Hot off the press 
Results from our RCT of continuing vs. discontinuing ACEIs vs. ARBs in patients hospitalized with #COVID19!
w/co-PI @JulioChirinosMd in @LancetRespirMed
http://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30558-0/fulltext
#tweetorial 1/
1/

Results from our RCT of continuing vs. discontinuing ACEIs vs. ARBs in patients hospitalized with #COVID19!
w/co-PI @JulioChirinosMd in @LancetRespirMed
http://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30558-0/fulltext
#tweetorial
 1/
1/
ACE2, a counterregulatory enzyme in the RAS, is the receptor for SARS-CoV-2 on host cells
Early in the pandemic, a hypothesis emerged that ACEIs & ARBs may COVID-19 risk & severity based on prior data that they *might*
COVID-19 risk & severity based on prior data that they *might*  ACE2 expression/activity
ACE2 expression/activity
https://doi.org/10.1016/s2213-2600(20)30116-8
2/
Early in the pandemic, a hypothesis emerged that ACEIs & ARBs may
 COVID-19 risk & severity based on prior data that they *might*
COVID-19 risk & severity based on prior data that they *might*  ACE2 expression/activity
ACE2 expression/activityhttps://doi.org/10.1016/s2213-2600(20)30116-8
2/
A counter-argument also emerged, based on data from SARS-Cov-1, that  ACE2 may
ACE2 may  the risk of acute lung injury
the risk of acute lung injury
RAS researchers & medical societies reacted, recommending to continue ACEI/ARBs as prescribed pending more data
http://www.nephjc.com/news/covidace2
https://doi.org/10.2215/cjn.03530320
3/
 ACE2 may
ACE2 may  the risk of acute lung injury
the risk of acute lung injuryRAS researchers & medical societies reacted, recommending to continue ACEI/ARBs as prescribed pending more data

http://www.nephjc.com/news/covidace2
https://doi.org/10.2215/cjn.03530320
3/
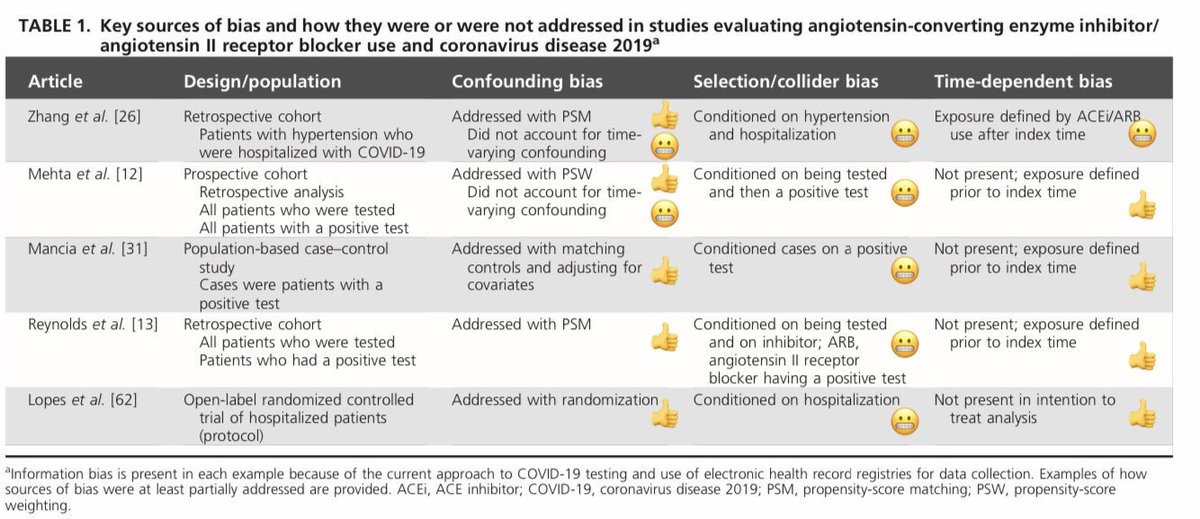
Did we ever get data!
