just because NHS hospital intensive care capacity isn’t technically “full” doesn’t mean that coronavirus patients are getting the level of care they normally would
government data available here shows this (thread) https://www.gov.uk/government/statistics/national-flu-and-covid-19-surveillance-reports
government data available here shows this (thread) https://www.gov.uk/government/statistics/national-flu-and-covid-19-surveillance-reports
there is some public awareness that there’s been a drop in the normal levels of NHS care, as emails leak from London hospitals talking of “disaster medicine mode” and saying that “high standard critical care” is no longer possible due to service overload https://twitter.com/paulbranditv/status/1344701745130254343
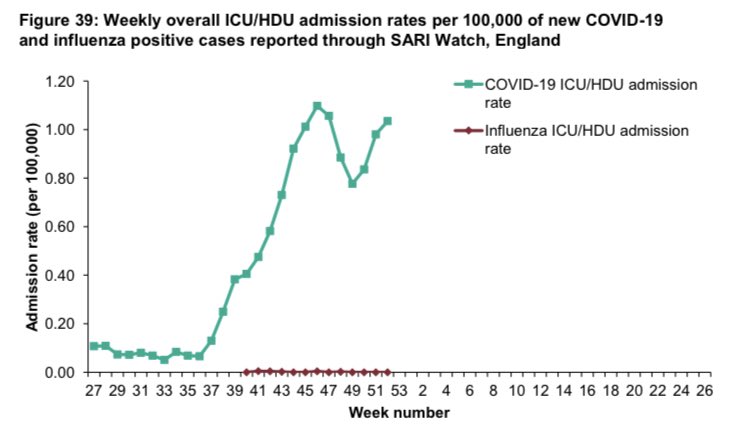
the reality is the COVID pressure on NHS intensive care had already markedly increased across the whole of England even during November, as this graph from the latest PHE report shows
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/948638/Weekly_Flu_and_COVID-19_report_w53.pdf
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/948638/Weekly_Flu_and_COVID-19_report_w53.pdf
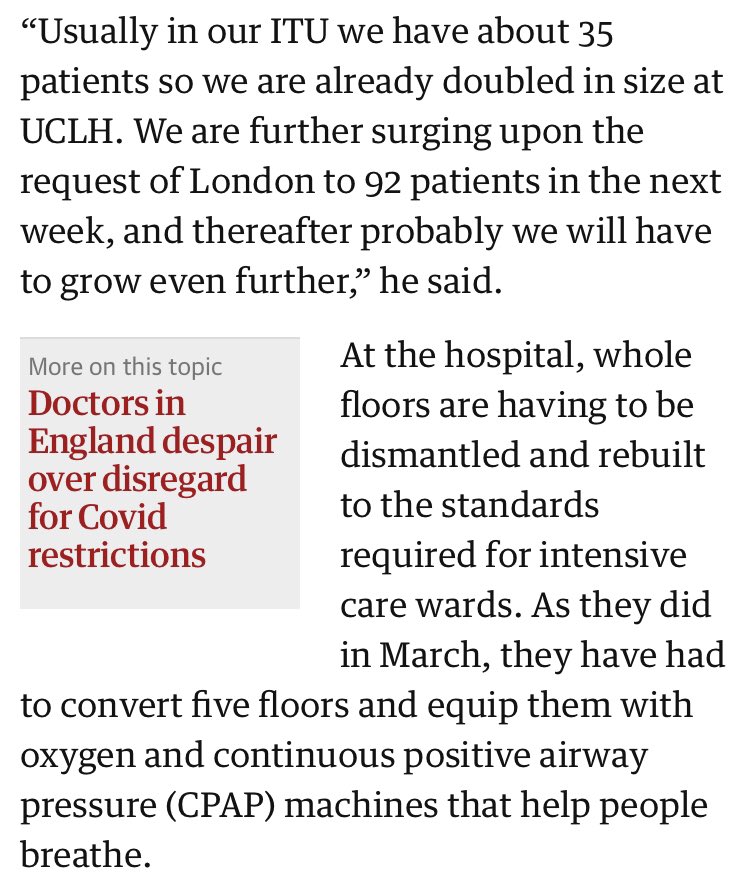
so how does an NHS intensive care unit cope when a spike of number of COVID patients suddenly hits?
well, more beds are created by finding ventilators in operating theatres and spreading staff thinner, huge efforts are made!
https://www.theguardian.com/world/2020/dec/31/london-hospital-uclh-warns-on-track-become-covid-only
well, more beds are created by finding ventilators in operating theatres and spreading staff thinner, huge efforts are made!
