Them: So what do you do?
Me: Well, I listen to people die for a living.
Them:
Me: Well, I listen to people die for a living.
Them:
If only I were kidding, sorta. But - critically - I also listen to people being brought back to life. Plus, it's all in the name of saving more lives moving forward.
And who can't get behind that?
And who can't get behind that?
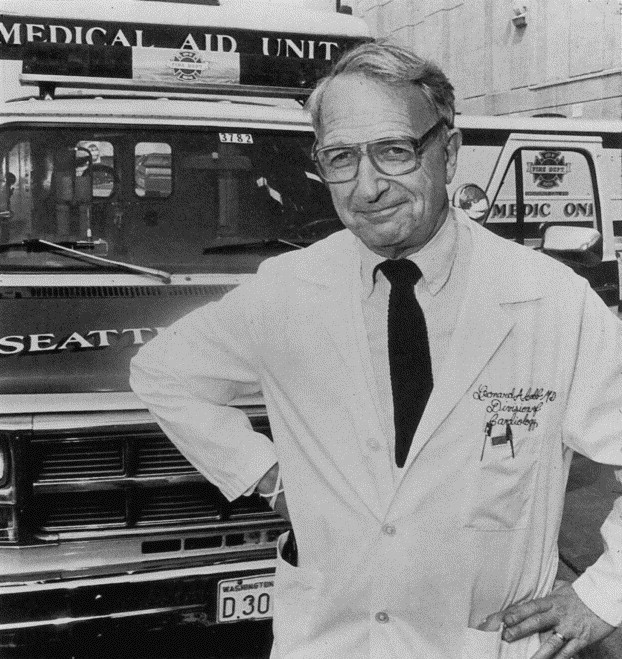
When I was hired by #UWashEMS I inherited the oldest OHCA database in the world.
Named after Dr. Leonard Cobb, @UWMedicine has reviewed every cardiac arrest treated by @SeattleFire since Seattle Medic One started in 1969. https://www.resuscitationjournal.com/article/S0300-9572(02)00146-6/fulltext
Named after Dr. Leonard Cobb, @UWMedicine has reviewed every cardiac arrest treated by @SeattleFire since Seattle Medic One started in 1969. https://www.resuscitationjournal.com/article/S0300-9572(02)00146-6/fulltext