While several trials were underway, >72 observational studies now show no assoc of ACEI/ARBs w/ COVID-19 risk or severity https://doi.org/10.7326/M20-1515
COVID-19 risk or severity https://doi.org/10.7326/M20-1515
But many of these struggled w/bias
@asouth_neph @LucyStats & I reviewed this
https://doi.org/10.1097/hjh.0000000000002706
4/
While several trials were underway, >72 observational studies now show no assoc of ACEI/ARBs w/
 COVID-19 risk or severity https://doi.org/10.7326/M20-1515
COVID-19 risk or severity https://doi.org/10.7326/M20-1515But many of these struggled w/bias
@asouth_neph @LucyStats & I reviewed this

https://doi.org/10.1097/hjh.0000000000002706
4/
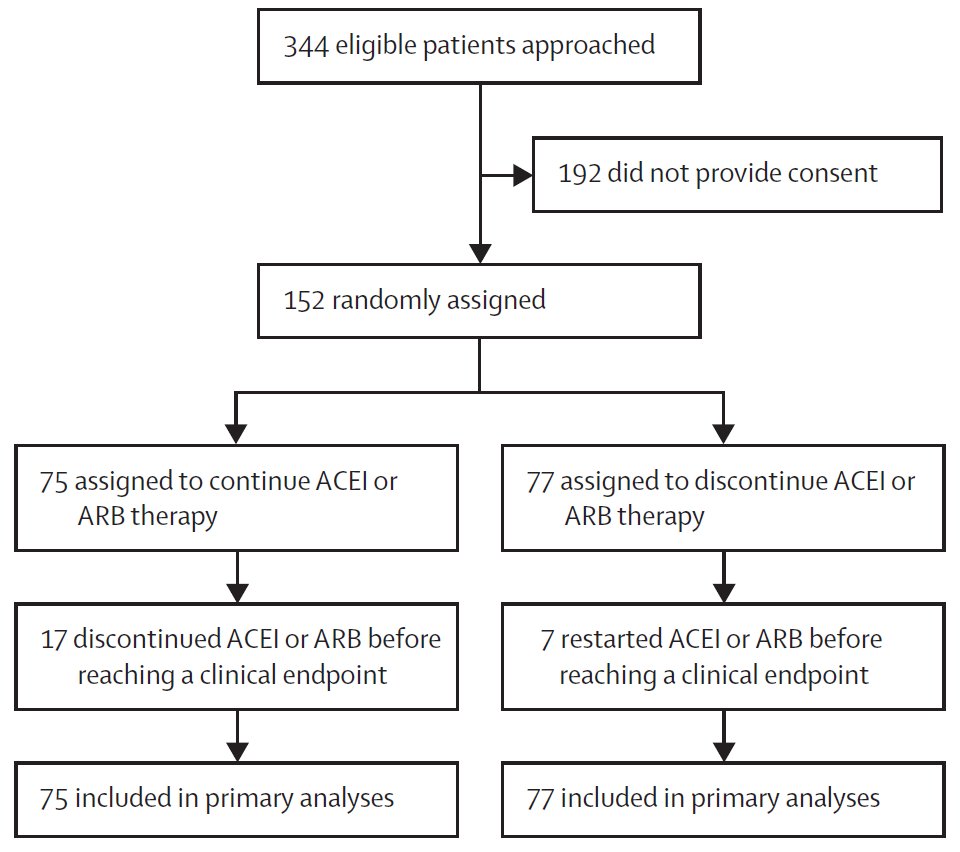
Trial data were needed to answer the question of whether it's safe to continue vs. stop ACEIs & ARBs in patients hospitalized w/COVID-19
Our trial, REPLACE COVID, randomized 152 patients at 20 international centers from March-Aug 2020
Design paper
https://onlinelibrary.wiley.com/doi/full/10.1111/jch.14011
5/
Our trial, REPLACE COVID, randomized 152 patients at 20 international centers from March-Aug 2020
Design paper

https://onlinelibrary.wiley.com/doi/full/10.1111/jch.14011
5/
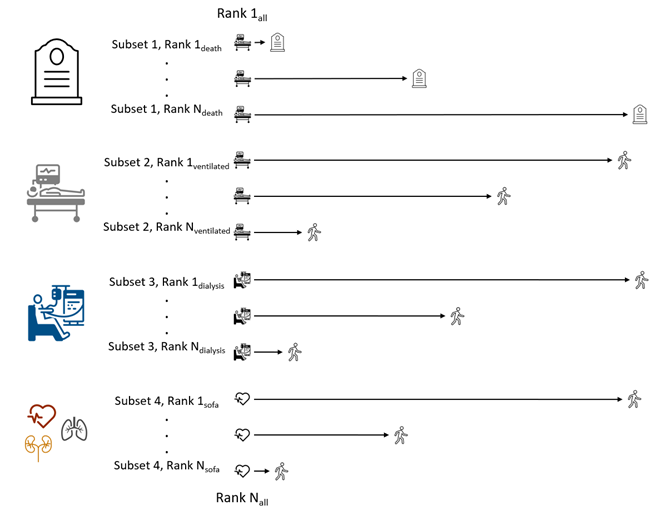
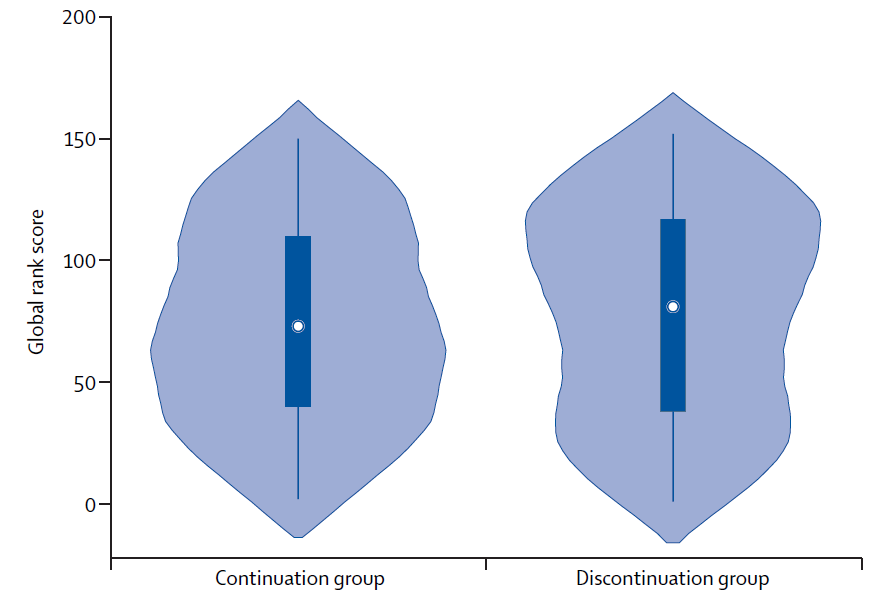
Our primary outcome was a hierarchical global rank score in which patients were ranked from 1-152 by severity of illness by
