#LongCOVID is real and bad.
Here is one of the most extensive and comprehensive long term follow-up of COVID patients (3762 respondents) with long lasting symptoms/complaints.
https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v2 via @ahandvanish @GinaAssaf et al.

A thread on LONG COVID.
1/n
Here is one of the most extensive and comprehensive long term follow-up of COVID patients (3762 respondents) with long lasting symptoms/complaints.
https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v2 via @ahandvanish @GinaAssaf et al.


A thread on LONG COVID.
1/n
Points covered:
 What is Long COVID?
What is Long COVID?
 Who can get Long COVID?
Who can get Long COVID?
 Why does Long COVID occur?
Why does Long COVID occur?
 Symptoms of Long COVID
Symptoms of Long COVID
 Some literature on Long COVID
Some literature on Long COVID
 Concerns about Long COVID
Concerns about Long COVID
 Instructions for the Common Man
Instructions for the Common Man
2/n
 What is Long COVID?
What is Long COVID? Who can get Long COVID?
Who can get Long COVID? Why does Long COVID occur?
Why does Long COVID occur? Symptoms of Long COVID
Symptoms of Long COVID Some literature on Long COVID
Some literature on Long COVID Concerns about Long COVID
Concerns about Long COVID Instructions for the Common Man
Instructions for the Common Man2/n
 What is Long COVID?
What is Long COVID?> A large number of COVID19 patients suffer from long lasting effects of the infection
> Characterized by a constellation of symptoms involving multiple systems in the body for >28 days
> Leading to increased morbidity even after "apparent recovery"
3/n
 Who can get Long COVID?
Who can get Long COVID?> Any patient who suffered from #COVID19 infection - mild, moderate or severe - can suffer from Long COVID.
> Even those with a mild infection can have symptoms lasting for more than 28 days and develop Long COVID.
4/n
 Why does Long COVID occur?
Why does Long COVID occur?> The pathophysiology behind Long COVID is yet unknown.
> Theories:
* ACE-2 receptor mediated multi-organ damage
* Viral persistence in body long after recovery
* Relapse or reinfection
* Immune mediated reactions
* Mental factors like PTSD
5/n
 Symptoms of #LongCovid
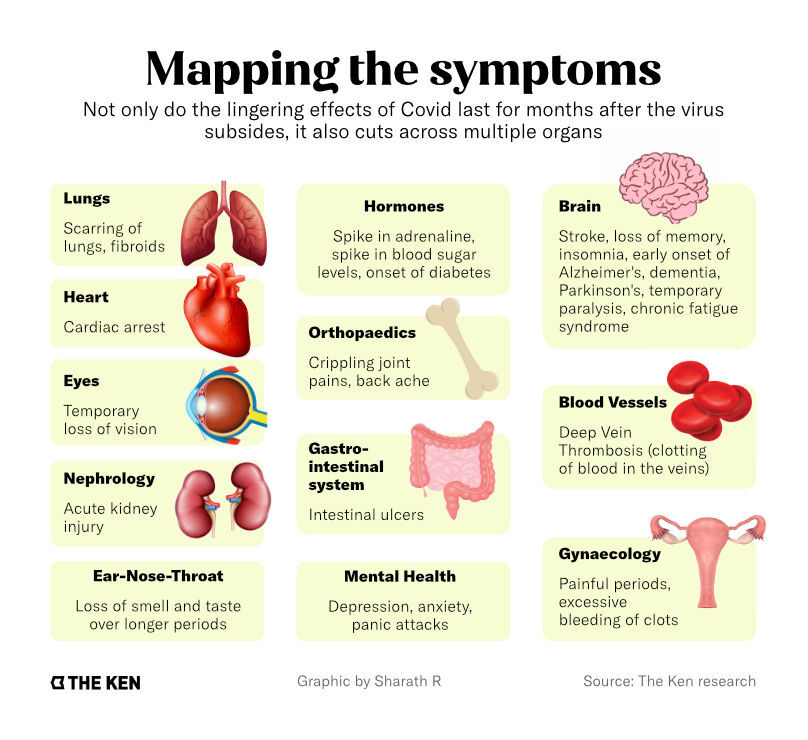
Symptoms of #LongCovid Here's a summary of the symptoms of Long COVID from @TheKenWeb.
A very helpful article on Long COVID from @TheKenWeb by @maitriporecha1.
https://the-ken.com/story/the-hidden-second-epidemic-of-long-covid/
We'll look at the symptoms in detail.
6/n
 Symptoms of #LongCovid
Symptoms of #LongCovid> @ahandvanish et al studied a total of 205 symptoms in their study.
>Non-Neuropsychiatric - Includes all symptoms of individual organ systems.
> Neuropsychiatric - Symptoms associated with neurological and cognitive functions.
