Our new pub in Diabetes Care is out:
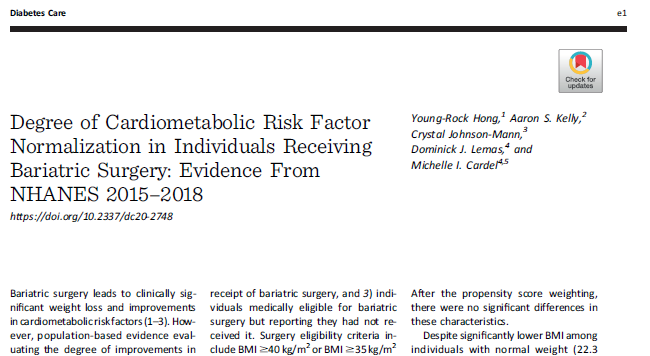
Degree of Cardiometabolic Risk Factor Normalization in Individuals Receiving Bariatric Surgery: NHANES 2015–2018
A thread below of findings, relevant to #obesity, cardiometabolic disease, #nutrition & #HAES
Degree of Cardiometabolic Risk Factor Normalization in Individuals Receiving Bariatric Surgery: NHANES 2015–2018
A thread below of findings, relevant to #obesity, cardiometabolic disease, #nutrition & #HAES
Using nationally representative NHANES data from 2015-2018, we examined cardiometabolic risk factors among individuals who had undergone bariatric surgery, those eligible but had not received bariatric surgery, & medically-classified normal weight adults. https://care.diabetesjournals.org/content/early/2021/01/08/dc20-2748
Methods:
 6,274 participants
6,274 participants
 Mean age 49.8
Mean age 49.8
 55.4% women
55.4% women
 64.9% White
64.9% White
Categories:
 2.1% received bariatric surgery
2.1% received bariatric surgery
 43% were eligible for bariatric surgery but did not receive
43% were eligible for bariatric surgery but did not receive
 54.9% had "normal weight'
54.9% had "normal weight'
 6,274 participants
6,274 participants Mean age 49.8
Mean age 49.8 55.4% women
55.4% women 64.9% White
64.9% WhiteCategories:
 2.1% received bariatric surgery
2.1% received bariatric surgery 43% were eligible for bariatric surgery but did not receive
43% were eligible for bariatric surgery but did not receive 54.9% had "normal weight'
54.9% had "normal weight'
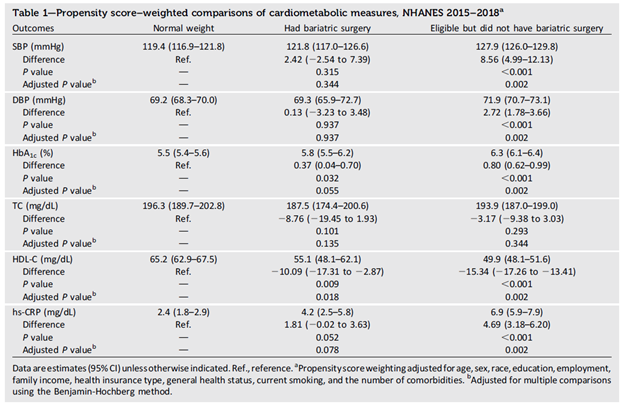
Key Findings: Despite significantly lower weight among 'normal weight' adults (BMI 22.3) compared to those receiving bariatric surgery (BMI 34.9), significant differences were not observed between the two groups for blood pressure, hemoglobin A1c, triglycerides, or CRP.
Key Findings: Conversely, those eligible but not receiving bariatric surgery (mean BMI of 36.8), had significantly higher levels of blood pressure, hemoglobin A1c, and CRP and lower HDL.
Key Takeaways: Despite having BMI values in the 'obesity' range, those who had received bariatric surgery had cardiometabolic risk profiles that largely mirrored that of their 'normal weight' counterparts.
Key Takeaways: Those who had received bariatric surgery had a mean BMI of 35 and those eligible for bariatric surgery but did not receive it had a mean BMI of 37. Yet, the cardiometabolic profile of those receiving surgery was significantly better than those without surgery.
Thus, even in absence of a 'normal weight' BMI following bariatric surgery, cardiometabolic profile is much improved, suggesting bariatric surgery can result in clinically significant improvements in cardiometabolic risk roughly equivalent to 'lean' despite residual adiposity.
I think this is important to note for #HAES, as we are seeing a lot of argument that all adverse cardiometabolic outcomes resulting from obesity are from weight stigma alone, rather any than directly from excess adiposity.
This data supports that even in the absence of differences in weight stigma (likely not much difference in weight stigma experience at BMI of 35 vs BMI of 37), undergoing evidence-based obesity treatment such as bariatric surgery is effective for reducing cardiometabolic risk.
Biggest Key Takeaway taken from overall literature: As healthcare providers and researchers, we need to continue to fight weight stigma, focus on the whole health of patients (not just physical health), and provide access to evidence-based obesity care for pts who seek it.
This project was the culmination of a great team at @UF and @CPOMUMN including lead author @YoungRock_H and study team members @CJMannMD @dominicklemas.

 Read on Twitter
Read on Twitter