1) Time to death
2) Duration of invasive mechanical ventilation
3) Duration of vasopressors or renal replacement therapy
4) AUC of a modified SOFA score
6/
1) Time to death
2) Duration of invasive mechanical ventilation
3) Duration of vasopressors or renal replacement therapy
4) AUC of a modified SOFA score
6/
The rank score benefits from higher statistical power compared w/other common approaches & accounts for important factors related to resource use & duration of hospitalization
We observed no difference in median scores btw patients whose ACEIs/ARBs were continued vs. stopped
7/
We observed no difference in median scores btw patients whose ACEIs/ARBs were continued vs. stopped
7/
We also observed no substantial differences in our secondary endpoints, including death, ICU admission or mechanical ventilation, length of hospitalization, &  BP requiring vasopressors
BP requiring vasopressors
And no significant effect modification (though statistical power to look at this)
statistical power to look at this)
8/
 BP requiring vasopressors
BP requiring vasopressors And no significant effect modification (though
 statistical power to look at this)
statistical power to look at this)8/
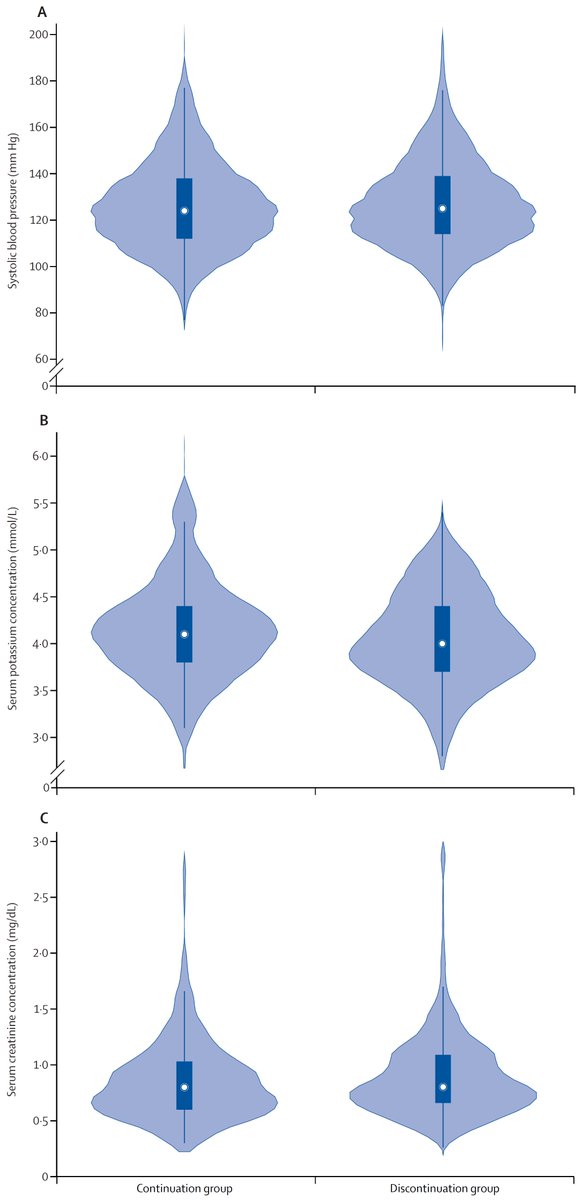
For the nephrology & HTN  's
's
We found no difference in systolic BP, K, & creatinine during follow-up btw groups!