7/n
 Non-Neuropsychiatric Symptoms:
Non-Neuropsychiatric Symptoms:> These symptoms are further divided according to the organ systems affected -
ENT
Gastrointestinal
Reproductive, Genitourinary and Endocrine
Cardiovascular
Musculoskeletal
Dermatological
Immunological/Auto-immune
Pulmonary
8/n
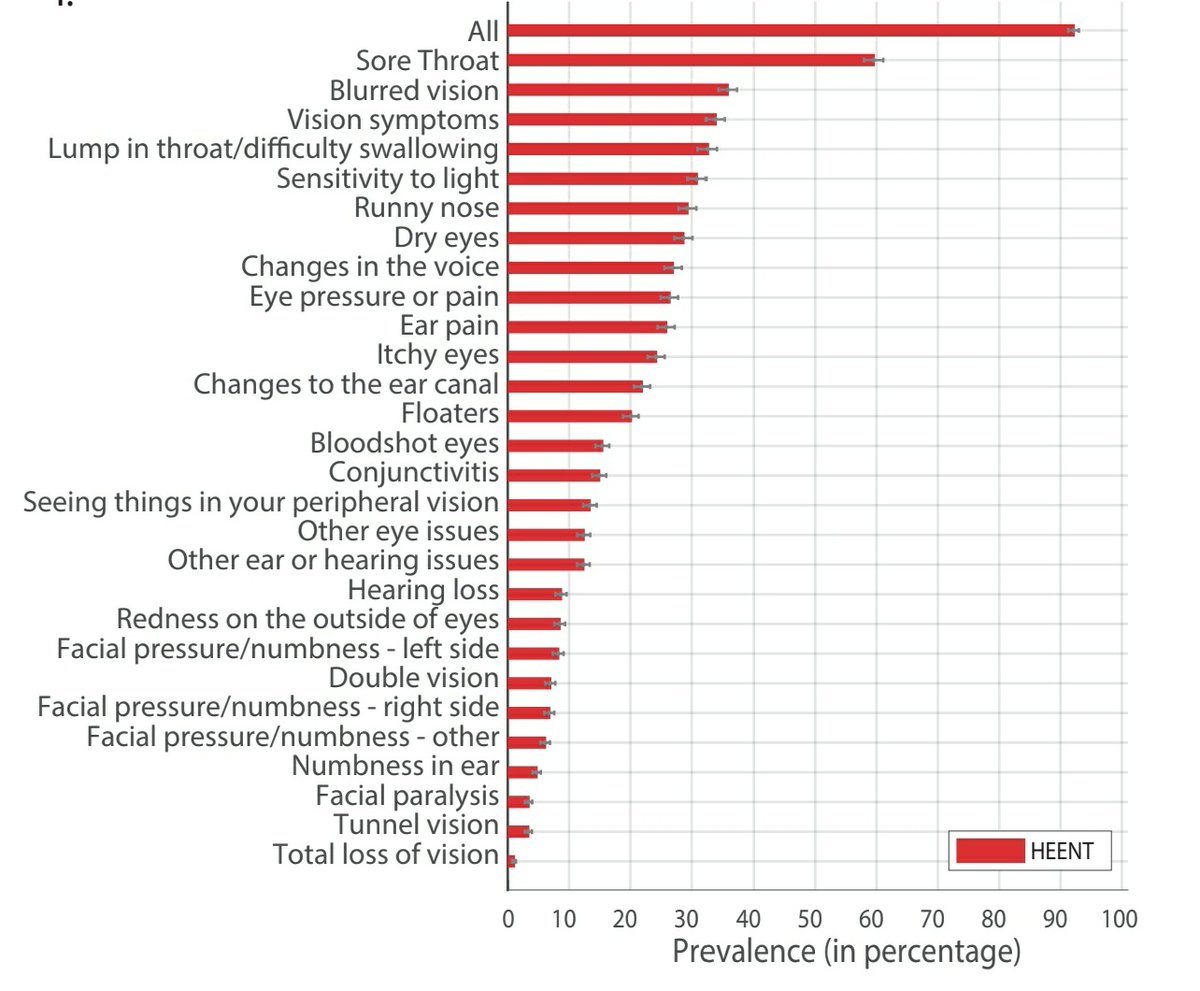
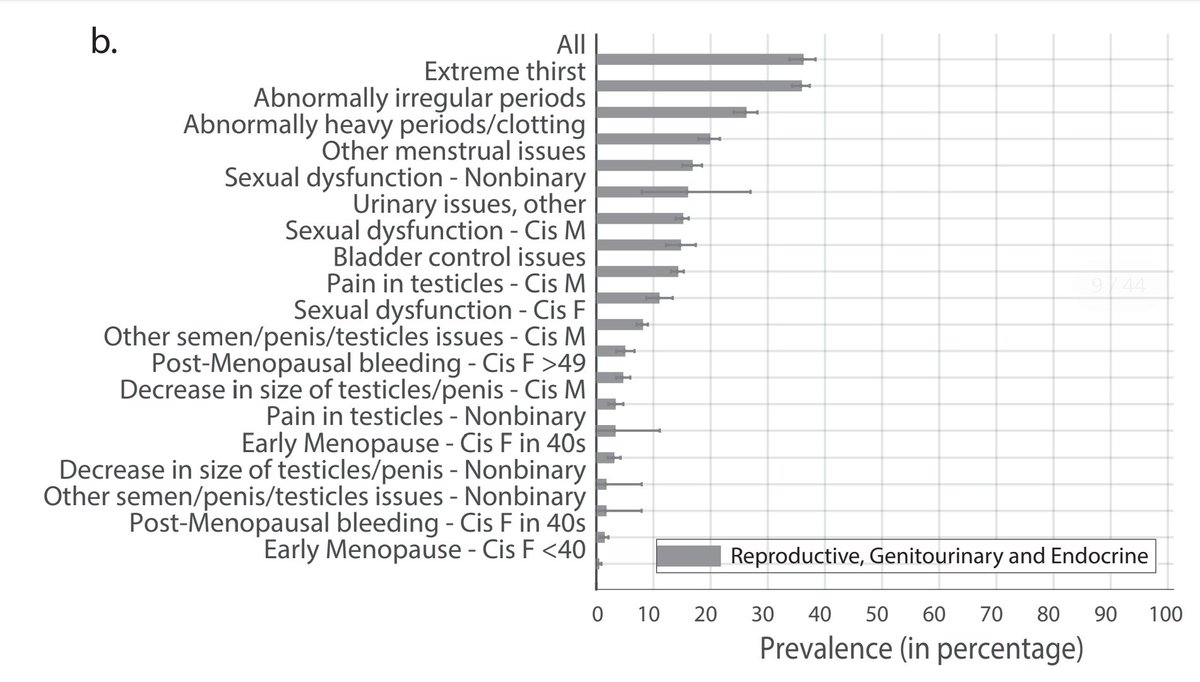
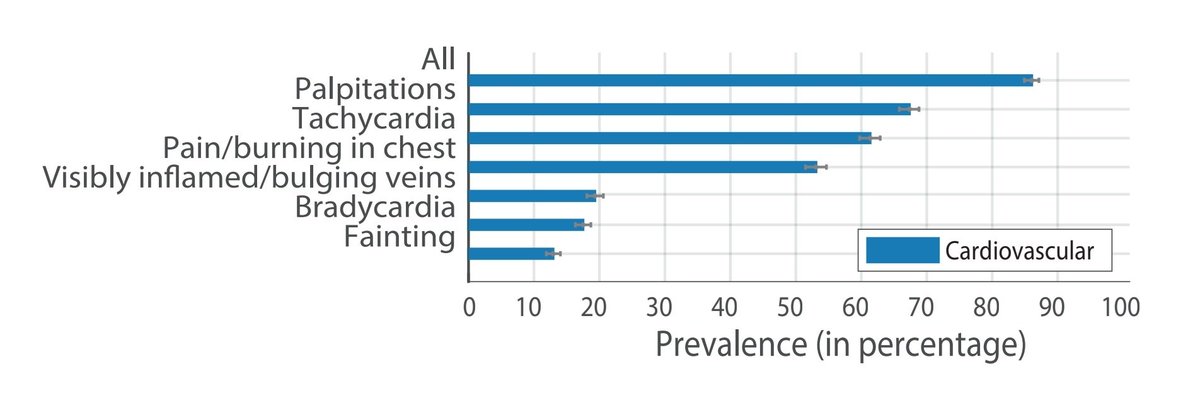
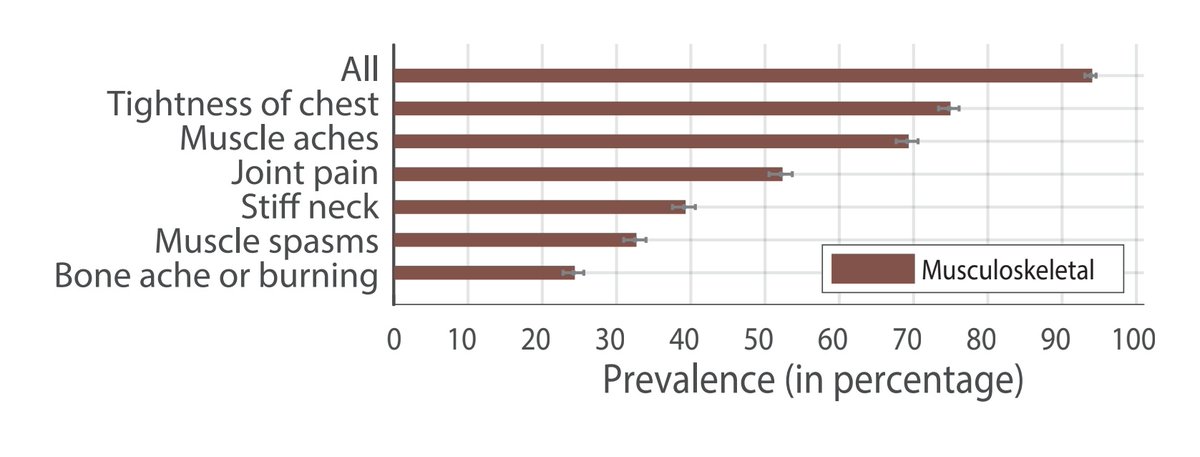
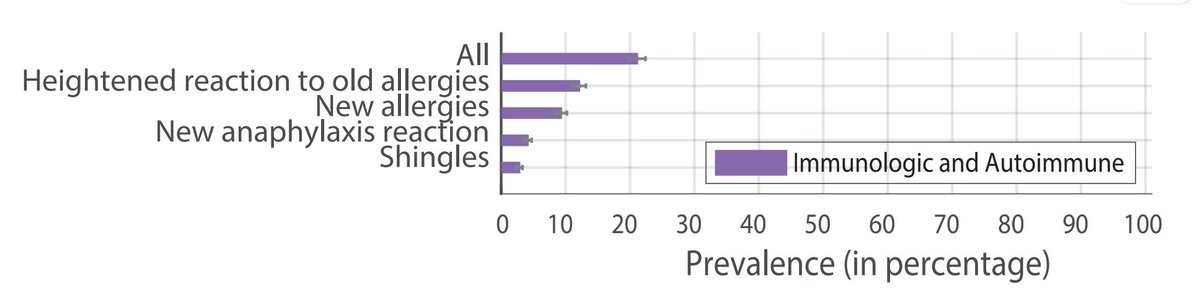
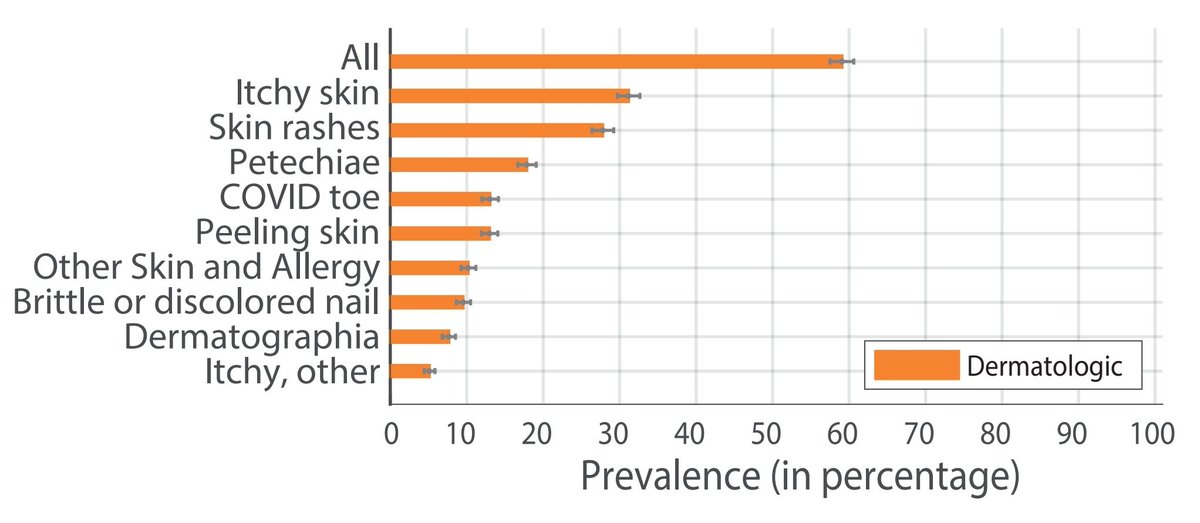
