-5 release  eosinophil production
eosinophil production  eotaxin attraction of eosinophils to the
eotaxin attraction of eosinophils to the  . (Picture: https://onlinelibrary.wiley.com/doi/full/10.1002/iid3.238)
. (Picture: https://onlinelibrary.wiley.com/doi/full/10.1002/iid3.238)
 inflammation
inflammation  T-cell activation
T-cell activation  IL-5 release
IL-5 release  eosinophil production
eosinophil production  eotaxin attraction of eosinophils to the
eotaxin attraction of eosinophils to the  . (Picture: https://onlinelibrary.wiley.com/doi/full/10.1002/iid3.238)
. (Picture: https://onlinelibrary.wiley.com/doi/full/10.1002/iid3.238)
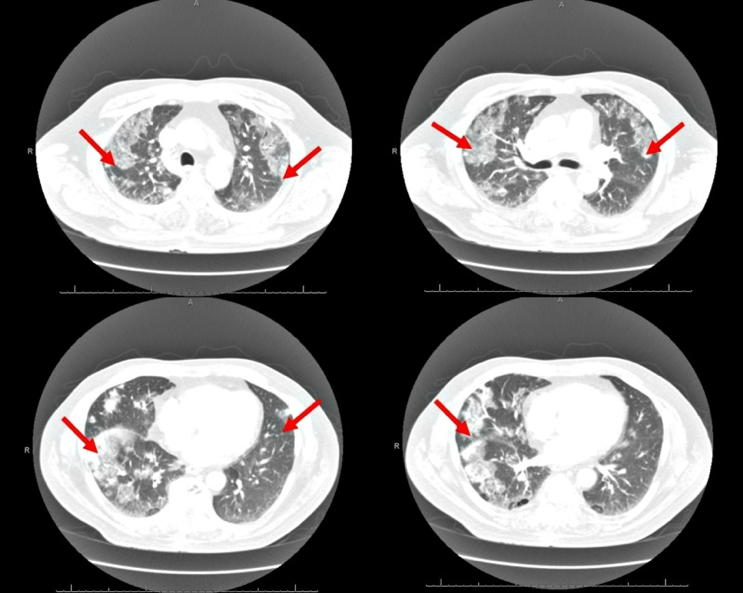
(6/10) DAP-induced eosinophilic PNA (AEP) should be suspected with DAP exposure + >25% eosinophils in bronch + fever +
fever + 
 dyspnea + new diffuse bilateral infiltrates on CT/CXR. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6207288/figure/FIG2/
dyspnea + new diffuse bilateral infiltrates on CT/CXR. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6207288/figure/FIG2/
 fever +
fever + 
 dyspnea + new diffuse bilateral infiltrates on CT/CXR. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6207288/figure/FIG2/
dyspnea + new diffuse bilateral infiltrates on CT/CXR. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6207288/figure/FIG2/
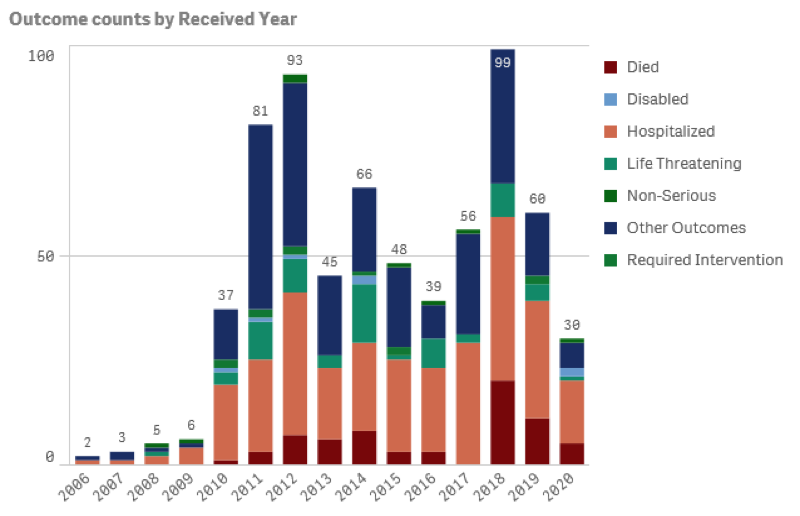
(7/10) There are <700 FAERS reports of DAP AEP over 15 years, with a majority of patients requiring hospitalization  and intervention. ( https://fis.fda.gov/sense/app/d10be6bb-494e-4cd2-82e4-0135608ddc13)
and intervention. ( https://fis.fda.gov/sense/app/d10be6bb-494e-4cd2-82e4-0135608ddc13)
 and intervention. ( https://fis.fda.gov/sense/app/d10be6bb-494e-4cd2-82e4-0135608ddc13)
and intervention. ( https://fis.fda.gov/sense/app/d10be6bb-494e-4cd2-82e4-0135608ddc13)
(8/10) Common ? Incidence independent of dose (4-10 mg/kg), median duration of therapy 2.8 weeks, 77% pts had
? Incidence independent of dose (4-10 mg/kg), median duration of therapy 2.8 weeks, 77% pts had  peripheral EOS. Resolution occurred within
peripheral EOS. Resolution occurred within  48-72 hours DAP D/C. https://aricjournal.biomedcentral.com/track/pdf/10.1186/s13756-016-0158-8.pdf
48-72 hours DAP D/C. https://aricjournal.biomedcentral.com/track/pdf/10.1186/s13756-016-0158-8.pdf
 ? Incidence independent of dose (4-10 mg/kg), median duration of therapy 2.8 weeks, 77% pts had
