And here is the preprint: "Characterizing Long COVID in an International Cohort: 7 Months of Symptoms and Their Impact"
Special thanks to thousands of you who participated in our study on #LongCovid.
a thread 0/ https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v1
0/ https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v1
Special thanks to thousands of you who participated in our study on #LongCovid.
a thread
 0/ https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v1
0/ https://www.medrxiv.org/content/10.1101/2020.12.24.20248802v1
>8k responded to our survey.
In this work, we focus on 3762 cases w illness lasting >28 days & onset prior to June 2020, which gives us the chance to characterize symptom profile & time course over 7 months, along w the impact on daily life, work & return to baseline health 1/
In this work, we focus on 3762 cases w illness lasting >28 days & onset prior to June 2020, which gives us the chance to characterize symptom profile & time course over 7 months, along w the impact on daily life, work & return to baseline health 1/
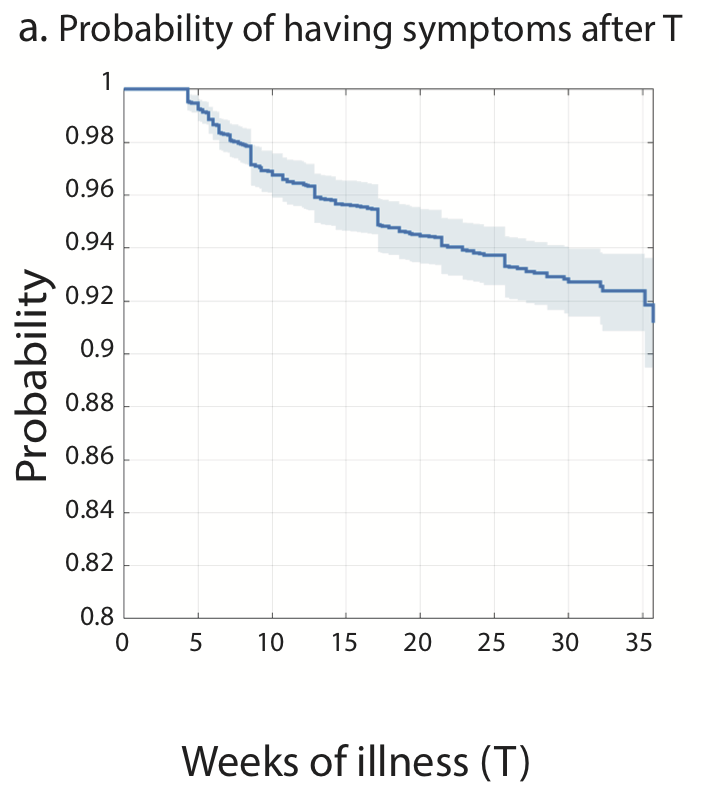
Of the 3762 respondents, 2454 experienced symptoms for at least 180 days (6 months). 257 respondents (6.8%) recovered after day 28 of illness. In this Long COVID cohort The probability of symptoms lasting beyond 35 weeks was 91.8%.
2/
2/
The majority of respondents reported “moderate” symptoms throughout the course.