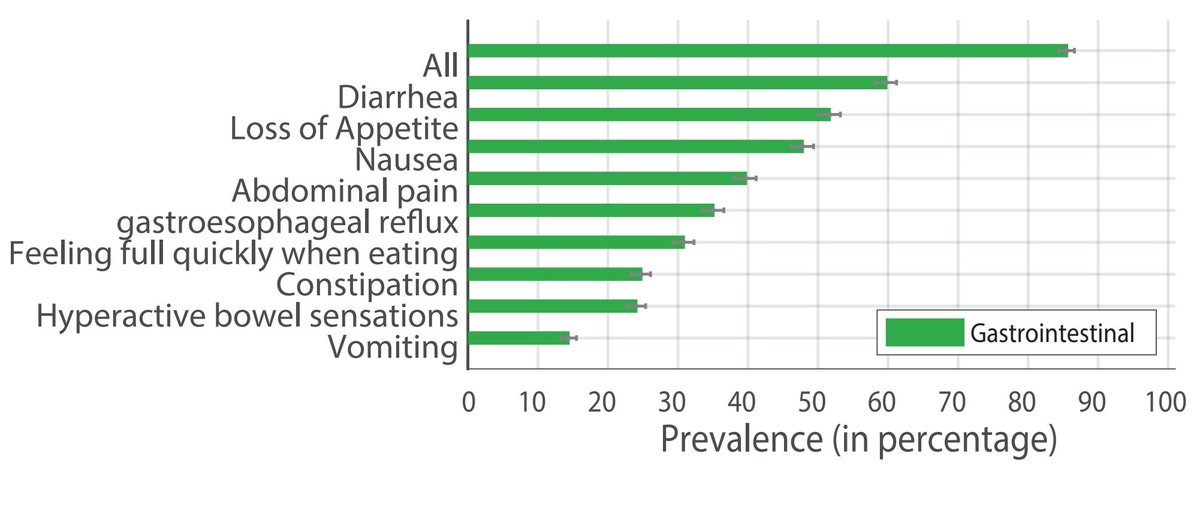
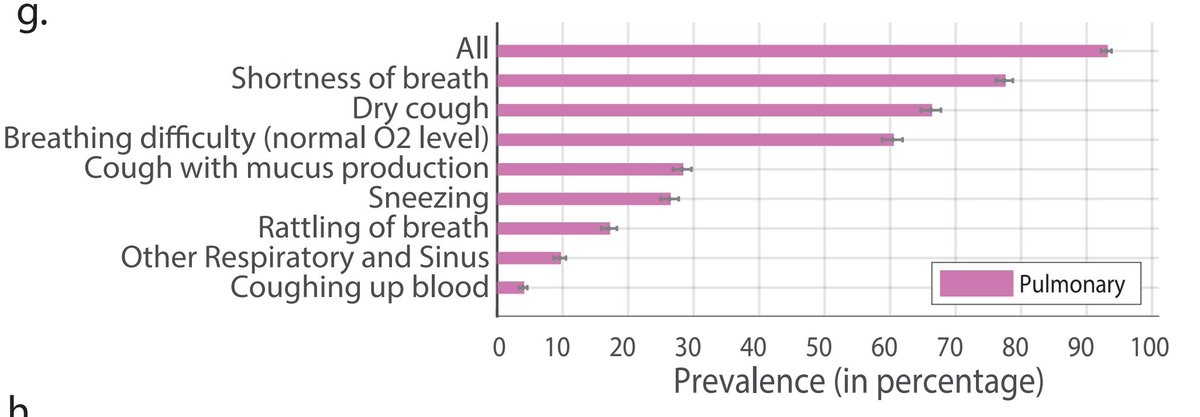
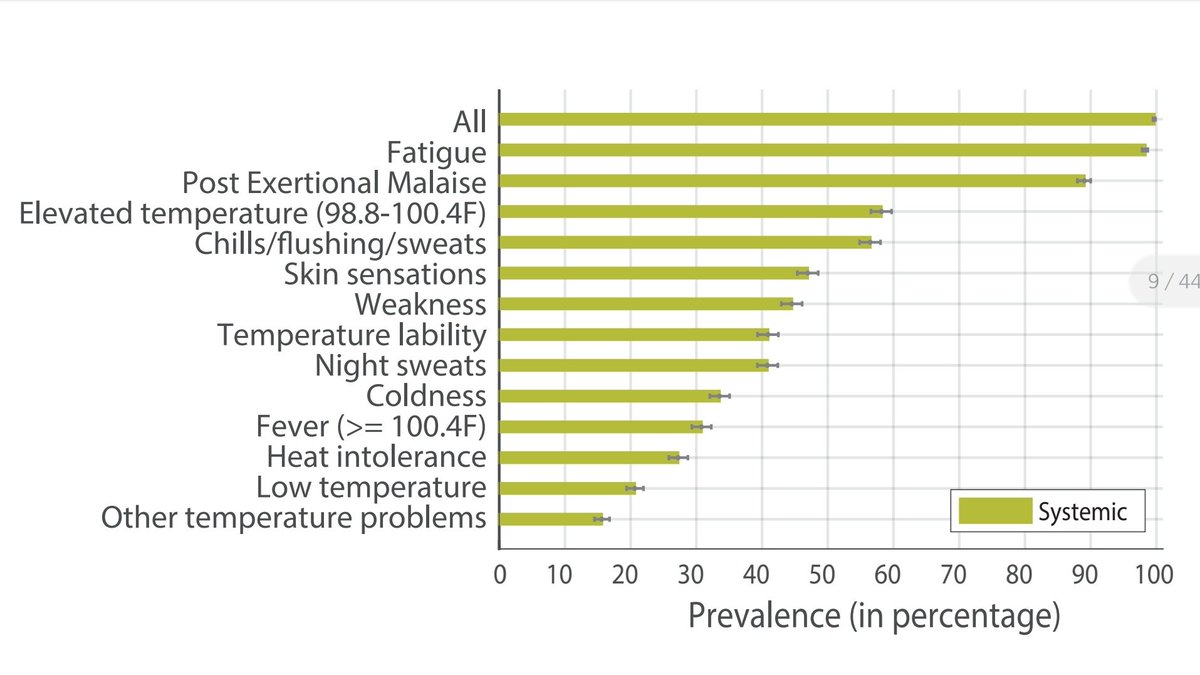
A look at the prevalence of Non Neuropsychiatric Symptoms:
The graphs show prevalence of individual symptoms in percentage.
