Are we, cardiologists, killing patients over the NYHA score!?
We raise this question - with less drama - in our new @Heart paper. This matters. Here's why.
https://heart.bmj.com/content/early/2020/12/23/heartjnl-2020-317984
We raise this question - with less drama - in our new @Heart paper. This matters. Here's why.

https://heart.bmj.com/content/early/2020/12/23/heartjnl-2020-317984
This is Daniel, your typical heart failure patient. 68 yo man, ejection fraction 25%. Doesn't walk much b/c of hip osteoarthritis, but swears he has no heart symptoms whatsoever.
The 100-year-old, subjective classification would say he's a NYHA I. Apparently ancient Romans agree on this one. https://twitter.com/ProfDFrancis/status/1272246810627670016
How should we treat this fellow?
Guidelines tell us that every single part of option B saves lives. *BUT ONLY* if we call our patient a NYHA II and not a NYHA I.
I or II. This can be blurry.
I or II. This can be blurry.
(I swear that wasn't a trick question.)
But is it easy to tell if a patient like Daniel has NO limitation (NYHA I) or SLIGHT limitation (NYHA II)?
But is it easy to tell if a patient like Daniel has NO limitation (NYHA I) or SLIGHT limitation (NYHA II)?
Daniel's treatment relies on his NYHA score. It depends on the doctor's *subjective* impression about the patient's *subjective* impression of his *subjective* symptoms.
If it seems too subjective to guide huge decisions, it's because it is.
If it seems too subjective to guide huge decisions, it's because it is.
So we wanted to check if there really are *objective* differences between these NYHA I and II patients, that justify their different treatments. https://heart.bmj.com/content/early/2020/12/23/heartjnl-2020-317984
We used ReBIC-II trial data to compare NYHA I vs. II stable outpatients. Few datasets are this detailed.
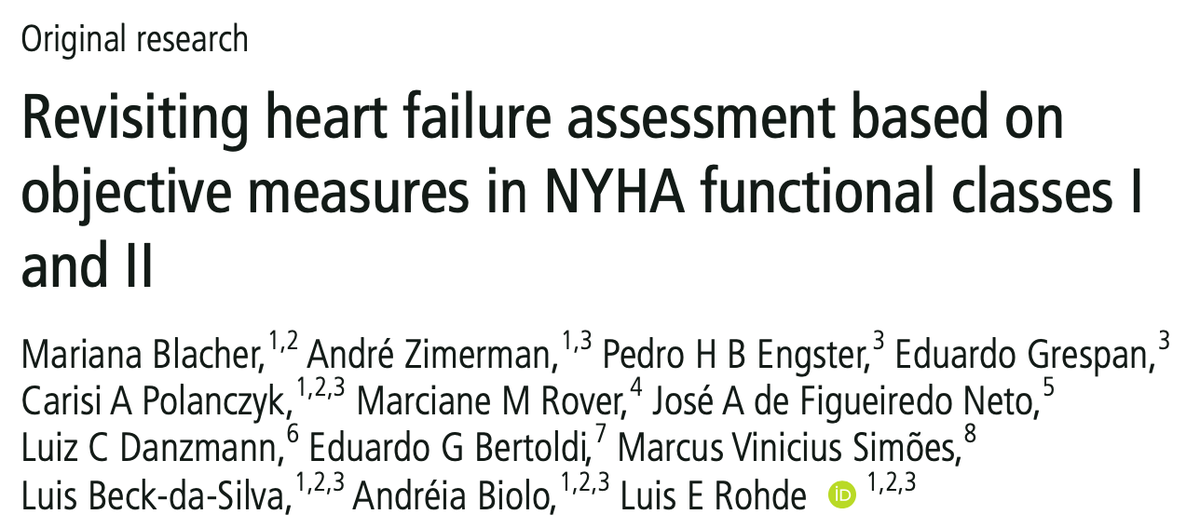