With great (volumes of) data, comes great responsibility. My job is to not break what's not broken, while putting my millennial spin on its infrastructure, collection, and cleaning.
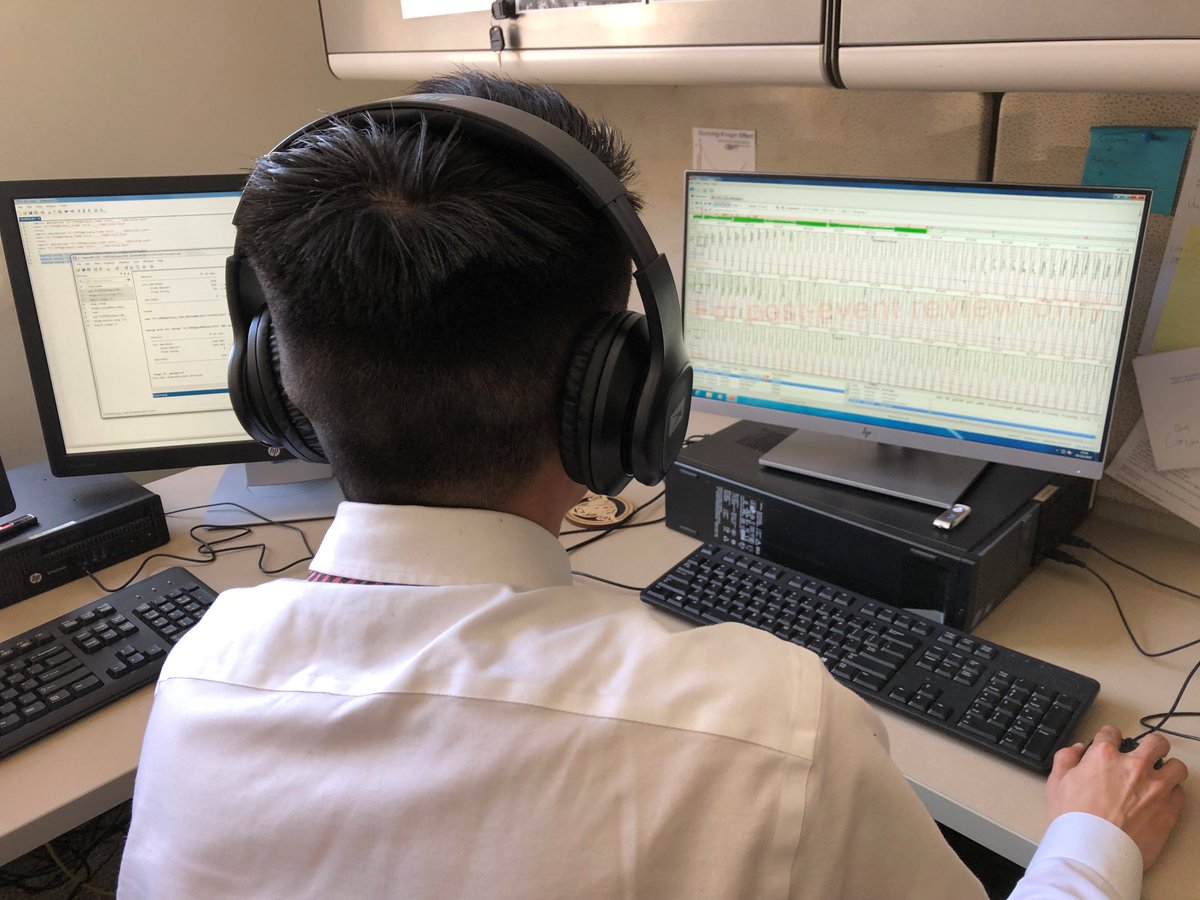
Lots of data elbow grease (Team @Stata) and lots of old coding syntax. https://twitter.com/CatherineCounts/status/1351764036484886529?s=20
Lots of data elbow grease (Team @Stata) and lots of old coding syntax. https://twitter.com/CatherineCounts/status/1351764036484886529?s=20
How does this operationalize? Each morning my team reviews the cardiac arrests from the previous 24 hours to make sure we have the medical record, the defibrillator file(s), and any other details we need to track cases moving forward.
There is no database without raw data.
There is no database without raw data.
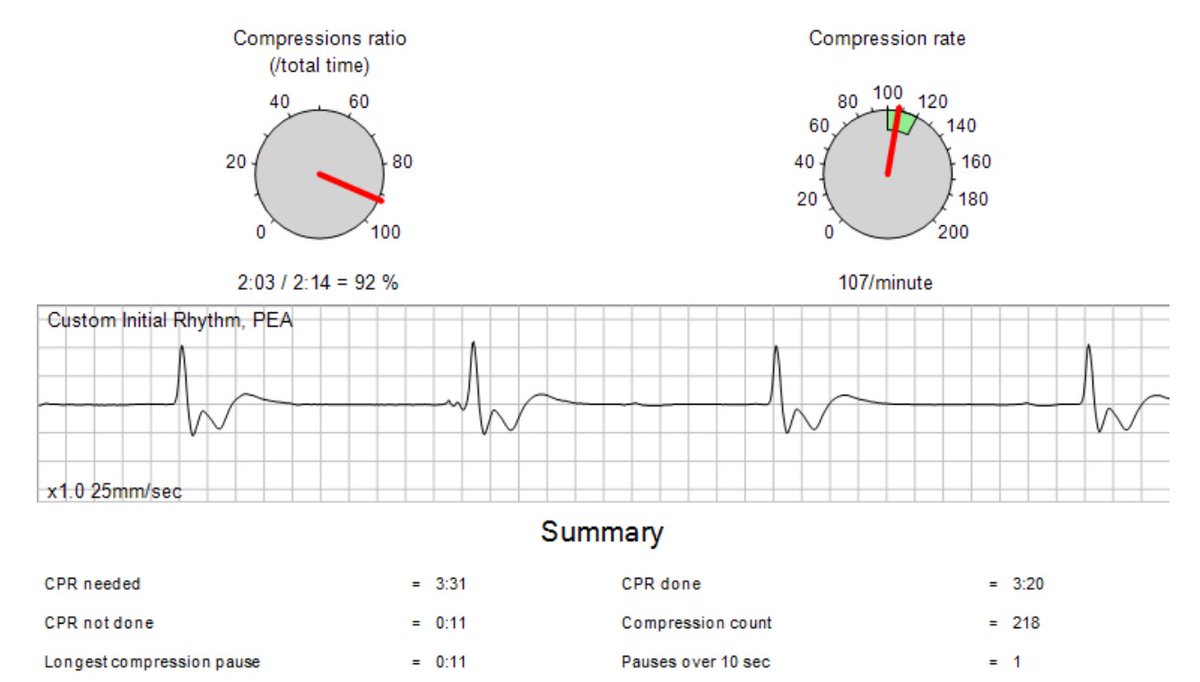
Then we listen to the recording of the case (black box audio in the defibrillator) while coding the times of events and interventions.