1. HEENT
2. Reproductive, Genitourinary, Endocrine
3. Cardiovascular
4. Musculoskeletal
Source: https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v2
9/n
The graphs show prevalence of individual symptoms in percentage.
1. HEENT
2. Reproductive, Genitourinary, Endocrine
3. Cardiovascular
4. Musculoskeletal
Source: https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v2
9/n
5. Immunological and Autoimmune
6. Dermatological
7. Gastrointestinal
8. Pulmonary
Source: https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v2
10/n
6. Dermatological
7. Gastrointestinal
8. Pulmonary
Source: https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v2
10/n
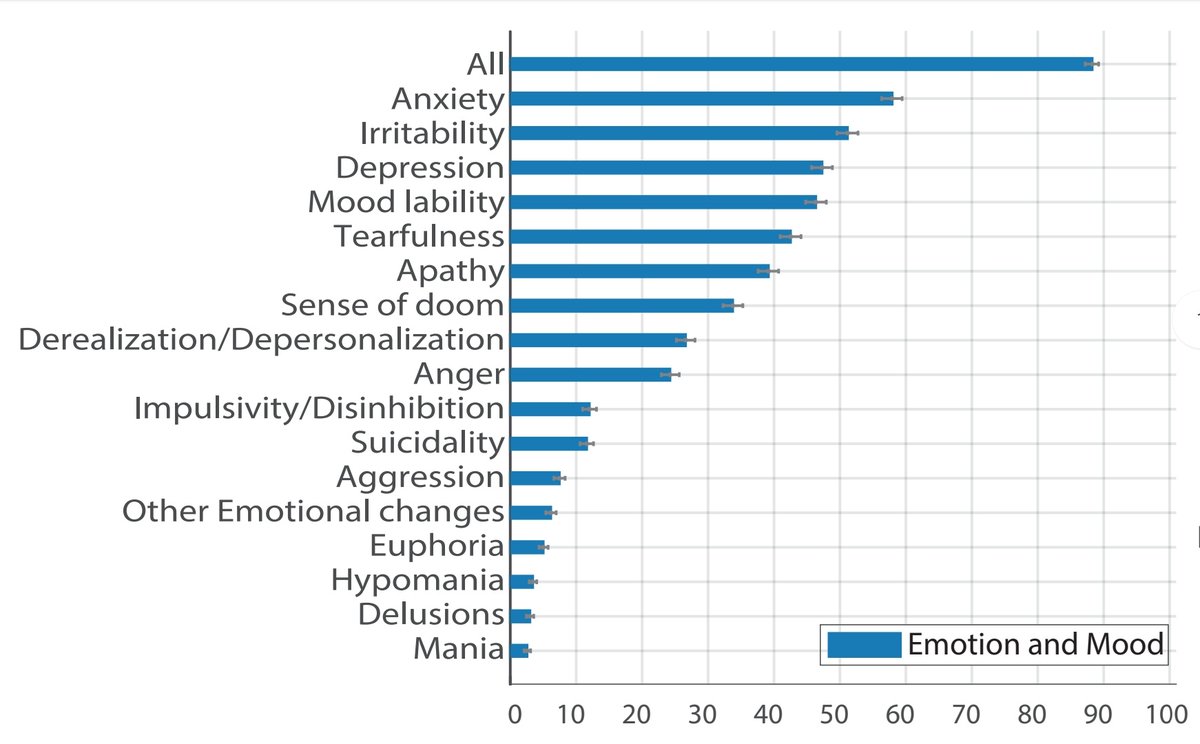
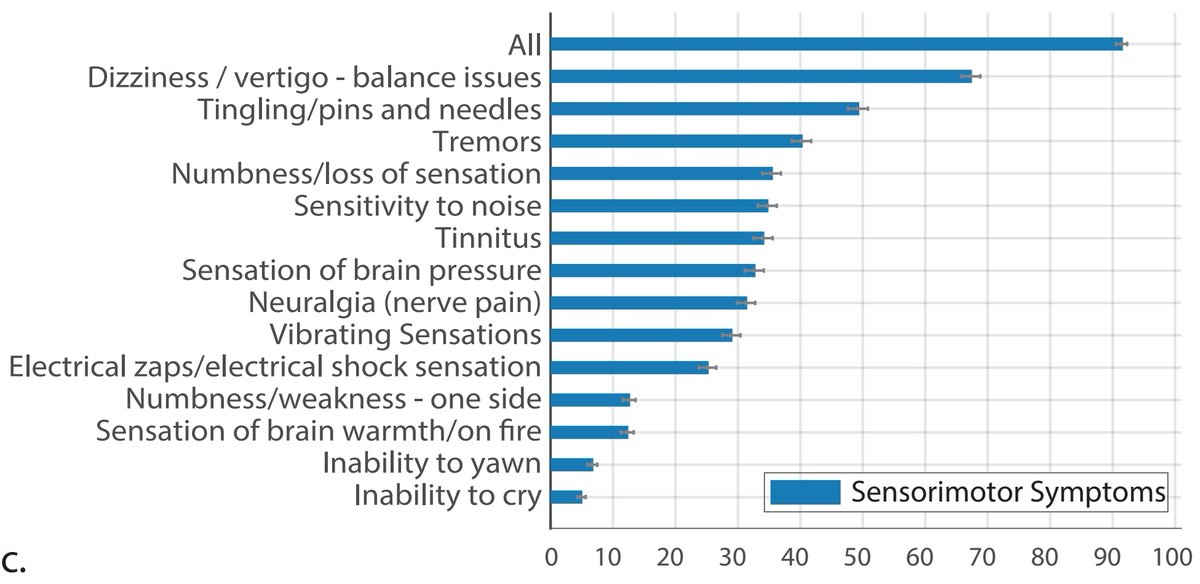
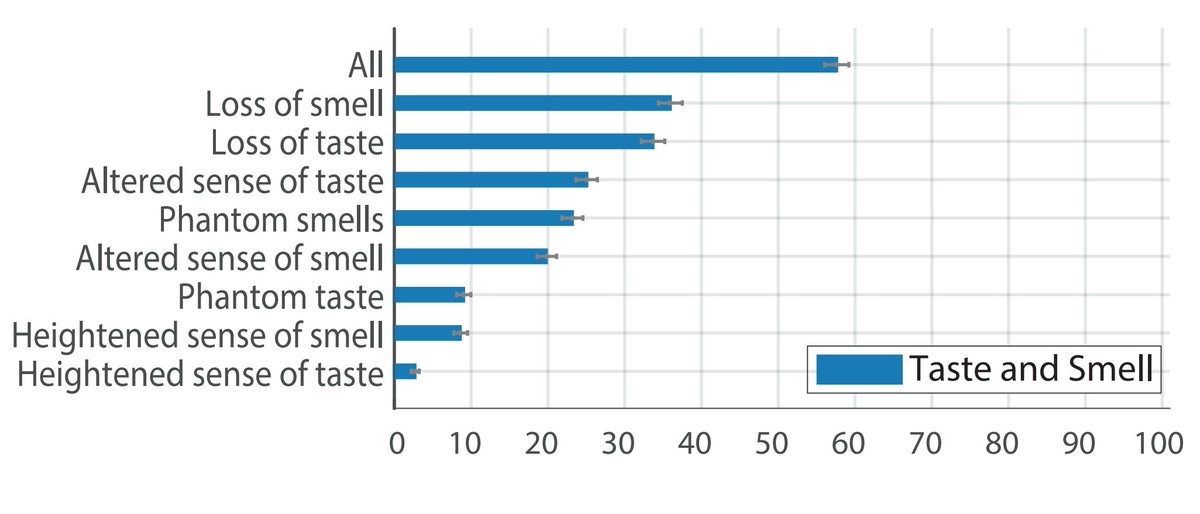
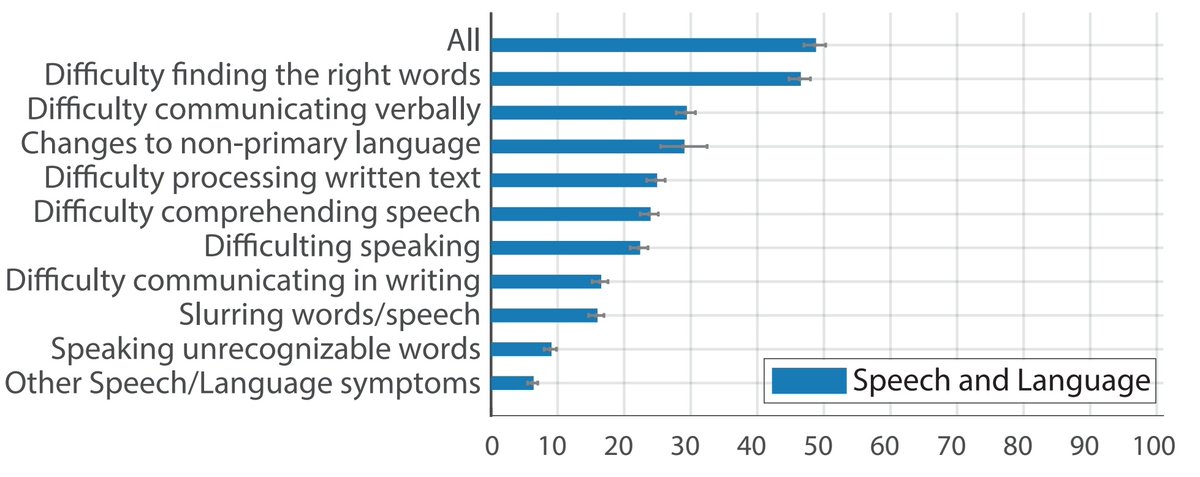
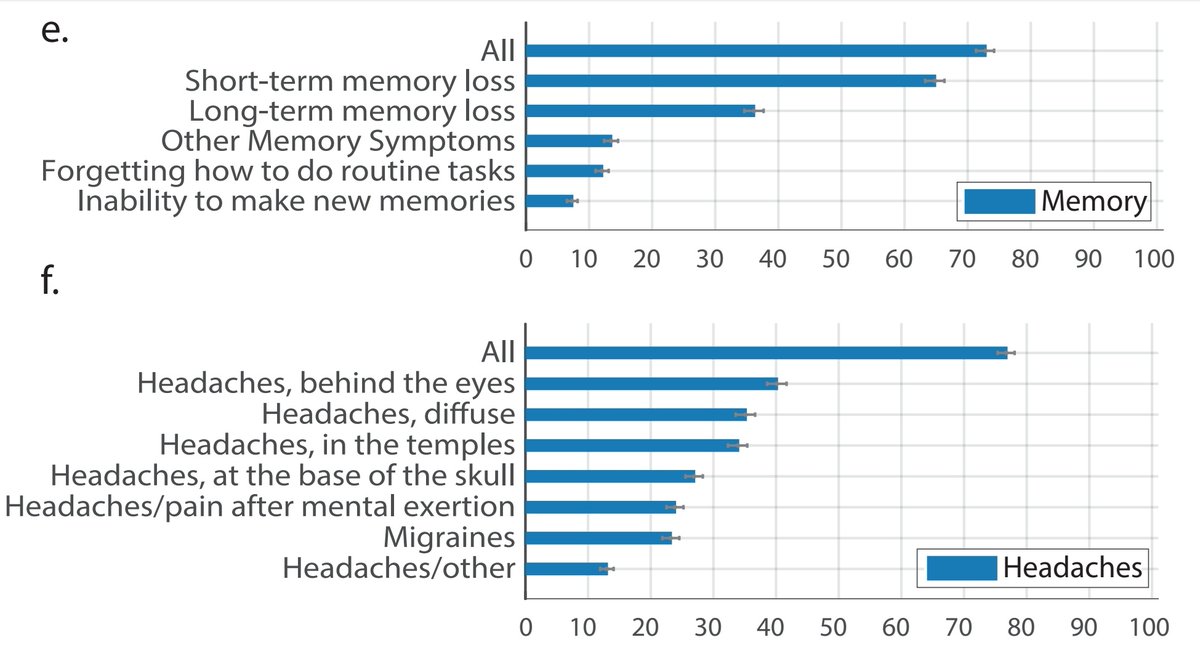
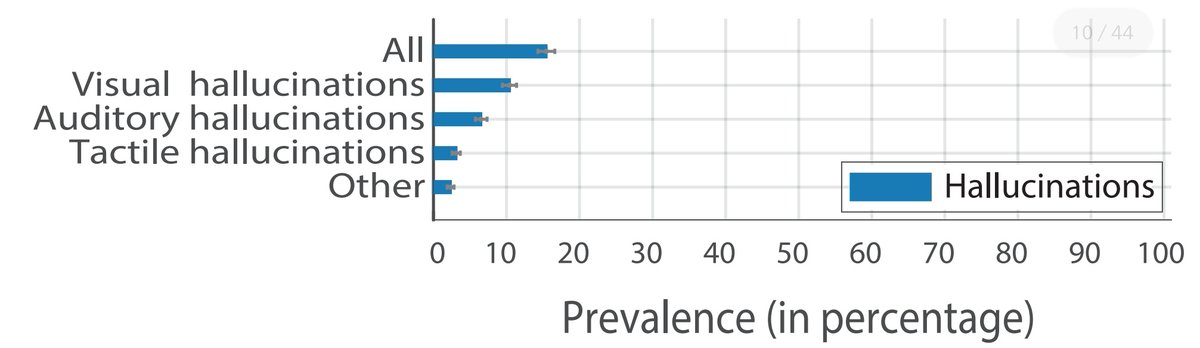
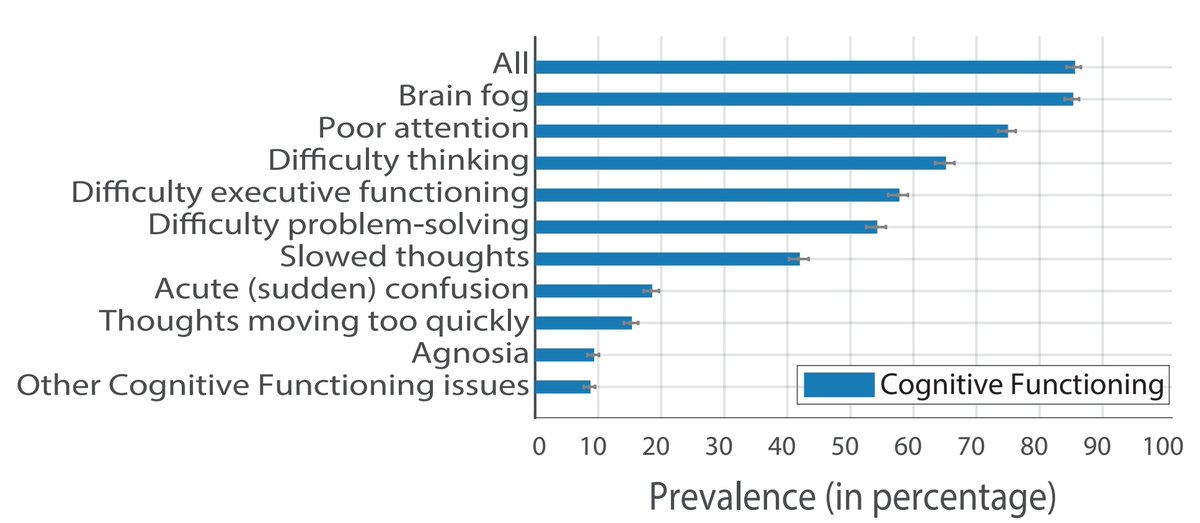
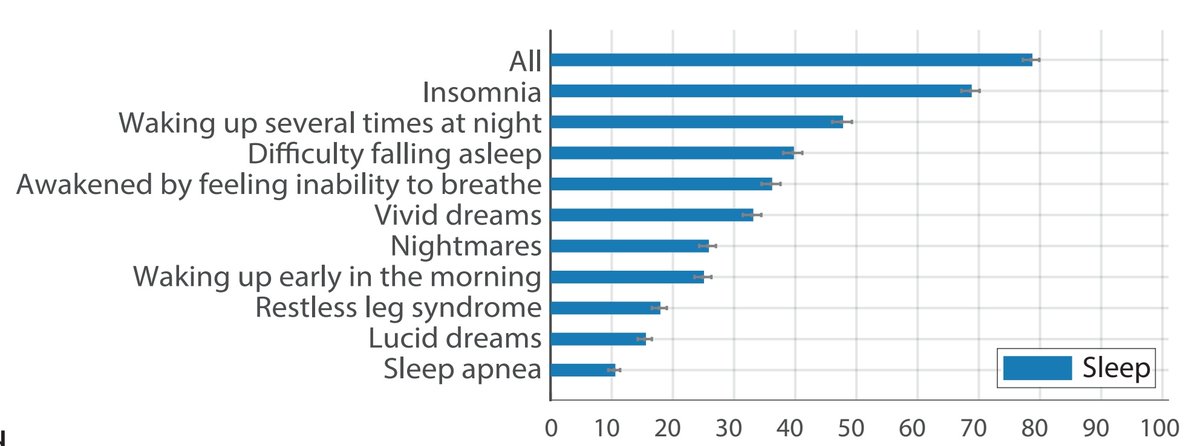
 Neuropsychiatric Symptoms:
Neuropsychiatric Symptoms:> These are further divided into sub-categories:
