This is Monica Smith, a 45-year-old Indiana woman who was in a serious car wreck in 2016.
She had health insurance. The hospital refused to bill it, instead pursuing her for $12,856.
How'd that happen?
Her story is the wildest medical bill saga I've seen in months. (1/13)
She had health insurance. The hospital refused to bill it, instead pursuing her for $12,856.
How'd that happen?
Her story is the wildest medical bill saga I've seen in months. (1/13)
When Monica Smith was taken by ambulance to Parkview Hospital, she had Medicaid — the public program that covers low-income Americans. She showed her Medicaid card. The ambulance billed her coverage.
But the hospital refused to — even after she asked multiple times. (2/13)
But the hospital refused to — even after she asked multiple times. (2/13)
They didn't want to bill Medicaid, it turns out, because they wanted to pursue Monica for the full billed charges.
Medicaid tends to pay the lowest amounts. It would have paid $2,500 for Monica's care.
But the billed charges would bring in 5x more — $12,856, to be exact. (3/13)
Medicaid tends to pay the lowest amounts. It would have paid $2,500 for Monica's care.
But the billed charges would bring in 5x more — $12,856, to be exact. (3/13)
I had assumed, even after a decade of health reporting, that of course a hospital would bill your health coverage if you told them about it.
Well, I was wrong!
When a patient is involved in an accident, many hospitals will refuse to bill insurance. (4/13)
Well, I was wrong!
When a patient is involved in an accident, many hospitals will refuse to bill insurance. (4/13)
Instead, they will try to claim their full billed charges from the patient's auto accident settlement.
The consequence of this is the price of your health care can double, or triple — or in Monica's case go up 5x — when you lose your insurer-negotiated discounts.
Ouch. (5/13)
The consequence of this is the price of your health care can double, or triple — or in Monica's case go up 5x — when you lose your insurer-negotiated discounts.
Ouch. (5/13)
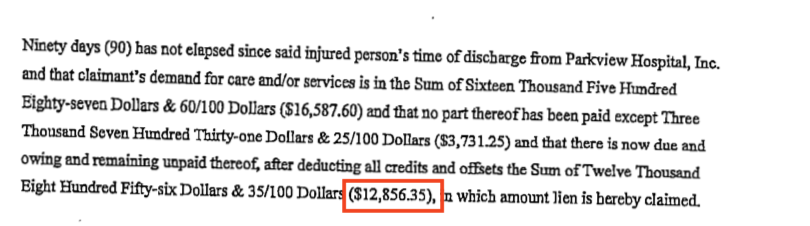
They do this using a lien — essentially, a claim on some property or money you have to ensure they get repaid. This is what the lien Parkview filed against Monica looked like. (6/13)
Monica didn't think this was right. Neither did other Medicaid patients.
So, they sued Parkview. They were suing for the right to have their health insurance billed. (7/13)
So, they sued Parkview. They were suing for the right to have their health insurance billed. (7/13)
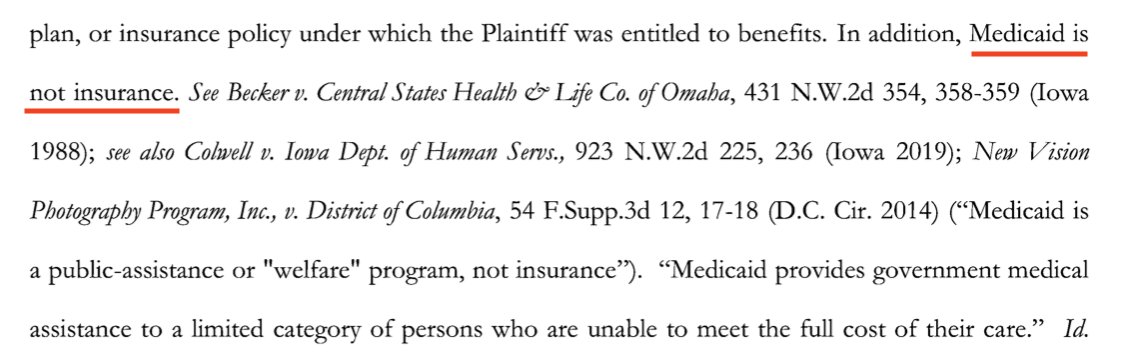
Here's where things get especially wild — the hospital responded by saying it didn't have to bill Monica's Medicaid, because Medicaid isn't health insurance. (8/13)
Here's the legal brief:
https://public.courts.in.gov/mycase#/vw/CaseSummary/eyJ2Ijp7IkNhc2VUb2tlbiI6Ik40UXhkSTdRUGVUYm9oTk0yMVZDbUR2VEVkbXZBeE1RNWJraTZxTFk3OEExIn19
Here's the legal brief:
https://public.courts.in.gov/mycase#/vw/CaseSummary/eyJ2Ijp7IkNhc2VUb2tlbiI6Ik40UXhkSTdRUGVUYm9oTk0yMVZDbUR2VEVkbXZBeE1RNWJraTZxTFk3OEExIn19
They go on to argue that billing Medicaid would cut against the public policy goals of Medicaid — which is not health coverage, but rather teaching people responsibility and self-reliance.
Again, a bit from the legal brief: (9/13)
Again, a bit from the legal brief: (9/13)
The judge did not buy this argument. He found that Medicaid is, in fact, health insurance and that the hospital had to bill it.
Monica got her settlement nearly 4 years after the wreck. (10/13)
Monica got her settlement nearly 4 years after the wreck. (10/13)
How'd this all happen?
It all comes down to century-old hospital lien laws, which give hospitals special privileges to collect their debt.
These laws were written in an era when only 10 percent of Americans had coverage, to ensure providers get paid for medical care (11/13)
It all comes down to century-old hospital lien laws, which give hospitals special privileges to collect their debt.
These laws were written in an era when only 10 percent of Americans had coverage, to ensure providers get paid for medical care (11/13)
In today's @nytimes, @jbsgreenberg and I look into how modern day hospitals are using these laws to profit from low-income patients.
It's not just Monica — this is happening all over the country. You can read more about it here: (12/13) https://www.nytimes.com/2021/02/01/upshot/rich-hospitals-profit-poor.html?action=click&module=News&pgtype=Homepage
It's not just Monica — this is happening all over the country. You can read more about it here: (12/13) https://www.nytimes.com/2021/02/01/upshot/rich-hospitals-profit-poor.html?action=click&module=News&pgtype=Homepage
Has this happened to you? Tell us about it! You can always reach me at sarah.kliff@nytimes with your forays into the wild world of medical billing.
Patient tips are often how these stories get started. I'd love to hear from you (13/13)
Patient tips are often how these stories get started. I'd love to hear from you (13/13)

 Read on Twitter
Read on Twitter