https://www.theguardian.com/world/2020/dec/31/london-hospital-uclh-warns-on-track-become-covid-only
but the awful reality is that there’s only so many extra beds and staff that can be found, so doctors have warned that care may have to be rationed
of course this is politically hugely controversial https://www.theguardian.com/world/2020/dec/29/nhs-could-face-horrendous-choices-over-who-gets-coronavirus-care
of course this is politically hugely controversial https://www.theguardian.com/world/2020/dec/29/nhs-could-face-horrendous-choices-over-who-gets-coronavirus-care
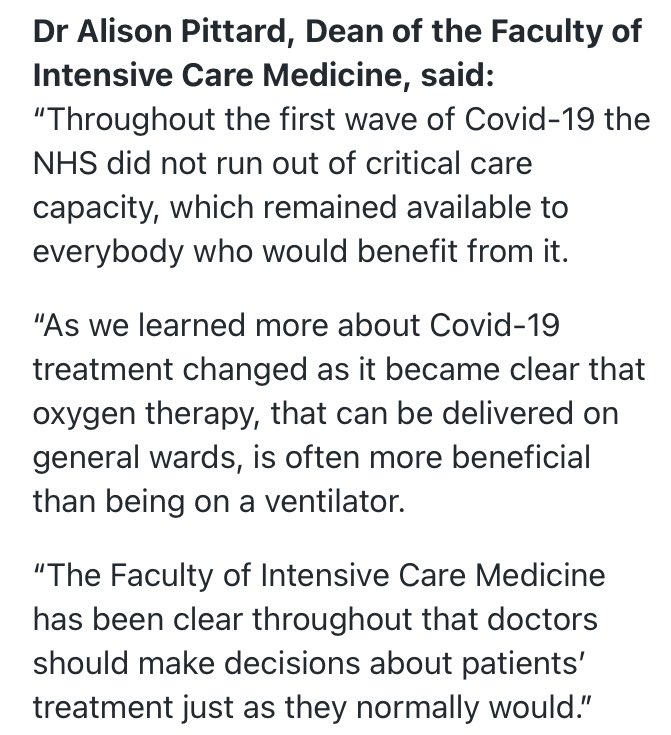
in October, the Sunday Times reported that the “elderly paid the price” for protecting the NHS from the first wave of the virus
the claim was that the elderly ended up with a reduced level of care to allow young coronavirus victims to be treated https://www.thetimes.co.uk/article/revealed-how-elderly-paid-price-of-protecting-nhs-from-covid-19-7n62kkbtb
the claim was that the elderly ended up with a reduced level of care to allow young coronavirus victims to be treated https://www.thetimes.co.uk/article/revealed-how-elderly-paid-price-of-protecting-nhs-from-covid-19-7n62kkbtb
NHS England and multiple professional medical organisations strongly disputed this claim that doctors and NHS trusts changed their behaviour to discriminate against the elderly
https://www.england.nhs.uk/2020/10/nhs-and-other-professional-bodies-response-to-sunday-times/
https://www.england.nhs.uk/2020/10/nhs-and-other-professional-bodies-response-to-sunday-times/
as NHS pressure ramps up during this new wave, it’s worth looking again at the official government statistics to see how many older coronavirus victims are getting HDU and intensive care level treatment
this time around there’s a very valuable previous comparison period, ie when NHS hospitals were under little stress in early Autumn
plus doctors have been treating COVID for months by now, so it’s harder to say that there was a big shift in clinical understanding of the disease
plus doctors have been treating COVID for months by now, so it’s harder to say that there was a big shift in clinical understanding of the disease
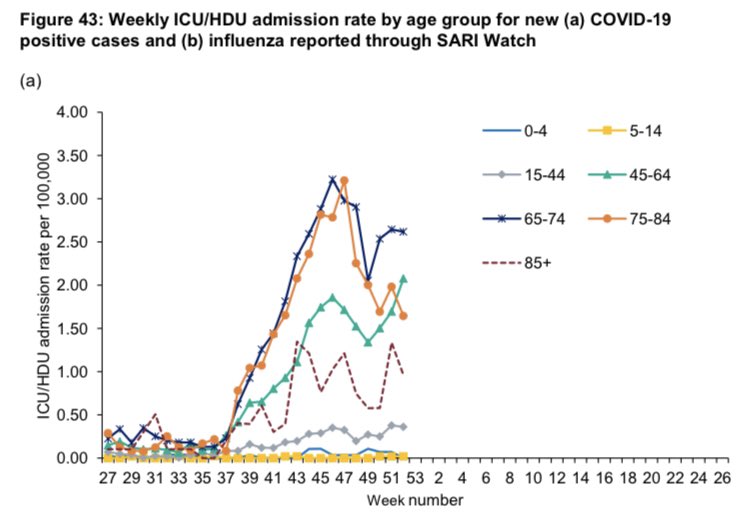
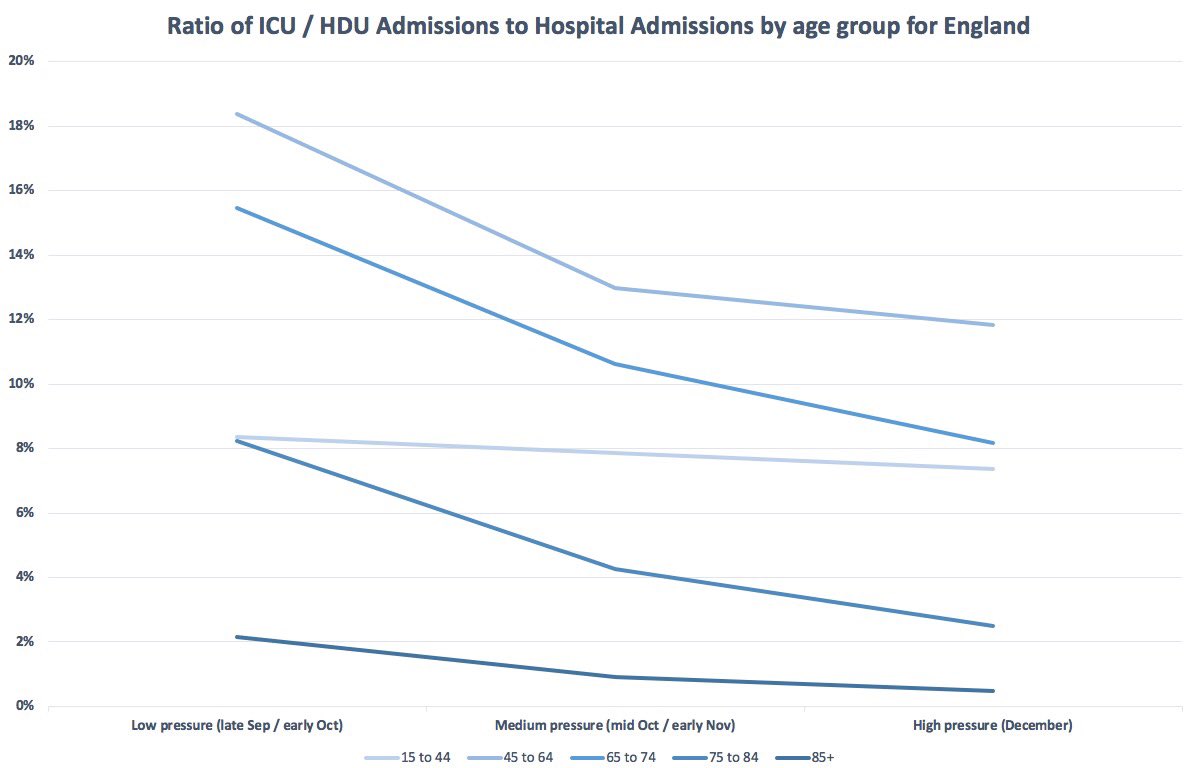