? Incidence independent of dose (4-10 mg/kg), median duration of therapy 2.8 weeks, 77% pts had  peripheral EOS. Resolution occurred within
peripheral EOS. Resolution occurred within  48-72 hours DAP D/C. https://aricjournal.biomedcentral.com/track/pdf/10.1186/s13756-016-0158-8.pdf
48-72 hours DAP D/C. https://aricjournal.biomedcentral.com/track/pdf/10.1186/s13756-016-0158-8.pdf
(9/10) Management:  stop daptomycin. Consider corticosteroids: IV methylprednisolone
stop daptomycin. Consider corticosteroids: IV methylprednisolone  60-125 mg Q6H
60-125 mg Q6H 
 prednisone 40-60 mg taper over 2-6 weeks. DAP rechallenge not
prednisone 40-60 mg taper over 2-6 weeks. DAP rechallenge not  recommended. https://aricjournal.biomedcentral.com/track/pdf/10.1186/s13756-016-0158-8.pdf
recommended. https://aricjournal.biomedcentral.com/track/pdf/10.1186/s13756-016-0158-8.pdf
 stop daptomycin. Consider corticosteroids: IV methylprednisolone
stop daptomycin. Consider corticosteroids: IV methylprednisolone  60-125 mg Q6H
60-125 mg Q6H 
 prednisone 40-60 mg taper over 2-6 weeks. DAP rechallenge not
prednisone 40-60 mg taper over 2-6 weeks. DAP rechallenge not  recommended. https://aricjournal.biomedcentral.com/track/pdf/10.1186/s13756-016-0158-8.pdf
recommended. https://aricjournal.biomedcentral.com/track/pdf/10.1186/s13756-016-0158-8.pdf
(10/10) Recap:
 AEP is a serious ADE of DAP and is under-reported
AEP is a serious ADE of DAP and is under-reported
 DAP attracted to alveolar surfactant
DAP attracted to alveolar surfactant  inflammation recruits eosinophils
inflammation recruits eosinophils
 Mgmt = Discontinue DAP and consider corticosteroids
Mgmt = Discontinue DAP and consider corticosteroids
 DAP rechallenge NOT recommended
DAP rechallenge NOT recommended
 AEP is a serious ADE of DAP and is under-reported
AEP is a serious ADE of DAP and is under-reported DAP attracted to alveolar surfactant
DAP attracted to alveolar surfactant  inflammation recruits eosinophils
inflammation recruits eosinophils Mgmt = Discontinue DAP and consider corticosteroids
Mgmt = Discontinue DAP and consider corticosteroids DAP rechallenge NOT recommended
DAP rechallenge NOT recommended

 Read on Twitter
Read on Twitter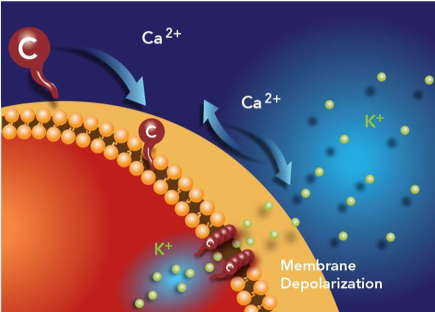
 for MRSA, but this MOA results in 2 respiratory
for MRSA, but this MOA results in 2 respiratory