I'll be tweeting here. Dr. Jean Hausheer, the coalition's lead on COVID-19 is starting. She takes a moment to reflect on the 2,300 Oklahomans who have died from the coronavirus and notes that Oklahoma again set a record for hospitalizations last night. https://twitter.com/CathJSweeney/status/1343979156711878659
Dr. David Kendrick, CEO of MyHealth Access and professor of medical informatics at the OU College of Community Medicine: We're showing a 7-day positivity rate of about 26 percent. (OK was recently ranked 1st in the nation for its positivity rate.)
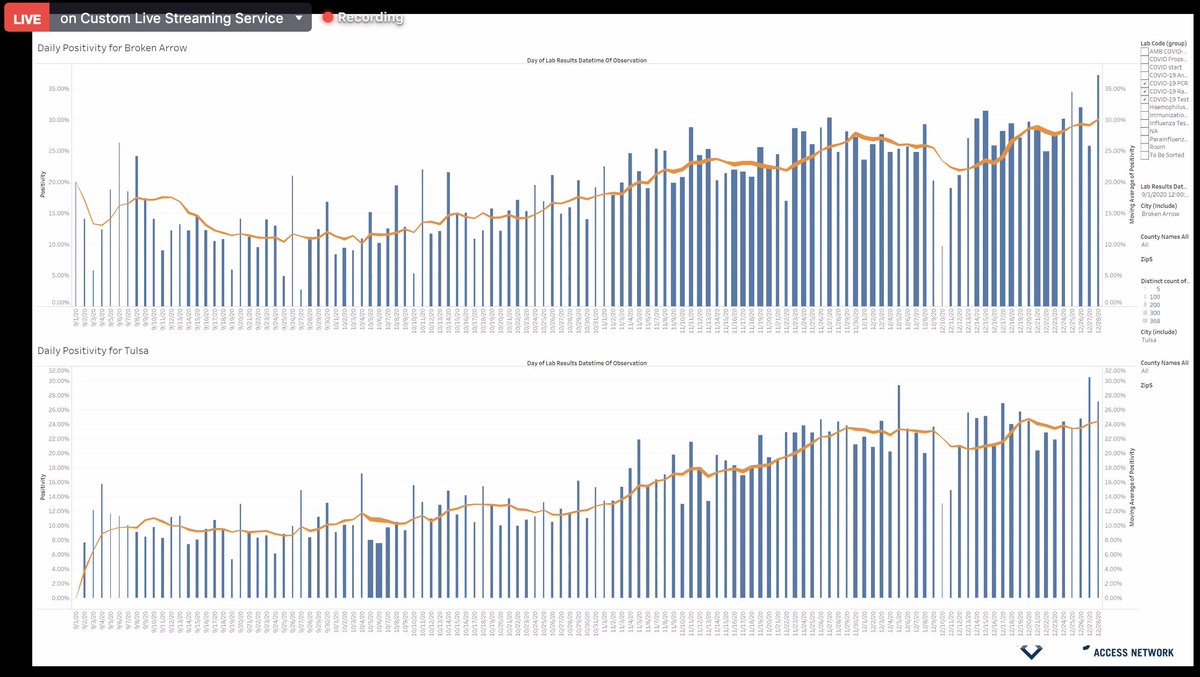
Kendrick: I've been asked about positivity in specific masked vs. non-masked cities. Tulsa has a mandate, Broken Arrow famously doesn't. Tulsa's 7-day positivity rate average is about 24 percent. Broken Arrow's is about 30 percent.
Kendrick: In our ICUs, we are tracking how many patients are from mask mandates cities are not. We're seeing a 60-40 split, with the majority coming from non-mandate cities.
George Diaz, M.D., infection prevention manager at Providence Regional Medical Center, in Everett, WA, and physician who treated first confirmed COVID-19 case in the U.S. is going to talk about the new COVID-19 strains.
Diaz: The UK does a good job of sequencing COVID viruses. What they found is the new strain has mutations in the spike protein, which is the mechanism the virus uses to enter human cells. The mutations make entering cells easier, which makes the virus more contagious.
Diaz: The new strain is not necessarily more deadly, but it is more contagious, especially among children. This is likely spread worldwide already because of travel.
Diaz: Despite the mutations in the spike protein, we are of the belief the mRNA vaccine will still protect against the new strain. "Our hope is, at this point, that people will still get vaccinated."
Rear Admiral Travis Watts, Pharm.D, director of Oklahoma City Area Indian Health Services and assistant surgeon general: The Oklahoma City-area IHS has received over 8,700 doses of Pfizer and 8,900 of Moderna. We're expecting thousands more in coming weeks.
Watts: IHS is using hub sites to distribute their vaccines (this is similar to how Oklahoma is distributing its vaccines). In recent weeks, our focus has been on frontline health workers. We're now moving on to elders and those with comorbidities, as well as essential workers.
Watts: It's important that, as a health system, we continue talking about containing the virus. While we're moving the vaccine through, we need to continue an education complain about the 3 Ws (wash your hands, wear a mask, watch your distance).
Dale Bratzler, D.O., chief COVID officer with the University of Oklahoma: I usually describe what we're doing in three different phases. Back in June, most of our efforts were focused on making the environment (classroom, labs) safer. HVAC systems, air filters, de-densifying.