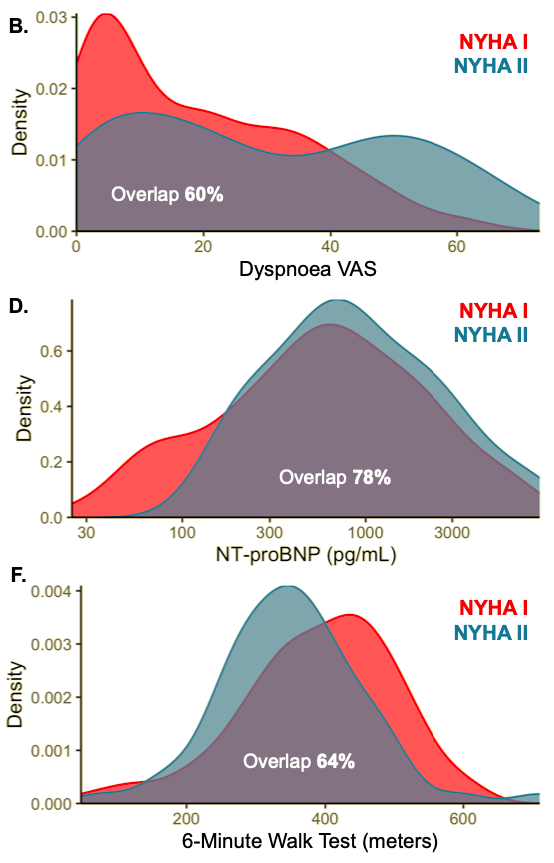
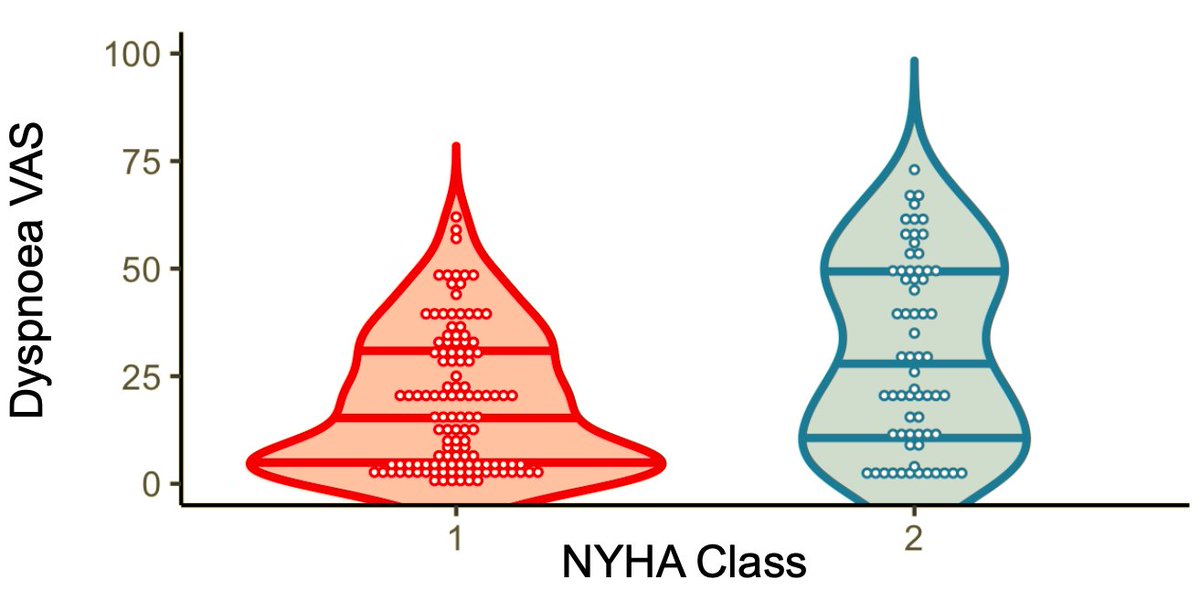
We compared self-assessed dyspnea, NT-proBNP, and 6-minute walk test between NYHA groups.
We compared self-assessed dyspnea, NT-proBNP, and 6-minute walk test between NYHA groups.
Table 1 shows us these patients are much more alike than they are different.
But then it gets (even more) interesting.
But then it gets (even more) interesting.
Is anyone surprised?
If these patients are largely similar, how should their treatments be (at least in theory)?
If we can't trust the NYHA assessment, how can we trust any decisions that rely solely on it?
@fperrywilson is categorical: "We need much better methods" https://twitter.com/fperrywilson/status/1199798412805320709
@fperrywilson is categorical: "We need much better methods" https://twitter.com/fperrywilson/status/1199798412805320709
And until then?
"We shouldn't be using NYHA Class to stratify risk", says @kardiologykazi https://twitter.com/kardiologykazi/status/1300512131335430144
"We shouldn't be using NYHA Class to stratify risk", says @kardiologykazi https://twitter.com/kardiologykazi/status/1300512131335430144
So what did we learn?
 NYHA I and II heart failure patients are similar
NYHA I and II heart failure patients are similar
 NYHA is unreliable, should not define treatment alone
NYHA is unreliable, should not define treatment alone
 We need better methods to stratify and treat our patients
We need better methods to stratify and treat our patients
 NYHA I and II heart failure patients are similar
NYHA I and II heart failure patients are similar NYHA is unreliable, should not define treatment alone
NYHA is unreliable, should not define treatment alone We need better methods to stratify and treat our patients
We need better methods to stratify and treat our patients

 Read on Twitter
Read on Twitter