THREAD: A basic understanding of the pathophysiology behind ‘Happy Hypoxemia’ in the context of Covid-19 and prehospital management .. (my first thread so be nice) .. #FOAMed #COVID19 #happyhypoxia /8
What is Happy Hypoxia?
A term coined by clinicians to describe patients w/ extraordinarily low blood-O2 levels who appear in next to no respiratory discomfort and are walking and talking (Couzin-Frankel, 2020).
This phenomenon has been noticed in the context of Covid-19.
A term coined by clinicians to describe patients w/ extraordinarily low blood-O2 levels who appear in next to no respiratory discomfort and are walking and talking (Couzin-Frankel, 2020).
This phenomenon has been noticed in the context of Covid-19.
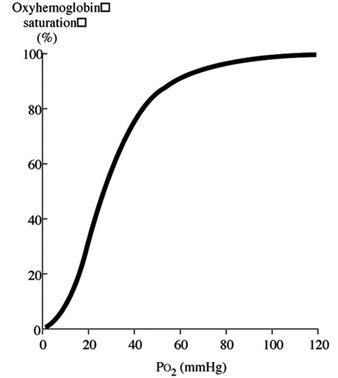
To understand why this happens we must first visit the Oxyhaemoglobin disassociation curve (ODC)
The curve has a sigmoid shape due to the varying affinities of each heme group for O2.
Ie; when O2 binds to the first group, the affinity for the second is enhanced and so on..
The curve has a sigmoid shape due to the varying affinities of each heme group for O2.
Ie; when O2 binds to the first group, the affinity for the second is enhanced and so on..
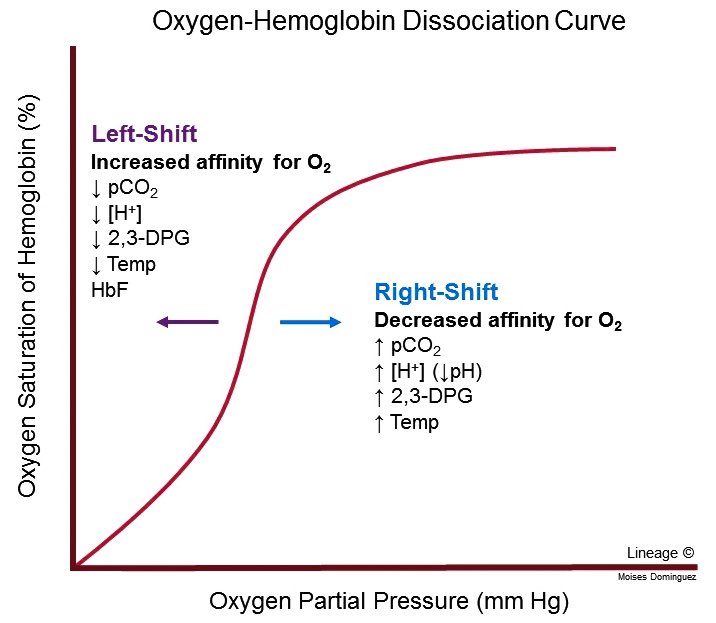
There are factors that cause the ODC to shift to the left ( O2 affinity) or shift to the right (
O2 affinity) or shift to the right ( O2 affinity).. these are:
O2 affinity).. these are:
-CO2
-pH
-temp
In the context of Covid-19 patients we predominately look at Carbon dioxide concentration..
 O2 affinity) or shift to the right (
O2 affinity) or shift to the right ( O2 affinity).. these are:
O2 affinity).. these are:-CO2
-pH
-temp
In the context of Covid-19 patients we predominately look at Carbon dioxide concentration..
In Covid-19 patients, their RR is as important as their SPO2 reading:
Tachypnoea causes respiratory alkalosis due to hypocapnia ( pCO2) which as mentioned above, causes a left shift of the ODC, thus
pCO2) which as mentioned above, causes a left shift of the ODC, thus  the Hb’s affinity for the O2 available..
the Hb’s affinity for the O2 available..
This is why they cope so well..
Tachypnoea causes respiratory alkalosis due to hypocapnia (
 pCO2) which as mentioned above, causes a left shift of the ODC, thus
pCO2) which as mentioned above, causes a left shift of the ODC, thus  the Hb’s affinity for the O2 available..
the Hb’s affinity for the O2 available..This is why they cope so well..
..they cope well until they deteriorate (rapidly).
As the disease progresses the consolidated airspaces don’t inflate as easily, lung compliancy and
lung compliancy and  work of breathing.
work of breathing.
Physiological dead space also increases due to poor blood flow caused by intravascular thrombi ..
As the disease progresses the consolidated airspaces don’t inflate as easily,
 lung compliancy and
lung compliancy and  work of breathing.
work of breathing.Physiological dead space also increases due to poor blood flow caused by intravascular thrombi ..
As well as disease severity, deterioration is caused by the host response and/or suboptimal management..
Prehospitally we can:
-give 15L O2 via non rebreather which can be upto 90% O2
-reassure and anxiety
anxiety
-get the patient to hospital for CPAP or other forms of ventilation
Prehospitally we can:
-give 15L O2 via non rebreather which can be upto 90% O2
-reassure and
 anxiety
anxiety-get the patient to hospital for CPAP or other forms of ventilation
References:
https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-020-01462-5
https://pubmed.ncbi.nlm.nih.gov/32123994/
Despopoulos et al (2009). Color atlas of physiology (Vol. 5)
Any comments / learning points appreciated! Please excuse any mistakes and my limited knowledge of physiology (shouldve listened more in A level Bio!)
https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-020-01462-5
https://pubmed.ncbi.nlm.nih.gov/32123994/
Despopoulos et al (2009). Color atlas of physiology (Vol. 5)
Any comments / learning points appreciated! Please excuse any mistakes and my limited knowledge of physiology (shouldve listened more in A level Bio!)


 Read on Twitter
Read on Twitter