Emotion and Mood
Sleep
Memory
Headaches
Speech and Language
Hallucinations
Taste and Smell
Sensorimotor symptoms
Cognitive Functions
12/n
A look at the Neuropsychiatric Symptoms:
1. Emotion and Mood
2. Sensorimotor Symptoms
3. Taste and Smell
4. Speech and Language
Source: https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v2
13/n
1. Emotion and Mood
2. Sensorimotor Symptoms
3. Taste and Smell
4. Speech and Language
Source: https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v2
13/n
5. Memory and Headaches
6. Hallucinations
7. Cognitive Functions
8. Sleep
Source: https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v2
14/n
6. Hallucinations
7. Cognitive Functions
8. Sleep
Source: https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v2
14/n
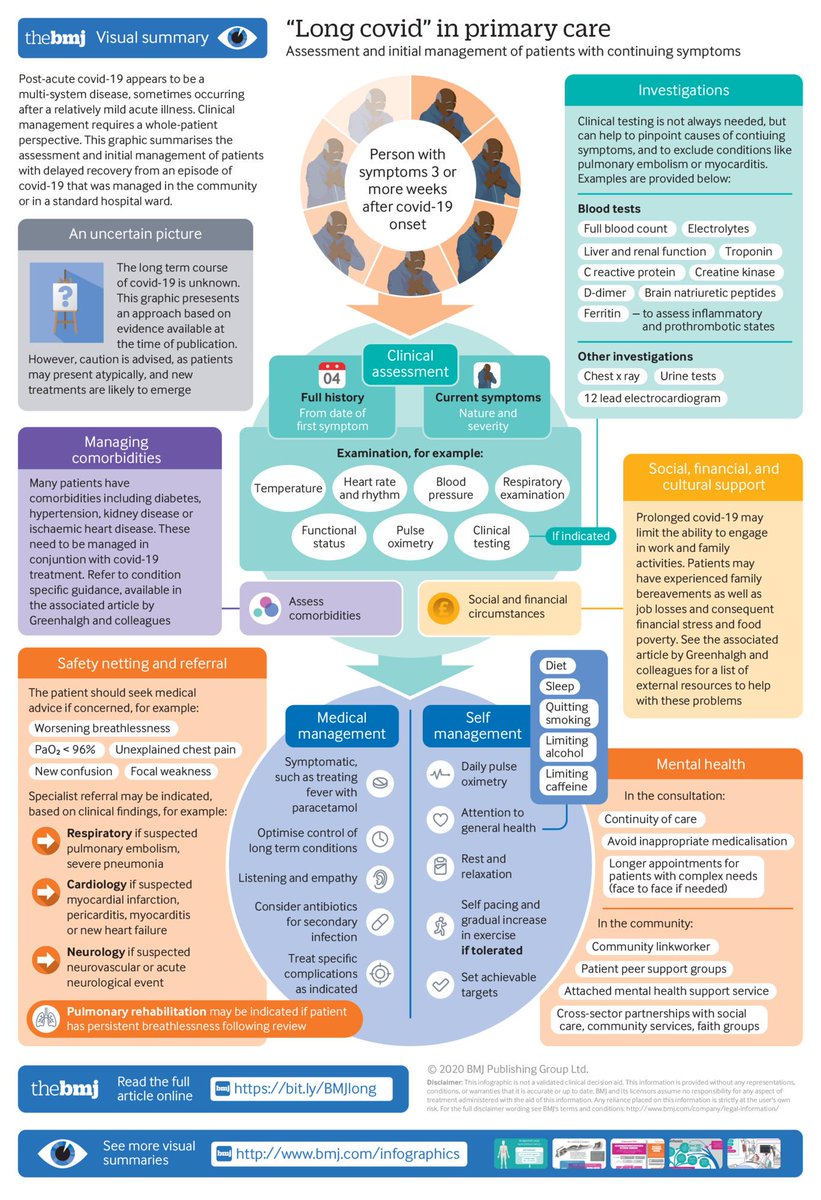
 Some Literature on Long COVID
Some Literature on Long COVIDHere is one excellent article on Long COVID and its management in @bmj_latest via @trishgreenhalgh et al.
https://www.bmj.com/content/370/bmj.m3026
15/n
