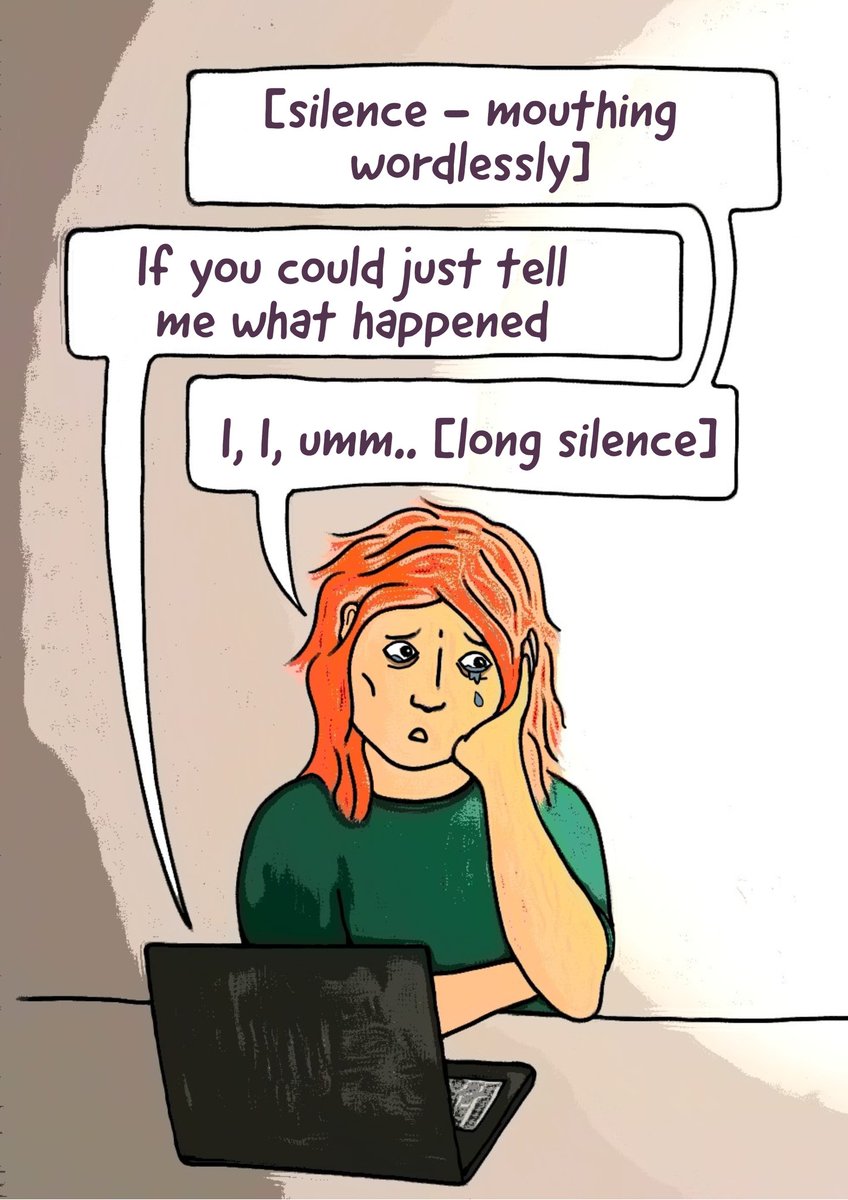
Illustrated direct quotes from my MH appointments #6
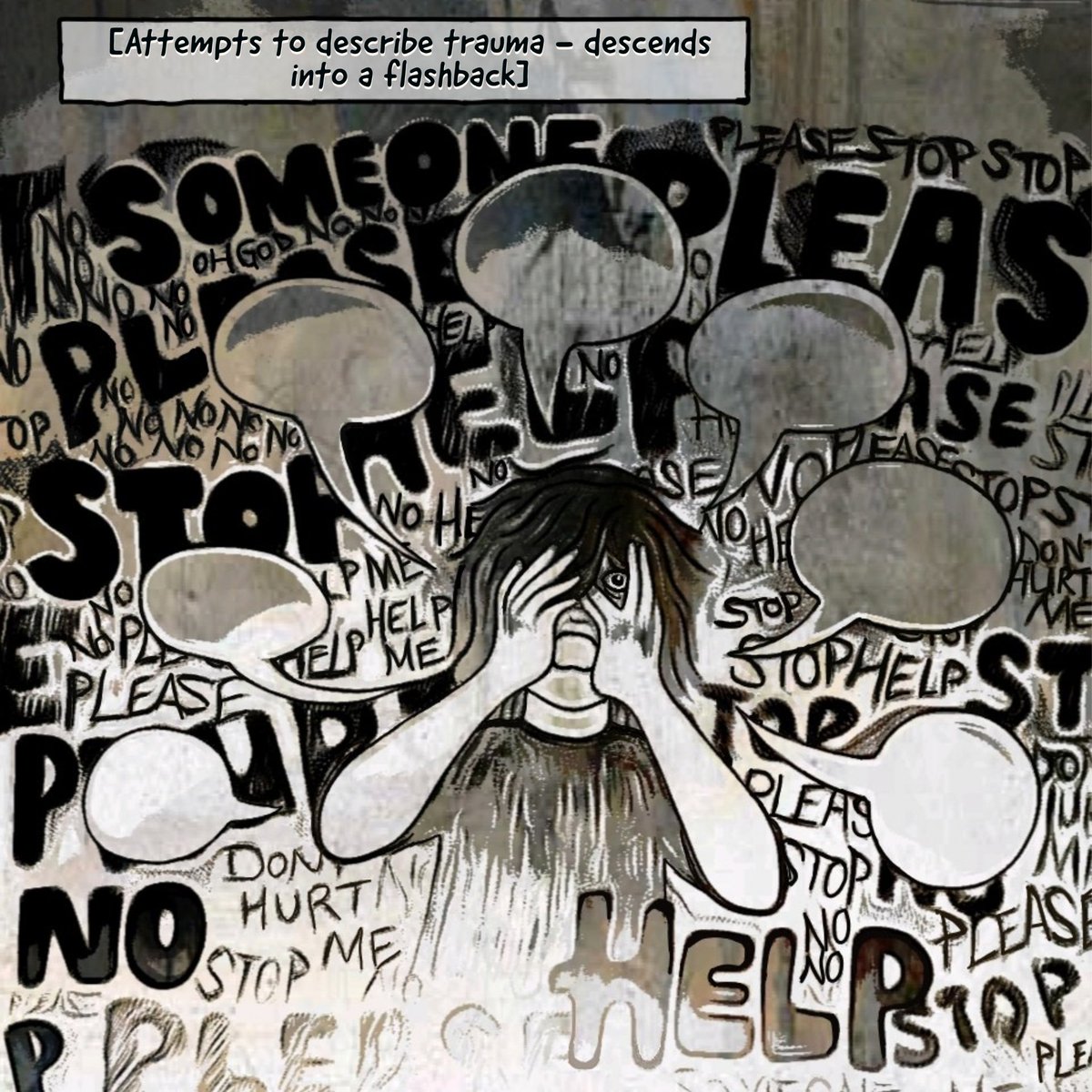
The (commonly denied) power imbalance in MH staff-patient relationships can make it impossible for patients to assert their needs. In this appointment I was pushed too far to disclose a trauma & was blamed for not saying no.
The (commonly denied) power imbalance in MH staff-patient relationships can make it impossible for patients to assert their needs. In this appointment I was pushed too far to disclose a trauma & was blamed for not saying no.
Creating boundaries as a MH patient is *extremely* difficult. Boundaries are often ignored entirely by staff who feel they know best, or who don't recognise how much control they have over an already disempowered person: if we weren't comfortable we would surely say no, right? 2/
Saying no to staff can lead to punishment. Saying no is commonly pathologised: labeled as aggression, unwillingness to engage, trust issues, avoidance etc. Saying no as an inpatient can lead to threats of or actual restraint, being sent to the PICU, being sedated, being 3/
discharged.. etc. When staff refuse to acknowledge their power, patients are both blamed for not asserting themselves & punished when they do.
Being on the losing end of the power dynamic, patients are not always able to communicate that they are uncomfortable, frightened, 4/
Being on the losing end of the power dynamic, patients are not always able to communicate that they are uncomfortable, frightened, 4/
triggered or unable to do something. Abuse dynamics can be recreated for some. Its vital that staff continually ask themselves "Do I really have this person's consent?" "Do they look comfortable with this?" "How can I make it easier for people to communicate their boundaries?"5/5

 Read on Twitter
Read on Twitter