I've been a hearing a lot about how children are more infectious *now* & contribute to transmission because of the B117 variant, but didn't before. This is a myth. Children & schools have always played an important role in transmission. Time to lay this to rest. Thread.
A few concepts. The role played by children in transmission depends upon 3 factors:
1. Susceptibility (how likely a child is to get infected when exposed)
2. Exposure (how likely a child is to get exposed)
3. Transmissibility (how likey a child is to transmit when infected)
1. Susceptibility (how likely a child is to get infected when exposed)
2. Exposure (how likely a child is to get exposed)
3. Transmissibility (how likey a child is to transmit when infected)
When we measure *infection* rates in children, it's worth remembering that this is a combination of susceptibility AND exposure. For example, children may be *individually less susceptible*, but can still have high rates of *infection* in situations where contact rates are high.
It's worth emphasising this because it's something that's been widely misunderstood by experts, where at point evidence suggestive of lower *susceptibility* has been interpreted as lower *infection* or even more puzzlingly, lower potential for *transmission*.
Transmission from children is a combination of *infection* (a combination susceptibility AND exposure) as well as *transmissibility* and *level of contact with others*. So there is an interplay of many factors that ultimately determine the role children play in transmission.
Different studies have examined different aspects of this. While teasing out these different aspects is important, understanding the role schools play in transmission doesn't require us to tease out these factors.
Studies that have looked at the impact of schools at population level are very clear & consistent in their evidence. I'm going to present just a few here. These are studies that look at the time at which different interventions were carried out & the impact they had on R.
So essentially the association is temporal (based on when schools were closed) & geographical (where they were closed). While this is not strictly causal evidence, seeing this consistent pattern again & again and across multiple countries strongly suggests a causal link.
Here is a study carried out across >200 countries that showed that among all interventions studied, closing educational institutions was the 2nd most effective. Importantly, the impact on R was similar for pre-school, primary & secondary school settings.
https://www.nature.com/articles/s41562-020-01009-0
https://www.nature.com/articles/s41562-020-01009-0
Another study of >131 countries showed that among different interventions studied, one of the highest changes in R (R ratio) between introducing an intervention & lifting it was for school closures:
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30785-4/fulltext
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30785-4/fulltext
Here's a study from the US that linked statewide school closures to *60%* reductions in both new cases of COVID-19 & COVID-19 mortality. https://jamanetwork.com/journals/jama/fullarticle/2769034
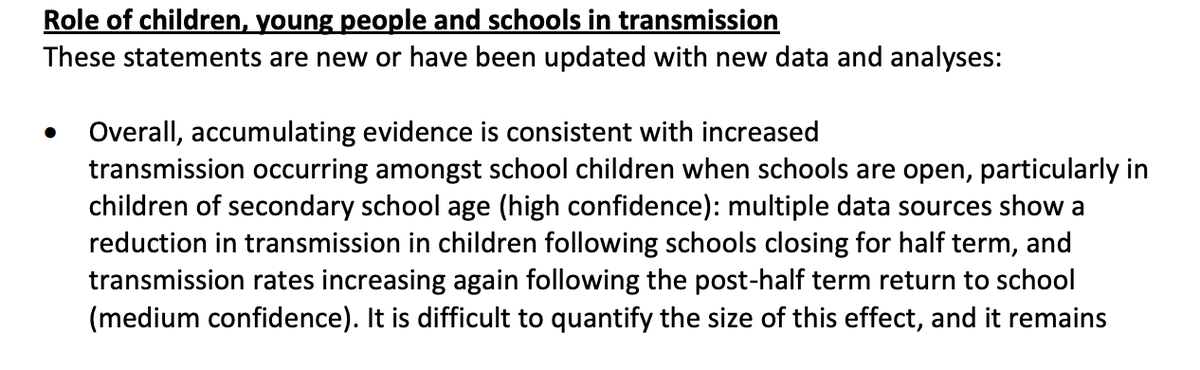
How about England? The recent SAGE report on schools - as many of us reported at the time, SAGE reading of evidence concurs that infection rates among children dropped over half-term & increased again following this in Oct. This is before the new variant was dominant.
Important to note that most of the evidence presented here isn't recent. The important roles schools play in transmission has been known for a long time & pre-dates the emergence of this variant. So how do we explain how this has been so widely misunderstood- even by experts?
There are many reasons for this. Let's look at some.
Studies that have tried to look at susceptibility have often focused on transmission within households. These look at how often children get infected when exposed to an index case (secondary attack rate).
Studies that have tried to look at susceptibility have often focused on transmission within households. These look at how often children get infected when exposed to an index case (secondary attack rate).
Transmissibility studies look at how often children get infected when exposed to an 'index case'.
Most studies looking at both of these use symptom-based testing to determine case status. This is flawed - because children are often asymptomatic & infect adults silently.
Most studies looking at both of these use symptom-based testing to determine case status. This is flawed - because children are often asymptomatic & infect adults silently.