this is a chart of the raw data on ICU admission rates per capita for England, split into age bands
there’s already changes in the ICU/HDU admission rates for older people between November and December that can be “eyeballed” here (report p52)
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/948638/Weekly_Flu_and_COVID-19_report_w53.pdf
there’s already changes in the ICU/HDU admission rates for older people between November and December that can be “eyeballed” here (report p52)
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/948638/Weekly_Flu_and_COVID-19_report_w53.pdf
now to make a fair comparison you need to standardise for admission rates - after all if less older people are getting coronavirus and ending up in hospital, it wouldn’t be so surprising that less are in ICU/HDU
however this doesn’t seem to be the case
however this doesn’t seem to be the case
to make a simple comparison, I’ve split the national data into three 4 week periods
“Low pressure” which is weeks 38 to 41: mid September to early October
“Medium pressure” which is weeks 42 to 45: mid October to early November
“High pressure” which is weeks 49 to 52: December
“Low pressure” which is weeks 38 to 41: mid September to early October
“Medium pressure” which is weeks 42 to 45: mid October to early November
“High pressure” which is weeks 49 to 52: December
I’ve then calculated a simple ratio of the number of patients admitted to ICU/HDU, divided by the number of patients admitted to hospital for these 4 week periods
for short, I’ll call this the ICU admissions ratio
for short, I’ll call this the ICU admissions ratio
on a chart, the ICU admissions ratio looks like this
seems everyone in hospital is less likely to get an ICU or HDU bed as NHS pressure increases, but the drops are much bigger for older age groups compared to the young
seems everyone in hospital is less likely to get an ICU or HDU bed as NHS pressure increases, but the drops are much bigger for older age groups compared to the young
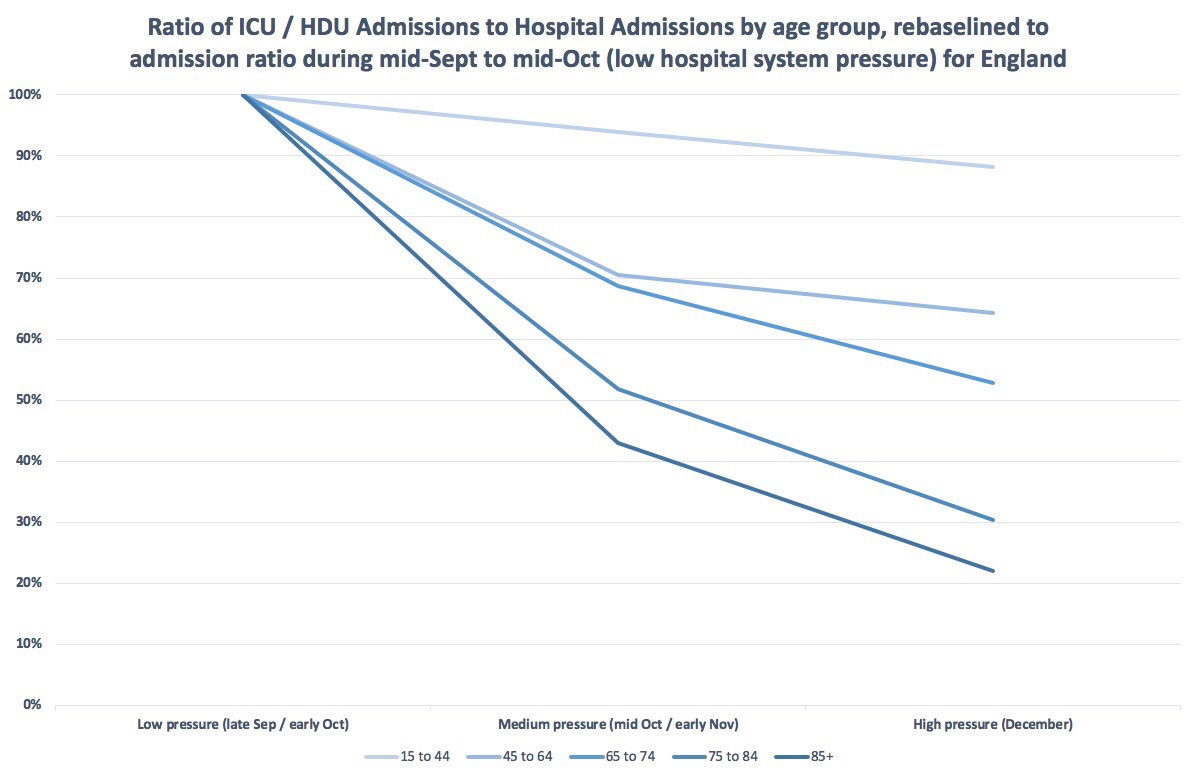
to make these changes easier to visualise, let’s assume the ICU admission ratios back in early Autumn (labelled as low pressure) was the NHS operating “normally”
if we rebaseline the “medium” and “high pressure” data relative to “normal” (“low pressure”), the changes look stark