A comprehensive infographic about Long COVID from the article by @trishgreenhalgh et al.
A basic, preliminary guide on how to approach suspected cases of Long COVID.
16/n
A basic, preliminary guide on how to approach suspected cases of Long COVID.
16/n
The National Institute for Health and Care Excellence @NICEComms has released a comprehensive set of guidelines on management of COVID and Post-COVID syndrome aka Long COVID.
https://www.nice.org.uk/guidance/ng188/chapter/Common-symptoms-of-ongoing-symptomatic-COVID-19-and-post-COVID-19-syndrome
17/n
https://www.nice.org.uk/guidance/ng188/chapter/Common-symptoms-of-ongoing-symptomatic-COVID-19-and-post-COVID-19-syndrome
17/n
 Concerns about Long COVID
Concerns about Long COVID> Mechanisms are not fully known. More studies are needed to establish pathophysiology of Long COVID.
> Duration is undetermined. We don't yet know if some of the organ damage is short-term, long-term or permanent.
18/n
> Increased post-infection morbidity and secondary mortality due to long term organ/systemic damage.
> Increased healthcare costs and burden.
> Aggravation of chronic disorders like Diabetes, Hypertension, COPD etc.
> Reduction in Quality of Life post-infection.
19/n
> Increased healthcare costs and burden.
> Aggravation of chronic disorders like Diabetes, Hypertension, COPD etc.
> Reduction in Quality of Life post-infection.
19/n
 Instructions for the Common Man
Instructions for the Common ManHere are some basic instructions to follow to manage Long COVID:
1. Prevent COVID infection:
>Masks and Distancing are mandatory.
> Vaccination when available.
20/n
2. Post-infection:
> Daily self-assessment of well-being.
> Rehabilitation to pre-infection status.
> Manage chronic diseases adequately.
> Note down:
* New symptoms
* Persistence and/or Aggravation of new/old symptoms.
> Consult a doctor asap for the above points.
21/21
> Daily self-assessment of well-being.
> Rehabilitation to pre-infection status.
> Manage chronic diseases adequately.
> Note down:
* New symptoms
* Persistence and/or Aggravation of new/old symptoms.
> Consult a doctor asap for the above points.
21/21

 Read on Twitter
Read on Twitter