This means contacts of children are often wrongly identified as the index case as initial testing is based on symptoms. If contacts are then tested, it's possible the child would then be considered as a secondary infection, or not infected at all (if swab -ve by this point)
The second issue is that many of earlier studies on infection were carried out during lockdowns & periods where schools were either closed or attendance was much lower. This will have a huge impact on inferences, as infection in children depends on *susceptibiliy* & *exposure*
An example of one such study was the study by PHE that was widely reported, even by experts as evidence that schools didn't contribute significantly to transmission. This study was based on symptom-based testing & carried out when only 7% of children were attending schools.
Another study that provided false assurance (the OpenSAFELY study) suggested that although parents of secondary school children had a significantly higher risk of infection than similarly aged non-parents, the rate of death was similar in both groups.
This study is extremely flawed, and was widely misinterpreted as evidence that school transmission didn't put parents or communities at risk. I've previously explained what the limitations of this study are here. https://twitter.com/dgurdasani1/status/1330447305246470146?s=20
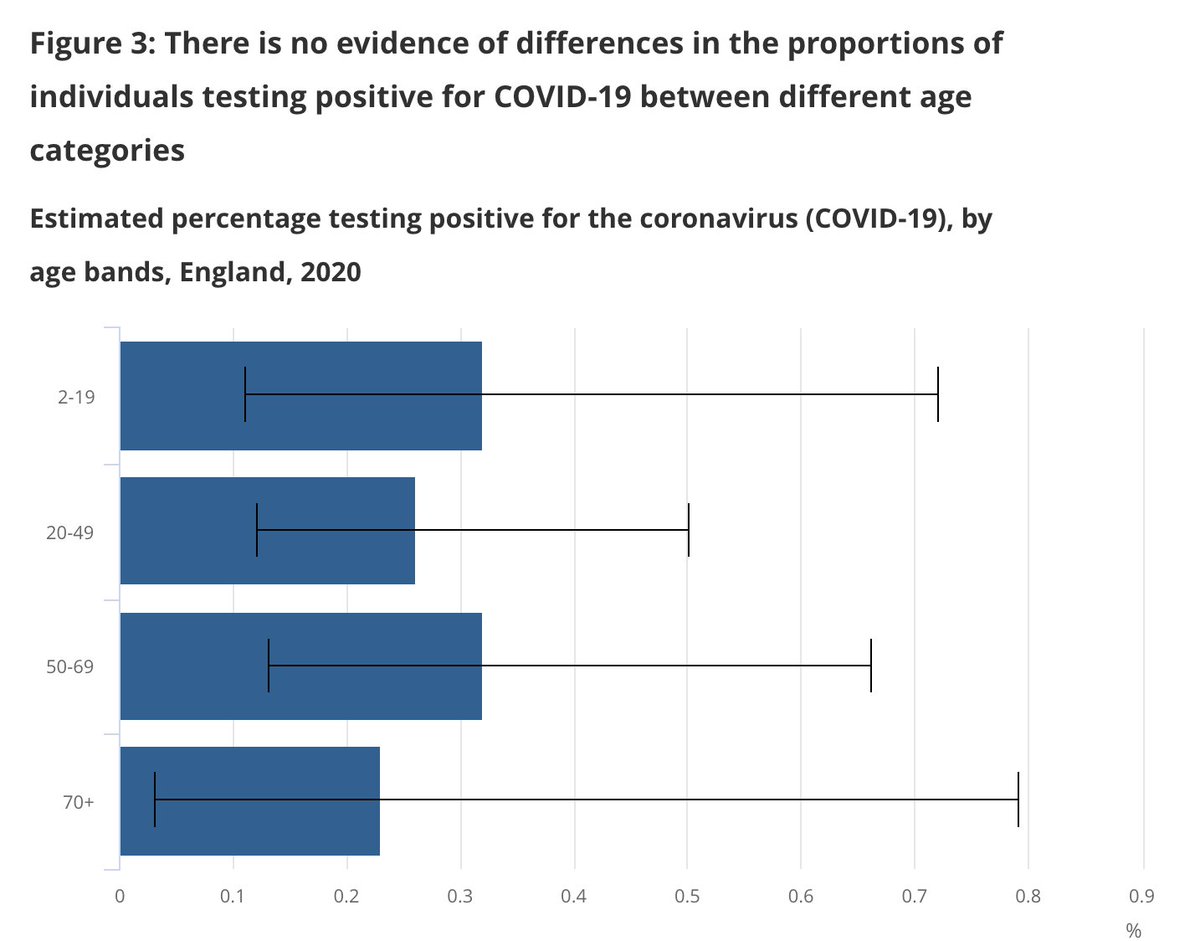
Despite all this, just simple infection prevalence data from the ONS survey very early on showed that in random community testing the infection rates among children were not different from those of adults.
Seroprevalence (antibody) studies have shown mixed results- some showing slightly lower seroprevalence among children or equal (often depending on context- schools open or not).
And we need to remember that this is despite swab and serology being less sensitive in children.
And we need to remember that this is despite swab and serology being less sensitive in children.

 Read on Twitter
Read on Twitter