We also mark things like pauses in CPR and when the patient got a pulse back.
We also mark things like pauses in CPR and when the patient got a pulse back.
Pre COVID - these process measures were shared with the crews that took care of the patient as well as the patient's outcomes if they made it to the hospital.
Post COVID - I'm still trying to figure out how to close the feedback loop with everything else going on.
Post COVID - I'm still trying to figure out how to close the feedback loop with everything else going on.
From the time an OHCA case is received to the time it is "locked" in our database it's reviewed no less than 3 times:
1) Initial QI Pass
2) Deep data dive
3) Final review by group
I take the accuracy of our OHCA data *very* seriously.
1) Initial QI Pass
2) Deep data dive
3) Final review by group
I take the accuracy of our OHCA data *very* seriously.
We apply similar processes of data collection to advanced airway management, the thought is, that if we're going to take away a patient's ability breathe (a la "rapid sequence intubation") we should make sure we're doing it well and not causing harm. https://litfl.com/rapid-sequence-intubation-rsi/
For OHCAs that receive an advanced airway during care they actually get a fourth review specifically targeted to the airway management of the case.
Like I said, *very* seriously.
Like I said, *very* seriously.
Our third program that gets intensive case-by-case review is whole blood, as this is brand new to the EMS setting, and because of the oversight involved, it's critical that we make sure all the potential pitfalls are ironed out.
Now, if I told you beyond the above I spend 6-8 hours on Zoom per day would anyone be surprised?
The real question is if I spend all my time on Zoom, when do I get the real work done?
Answer: On Zoom (90's kids will get the gif)
The real question is if I spend all my time on Zoom, when do I get the real work done?
Answer: On Zoom (90's kids will get the gif)
The key is that all my Zooming is the key to my research offices' success, we collaborate with outside researchers on nearly all of our projects.
First and foremost, our relationship with King County EMS ( @KCPubHealth). As EMS is primarily funded by a county-wide levy, we collectively report EMS statistics each year, importantly including OHCA survival. https://www.kingcounty.gov/depts/health/emergency-medical-services/reports.aspx
This collaboration between KCEMS and #UWashEMS has resulted in decades of successful research projects.
I don't have favorites...but our recent look at do not attempt resuscitation orders during OHCA is near and dear to my heart. https://twitter.com/UWashEM/status/1330261024906371074?s=20
I don't have favorites...but our recent look at do not attempt resuscitation orders during OHCA is near and dear to my heart. https://twitter.com/UWashEM/status/1330261024906371074?s=20
Since #COVID19 our collaboration has only increased as we work to implement testing sites and vaccination programs, all while using data to inform EMS provider exposures.
If I'm proud of anything it's all the behind the scenes stuff we've done.
If I'm proud of anything it's all the behind the scenes stuff we've done.
