From this morning’s @westaustralian
Some thoughts on delayed transfer of care - aka ramping - a 

First of all, what are the metrics? Transfer of care (TOC) is the time interval between ambulance arrival at an ED and when that patient is handed over to the care of the ED team - most commonly onto an ED trolley or sometimes to the ED waiting room.
During this time period - arrival to transfer of care, the patient is also seen by the ED triage nurse and allocated an urgency score under the Australasian Triage Scale (ATS) with ATS 1 being the most clinically urgent and ATS 5 being least clinically urgent.
So within the time interval arrival to TOC there are two sub intervals - arrival to triage and triage to TOC.
Still with me?
Still with me?
ACEM - the Australasian College for Emergency Medicine - has a position paper on ambulance ramping - https://tinyurl.com/yxm642p9 .
ACEM notes: Adverse patient outcomes, poor patient experiences and higher health system costs are associated with ambulance ramping.
ACEM notes: Adverse patient outcomes, poor patient experiences and higher health system costs are associated with ambulance ramping.
ACEM go on to say: In a well-functioning system, with good access to cubicles and beds, the time interval of ambulance arrival to clinical handover should routinely occur within 15 minutes and never take more than 30 minutes.
Note the word never.
Note the word never.
Next couple of comments are my opinion, based on working extensively in EDs in Western Australia from 1993 - 2019. I've worked in most places west of a line from Port Hedland to Kalgoorlie.
EDs have always been busy and often overcrowded places. It wasn't until the early to mid
EDs have always been busy and often overcrowded places. It wasn't until the early to mid
2000's that capacity constraints started impacting ambulance patients. At that time, individual EDs would go on "diversion" when over capacity and patients bound for that ED would be taken elsewhere. Diverting patients to other EDs often resulted in that ED becoming overwhelmed
The diversion strategy stopped being useful as the majority of the EDs were busy / overcrowded at any given time, resulting in "triple diversion" of the three biggest EDs in the city which effectively put everyone back to the same status.
Out of this entirely unsatisfactory set
Out of this entirely unsatisfactory set
of circumstances, ambulance ramping was created as a method of coping with the mismatch between ED capacity and the tempo of patient presentations.
It started off being an issue at times of peak activity, particularly in winter, and would defervesce in the warmer months.
It started off being an issue at times of peak activity, particularly in winter, and would defervesce in the warmer months.
Back to facts. In 2013, St John implemented ASCU - the Ambulance Surge Capacity Unit - based at Hollywood Hospital - https://tinyurl.com/yyrcm47r .
This was an attempt by St John to care for patients in a safe environment at times of peak ambulance demand / overcrowding in our EDs.
This was an attempt by St John to care for patients in a safe environment at times of peak ambulance demand / overcrowding in our EDs.
ASCU 1.0 lasted several months.
In 2015, ASCU 2.0 was implemented at SCGH - https://tinyurl.com/y4oxlvwk .
What we found is that the majority of patients taken to ASCU did in fact need assessment in an ED and the strategy was discontinued.
During this period of time, ramping levels
In 2015, ASCU 2.0 was implemented at SCGH - https://tinyurl.com/y4oxlvwk .
What we found is that the majority of patients taken to ASCU did in fact need assessment in an ED and the strategy was discontinued.
During this period of time, ramping levels
were in the order of 400-700 hours per month.
I should also mention that ramping hours on any given day are the sum total of the time taken from 30 minutes after patient arrival at an ED to transfer of care. That is to say, the first 30 minutes does not count. For all patients
I should also mention that ramping hours on any given day are the sum total of the time taken from 30 minutes after patient arrival at an ED to transfer of care. That is to say, the first 30 minutes does not count. For all patients
across the system.
So that's the history lesson people.
So that's the history lesson people.
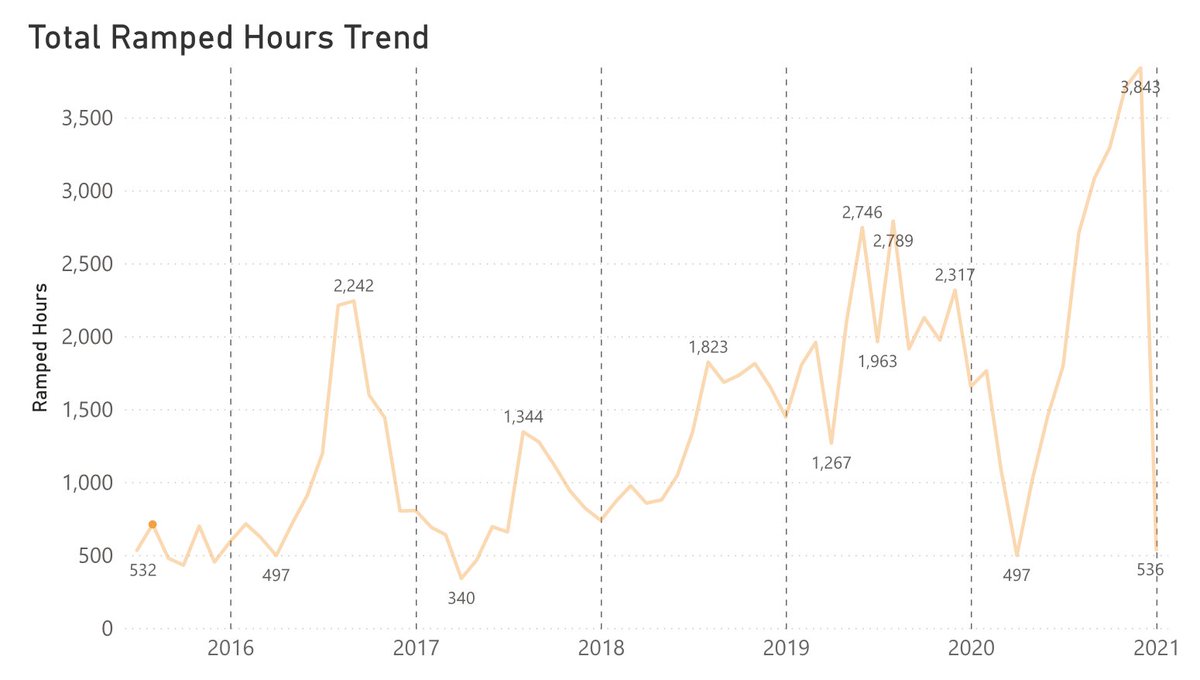
In the middle of 2018, ambulance ramping stopped being seasonal and remained elevated other than a brief period of respite when Western Australia was locked down in the early stages of COVID.
(The January '21 figure is month to date up to the 4/1/21).
(The January '21 figure is month to date up to the 4/1/21).
Prior to 2020, the single worst month for ramping was August 2019 at 2789 hours.
Since September 2020 we have set 4 consecutive monthly records:
Sept 3084 hours
Oct 3292 hours
Nov 3706 hours
Dec 3843 hours
Since September 2020 we have set 4 consecutive monthly records:
Sept 3084 hours
Oct 3292 hours
Nov 3706 hours
Dec 3843 hours
I'm going to leave this part of the thread here for today - I want to take some time to properly consider how best to explain the effects of all of this on our front line clinical staff in Ambulance and most importantly our patients.

 Read on Twitter
Read on Twitter