In those who recovered in less than 90 days, the average number of symptoms peaked at week2 (11.35); in those who did not recover in 90 days, the average # of symptoms peaked at month2 (17.16!) 3/
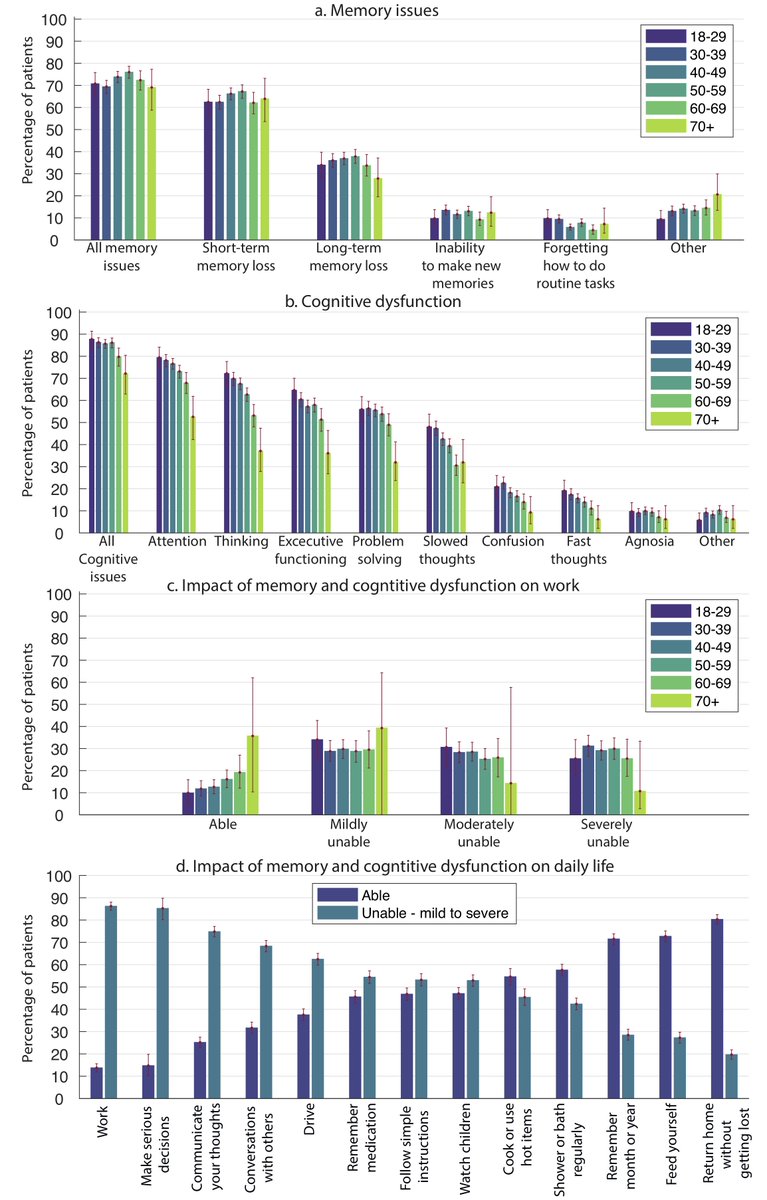
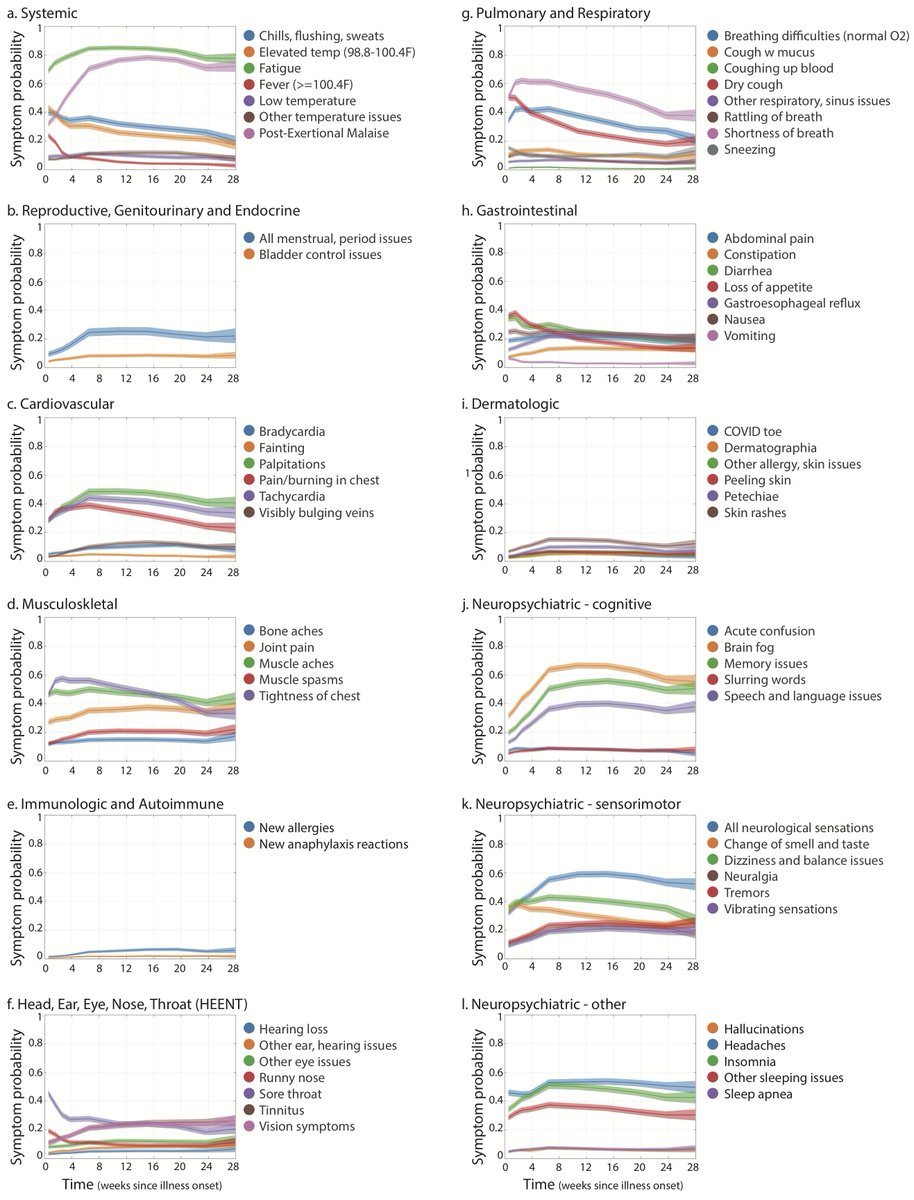
Prevalence of 205 symptoms in 10 organ systems was