1/ Ok somewhat long answer to this 
I never tell patients what approach they can or cannot do for diet, or medications for that matter. https://twitter.com/rotrader33/status/1357040822781308928

I never tell patients what approach they can or cannot do for diet, or medications for that matter. https://twitter.com/rotrader33/status/1357040822781308928
2/ I believe in patient education, treating adult patients like the intelligent individuals they are, forming a relationship based on patient centered care, and helping them to make a science based decision that best works for them.
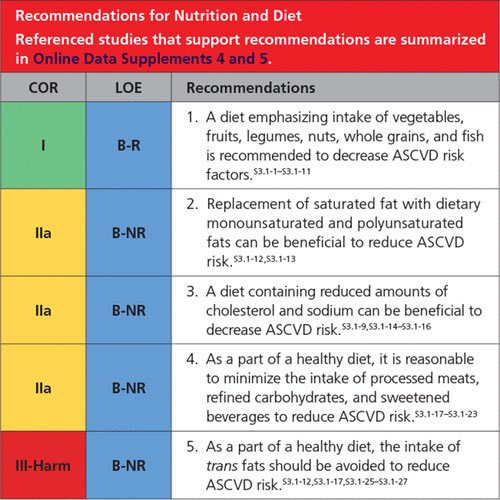
3/ Meaning: if a patient is interested in further information I believe in explaining guidelines, levels of evidence, and existing data to them in a digestible and easy to understand manner.
4/ We have some general ideas of dietary changes can help to reduce CV risk based on various levels of evidence.
5/ I see patients who follow all dietary paradigms, and believe in meeting patients where they are at, explaining risks and benefits, and doing what I can to support them choosing a path to reduce their CV risk: whether thats through lifestyle change, medications, or both.
6/ For example, I have patients who have been happy following an animal based keto diet, this is their preference, but their LDL-c was not at goal, and it’s my job as a cardiologist to discuss all options.
7/ They can try to transition to a low carb diet that is more plant-predominant, fully plant based (yes this is possible) or Mediterranean style low carb and see if that helps, or if they don’t want to do that, they can start a statin, PCSK9i, etc, to get their LDL-c at goal
8/ You can take any dietary paradigm and make it more CV friendly by reducing SFA, substituting in more plant proteins, increasing fiber intake via whole plant based foods. But at the end of the day, each patient has different needs, interests, tastes and desires.
9/ My goal as a cardiologist is to provide my patients with the best data available: and help them make the decision that is best for them to reduce their risk for atherosclerotic cardiovascular disease.
10/ Although I don’t subscribe to low carb diets personally, it’s not my job to talk someone into our out of something they like. It’s my job to present them with the data we have, and help them to make an informed decision based on risks and benefits, and trial and error.
11/ And that includes giving them accurate information to help them decide what dietary changes or medications they want to pursue to lower their LDL-c, HgbA1c, Blood pressure, waist circumference, and various other risk enhancing factors for ASCVD.
12/ I think it’s about being honest— if a patient wants to continue their preferred eating pattern but their LDL-c is not at goal, then the discussion moves to medication therapy. That is their decision.
13/ And of course sometimes patients who eat even the most perfectly structured plant based diets require medication as well. Medication + lifestyle change need not be a binary recommendation.

14/ But as long as patients know their options - with regards to the potential benefits of trying WFPB or Mediterranean diets, just like we provide options for medications to reduce CV risk, then I think that’s the best we can do.
14/ But as long as patients know their options - with regards to the potential benefits of trying WFPB or Mediterranean diets, just like we provide options for medications to reduce CV risk, then I think that’s the best we can do.
15/ I think patients should get to make the best informed decision possible and understand that there are both lifestyle choices as well as medications that can help them achieve their goals, depending on what works for them.
16/ But where I think many providers need introspection: just because WFPB is “restrictive” to you, doesn’t mean that it will be for every one of your patients. It’s not fair to pre-judge which patients will or will not make aggressive lifestyle interventions, inc dietary change.
17/ Here’s a final anecdote: I had a patient in her 80s with HFpEF come to see me, because she wanted to know if there were any dietary changes she could make to reduce her medications for HTN, HLD, and HFpEF. She disliked taking numerous pills a day and had some unpleasant s/e.
18/ She expressed frustration that numerous other physicians told her “you’re in your 80s, eat whatever you want, it doesn’t make a difference anyway”, and she continuously reiterated that *changing her diet is actually what she wanted* and no one was listening to her.
19/ I took her concerns seriously and she decided she wanted to go ALL in on a WFPB diet. She went from 8 medications down to 2, improved her QOL, and with improved BP control through aggressive lifestyle change - she reduced HFpEF exacerbations ... and hasn’t had one since.
20/ Of course not ALL patients will have these results, and of course not ALL patients will choose to make these changes in their 80s.
21/ But hearing my patients say they can play soccer with their grand kids and walk further than ever with increased QOL after lifestyle changes - is what’s most meaningful to me, but more importantly - what’s most meaningful to them.
22/ So don’t pre judge which of your patients will or will not make a lifestyle change. Provide them with the data, have a patient centered discussion, encourage them in trial and error to find what works for them, and let them make the decision. And support them.
23/ But if you don’t provide information about an option (for ex, WFPB or Med diet) simply because you yourself wouldn’t do it - it’s not fair to make that decision for your patient. They should get to decide what’s best for them after being presented all of the options available

 Read on Twitter
Read on Twitter