if we rebaseline the “medium” and “high pressure” data relative to “normal” (“low pressure”), the changes look stark
bear in mind I have averaged the data for the whole country and all of December into the “High pressure” ratios here
there are good reasons to think that this situation is deteriorating and that, if this data was available split out by region, London and Kent would be even worse
there are good reasons to think that this situation is deteriorating and that, if this data was available split out by region, London and Kent would be even worse
this is a simple analysis of publicly available data, I’m not an expert in intensive care or medical statistics
all I’m saying is there were proportionally *a lot more* older COVID patients in ICU/HDU in early Autumn, than there were last month
for over 75s, 3 to 4 times more
all I’m saying is there were proportionally *a lot more* older COVID patients in ICU/HDU in early Autumn, than there were last month
for over 75s, 3 to 4 times more
there may be a good reason for this large change in age demographic in intensive care, that isn’t that the NHS is rationing care to elderly COVID patients
but as a non-expert, I’m struggling to see what the ‘non-rationing’ explanation could be to explain a change that size
but as a non-expert, I’m struggling to see what the ‘non-rationing’ explanation could be to explain a change that size
so where are the ‘missing’ elderly ICU patients, compared to early Autumn, if NHS intensive care still officially has spare capacity?
if we’re told the NHS is not rationing medical care, I think ministers *and* medical leaders need to give an explanation for what’s going on here
if we’re told the NHS is not rationing medical care, I think ministers *and* medical leaders need to give an explanation for what’s going on here
here’s the data I’ve extracted and processed from the publicly available PHE report, for other people to review and make use of
none of this is complex analysis and there seems to be a lot of ‘missing patients’ that need finding … http://ge.tt/6jeP16A3
none of this is complex analysis and there seems to be a lot of ‘missing patients’ that need finding … http://ge.tt/6jeP16A3

 Read on Twitter
Read on Twitter