Bratzler: We implemented masking policies, which students and staff were great at complying with. With the start of the fall semester, our focus shifted to early detection.
Bratzler: "You cannot screen out COVID-19." Among young people, half of the people who get the infection have no symptoms. Checking temperatures won't work. We needed surveillance testing, we did wastewater testing, etc. Going forward, we expect after the holidays cases to surge.
Bratzler: We expect the case counts presented by the State Department of Health to be lower than reality. Not enough people are getting tested.
Bratzler: "I think all of us are concerned" about the amount of travel that took place over the holidays and the spread that will bring.
George Monks, M.D., president of the Oklahoma State Medical Association: "We had a hard night last night in the hospitals." We again set a record.
Monks: I'm going to talk about the economic impact. We have seen that places with strong mitigation efforts rebounded quickly. "Workers in those areas were able to return to work safely." They had fewer cases and fewer deaths. Cites figures from Germany, New Zealand and Australia
Monks: "We know unemployment remains high, but with all the negatives, we have hope because the vaccine is here."
@ChaseHorn: We have just over 30,000 vaccinations so far. It looks like the state has about 100,000 vaccines on hand. Why does it take so long to distribute them?
Bratzler: Our system alone gave 5,000 doses out yesterday. There is a reporting delay. The dashboard is lagged.
Bratzler: Our system alone gave 5,000 doses out yesterday. There is a reporting delay. The dashboard is lagged.
Bratzler: It's a slower vaccine. We have to watch everyone for 15 minutes after the vaccine, and for 30 minutes if they have a history of reactions.
Kendrick: These vials have an inexact amount of doses. They have to be thawed, which can affect number of doses too.
Kendrick: These vials have an inexact amount of doses. They have to be thawed, which can affect number of doses too.
Diaz: We've been vaccinating people as well here in Washington state. Physicians are much more likely to accept the vaccine, whereas nursing staff is less likely. Health care workers are members of the general public and therefore still subject to misinformation.
Diaz: You can have all the vaccine in the world, but you have to have people who are willing to take them.
@ReporterJanelle What are we seeing in terms of uptake, the desire to take the vaccine? What do we foresee in future populations?
Diaz: We have seen variation among populations, even just in roles. Doctors, we're seeing about 90% taking them. Among nursing staff, 40%
Diaz: We have seen variation among populations, even just in roles. Doctors, we're seeing about 90% taking them. Among nursing staff, 40%
Bratzler: Our real push is going to start next week, after the holidays. We're still learning how to do this, and the best ways to educate people. Remember, these side effects are incredibly transient. They last a day or two.
Diaz: There have been concerns about anaphylactic response. In the people that have a history anaphylaxis, we haven't seen much. That concern is overhyped.
@KOCODillon Oklahoma County is at about 39 percent of hospital occupancy being filled with covid patients, nearing Tier 4 of the covid hospitalization plan.
Hausheer: It's a moving target because figures change every hour.
Kendrick: They're doing what they can. Converting units.
Hausheer: It's a moving target because figures change every hour.
Kendrick: They're doing what they can. Converting units.
Bratzler: Oklahoma City metro hospitals have expanded their covid capacity by about 30 percent in a month, through converting spaces etc. But it's still bad. "We're stretched. We have more covid patients in the hospital today than we've ever had."
Corey Jones, Tulsa World: Given the new variance in strains, are we still expecting to be able to get rid of this or not?
Diaz: "If we were able to make vaccines mandatory, we'd get this behind us right away." Even with the new strains, it should still be effective.
Diaz: "If we were able to make vaccines mandatory, we'd get this behind us right away." Even with the new strains, it should still be effective.
@TevisHillisTV Is the state's 11 p.m. curfew on bar and restaurant indoor services effective?
Hausheer: "I would say absolutely."
Bratzler: "This virus is transmitted in restaurants and bars. We know that." 11 p.m. is arbitrary. Capacity limits would be better.
Hausheer: "I would say absolutely."
Bratzler: "This virus is transmitted in restaurants and bars. We know that." 11 p.m. is arbitrary. Capacity limits would be better.
Diaz: A Stanford study shows that transmission is rapid in bars and restaurants. It's going to be bad anywhere you take your mask off. Washington state has banned indoor dining.
@JeffMorganTV: What is the effect of testing being low? And what role do lab test cost increases play?
Bratzler: What the testing and positivity rate figures are showing us is people are no longer getting tested regularly but only when they are sick.
Bratzler: What the testing and positivity rate figures are showing us is people are no longer getting tested regularly but only when they are sick.
Diaz: We're a year into the pandemic, but we are still having supply chain issues. That is playing a role as well.
Hausheer on anaphylaxis: We tell people with a history of it to bring their epinephrine auto injector (aka EpiPen) in case they do have a reaction. "They know to bring their EpiPen, and they've been fine." Diaz reiterated that his hospital has seen no issues with that.
Bratzler on post-holiday cases: We are all of the same belief. "In 10 days to 14 days, we're going to see a substantial surge." And remember, at least 10 percent of them will end up in the hospital. This is going to be a significant strain.
That's a wrap.

 Read on Twitter
Read on Twitter