These results were upheld after censoring at the time of crossover btw treatment arms (n=24) & in (unpublished) analyses accounting for time-updated treatment
9/
 's
'sWe found no difference in systolic BP, K, & creatinine during follow-up btw groups!
These results were upheld after censoring at the time of crossover btw treatment arms (n=24) & in (unpublished) analyses accounting for time-updated treatment
9/
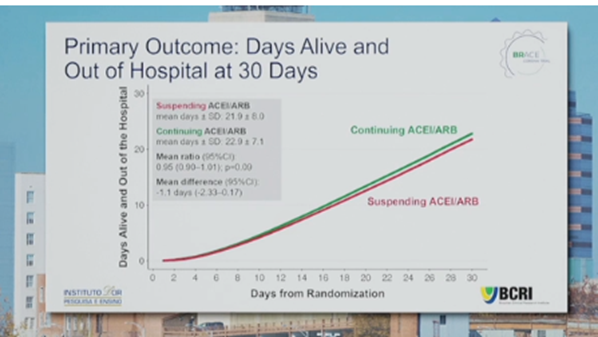
Strengths of our study include that it's the 1st published RCT in this area
BRACE CORONA presented @escardio, not yet published but saw no dif in 30-days alive & out of hospital w/continuing vs. stopping ACEI/ARB, w/some limitations (young, 11% excluded after study started)
10/
BRACE CORONA presented @escardio, not yet published but saw no dif in 30-days alive & out of hospital w/continuing vs. stopping ACEI/ARB, w/some limitations (young, 11% excluded after study started)
10/
Limitations of REPLACE include:
Small sample size (helped by rank score w/ power than common endpoints &
power than common endpoints &  events
events  )
)
Open-label design (some providers may have behaved differently knowing patients' randomization arms; but we made sure endpoint adjudicators were blinded)
11/
Small sample size (helped by rank score w/
 power than common endpoints &
power than common endpoints &  events
events  )
) Open-label design (some providers may have behaved differently knowing patients' randomization arms; but we made sure endpoint adjudicators were blinded)
11/
So, consistent w/society recs & considering the observational evidence, our findings support that ACEIs & ARBs can be safely continued in patients who are hospitalized w/COVID-19
Ongoing studies are evaluating if de novo introduction of ARBs is helpful to treat COVID-19
12/
Ongoing studies are evaluating if de novo introduction of ARBs is helpful to treat COVID-19
12/
Thank you to the amazing REPLACE COVID investigators, who called to arms as the pandemic started here & almost all of whom contributed w/out funding to support this
@TomHanffMD @taraichang @nicolasrennamd @DanEdmonston @thebyrdlab @nicolasrennamd @CarlosAlfonsoMD + many others
@TomHanffMD @taraichang @nicolasrennamd @DanEdmonston @thebyrdlab @nicolasrennamd @CarlosAlfonsoMD + many others
& to the ACE2 working group for all you've done to  increase awareness about relationships b/t ACEI/ARBs, ACE2, & COVID19 via #nephjc
increase awareness about relationships b/t ACEI/ARBs, ACE2, & COVID19 via #nephjc 
http://www.nephjc.com/news/covidace2
Including, not limited to
@hswapnil @Nephro_Sparks @PAWellingMD @Dan_Batlle @LouiseBurrell3 @PepaSolerR @asouth_neph
 increase awareness about relationships b/t ACEI/ARBs, ACE2, & COVID19 via #nephjc
increase awareness about relationships b/t ACEI/ARBs, ACE2, & COVID19 via #nephjc 
http://www.nephjc.com/news/covidace2
Including, not limited to
@hswapnil @Nephro_Sparks @PAWellingMD @Dan_Batlle @LouiseBurrell3 @PepaSolerR @asouth_neph
Editorial puts things in excellent context by the great Bryan Williams 
https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(21)00003-5/fulltext

https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(21)00003-5/fulltext

 Read on Twitter
Read on Twitter