Want to dig deep on our #COVID19 EMS research, here's our current publications:
Keep doing bystander CPR: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.048951
Epidemiology of patients seen by EMS: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2767993
PPE Works: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7507417/
Keep doing bystander CPR: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.048951
Epidemiology of patients seen by EMS: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2767993
PPE Works: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7507417/
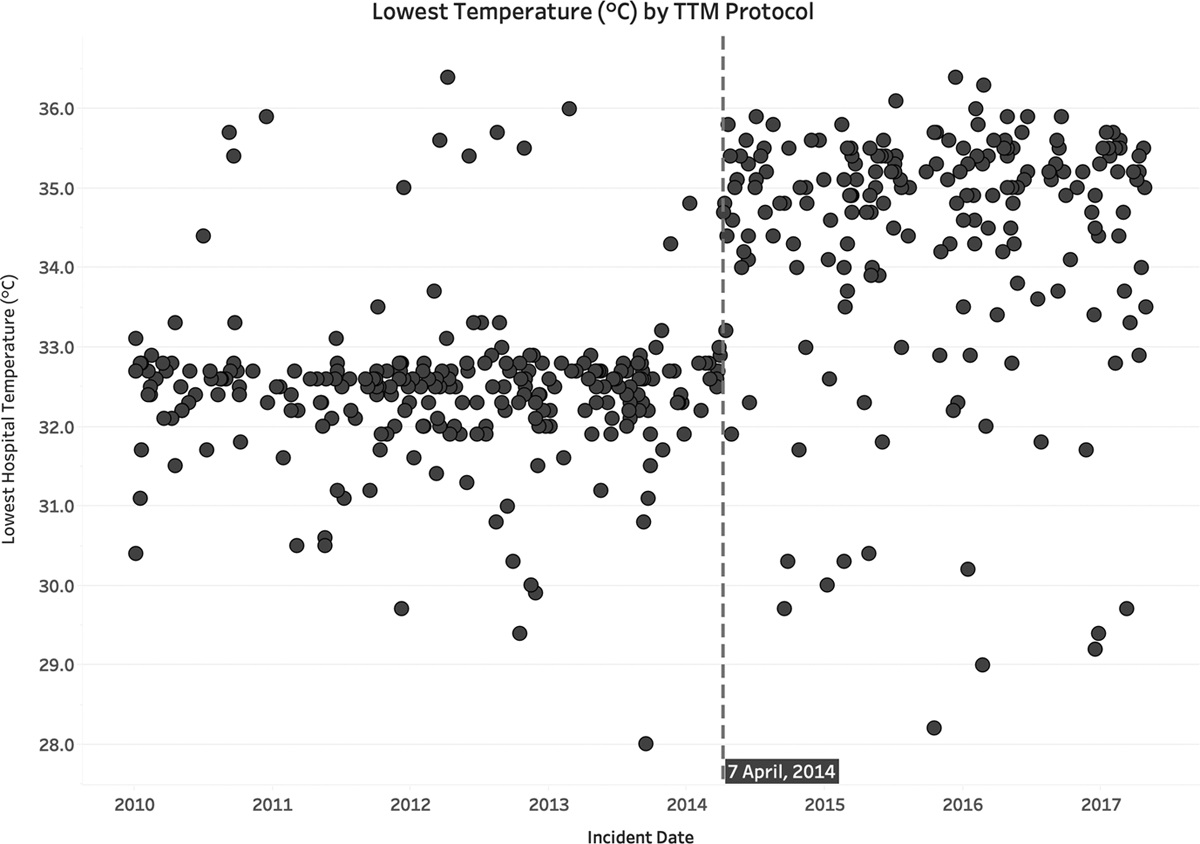
Because we're full of EM physicians at @UWashEM, we collaborate with our @uwpccm (ICU) compatriots quite often.
High on our list of topics: targeted temperature management (cooling to body to help the brain heal post OHCA). https://journals.lww.com/ccmjournal/Fulltext/2020/03000/Targeted_Temperature_Management_at_33_Versus_36.10.aspx
High on our list of topics: targeted temperature management (cooling to body to help the brain heal post OHCA). https://journals.lww.com/ccmjournal/Fulltext/2020/03000/Targeted_Temperature_Management_at_33_Versus_36.10.aspx
And then there's the random chances (mid-pandemic) when we get to try a new device in black box mode to see if it measures what they say it's going to measure and make sure it doesn't break in the EMS setting.
If it works, next stop interventional trial. https://twitter.com/CatherineCounts/status/1340103779660644352?s=20
If it works, next stop interventional trial. https://twitter.com/CatherineCounts/status/1340103779660644352?s=20
So what does a day in the life look like? No clue.
But it revolves around the central construct that data becomes information.
Information becomes knowledge.
And with more knowledge, the better we get at improving care.
But it revolves around the central construct that data becomes information.
Information becomes knowledge.
And with more knowledge, the better we get at improving care.

 Read on Twitter
Read on Twitter