estimated, with 66 symptoms traced over seven months. We had special focus on neurological/psychiatric symptoms (calling them neuropsychiatric)
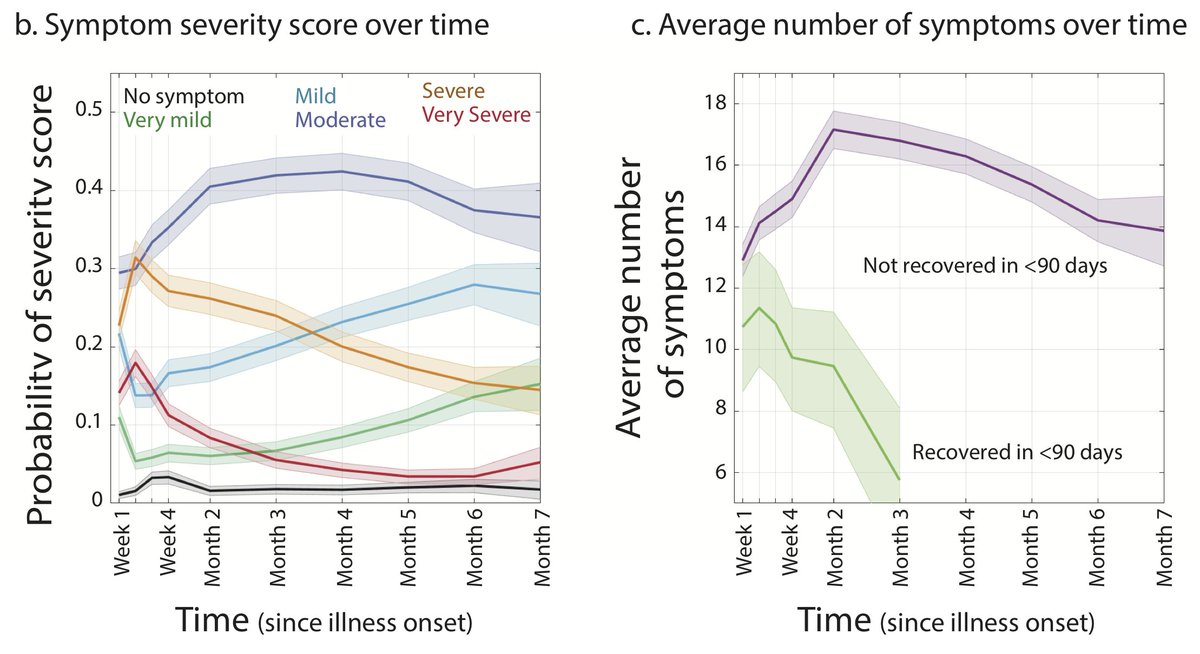
Here's symptom prevalence estimates for non-neuropsychiatric symptoms. 4/
Here's symptom prevalence estimates for non-neuropsychiatric symptoms. 4/
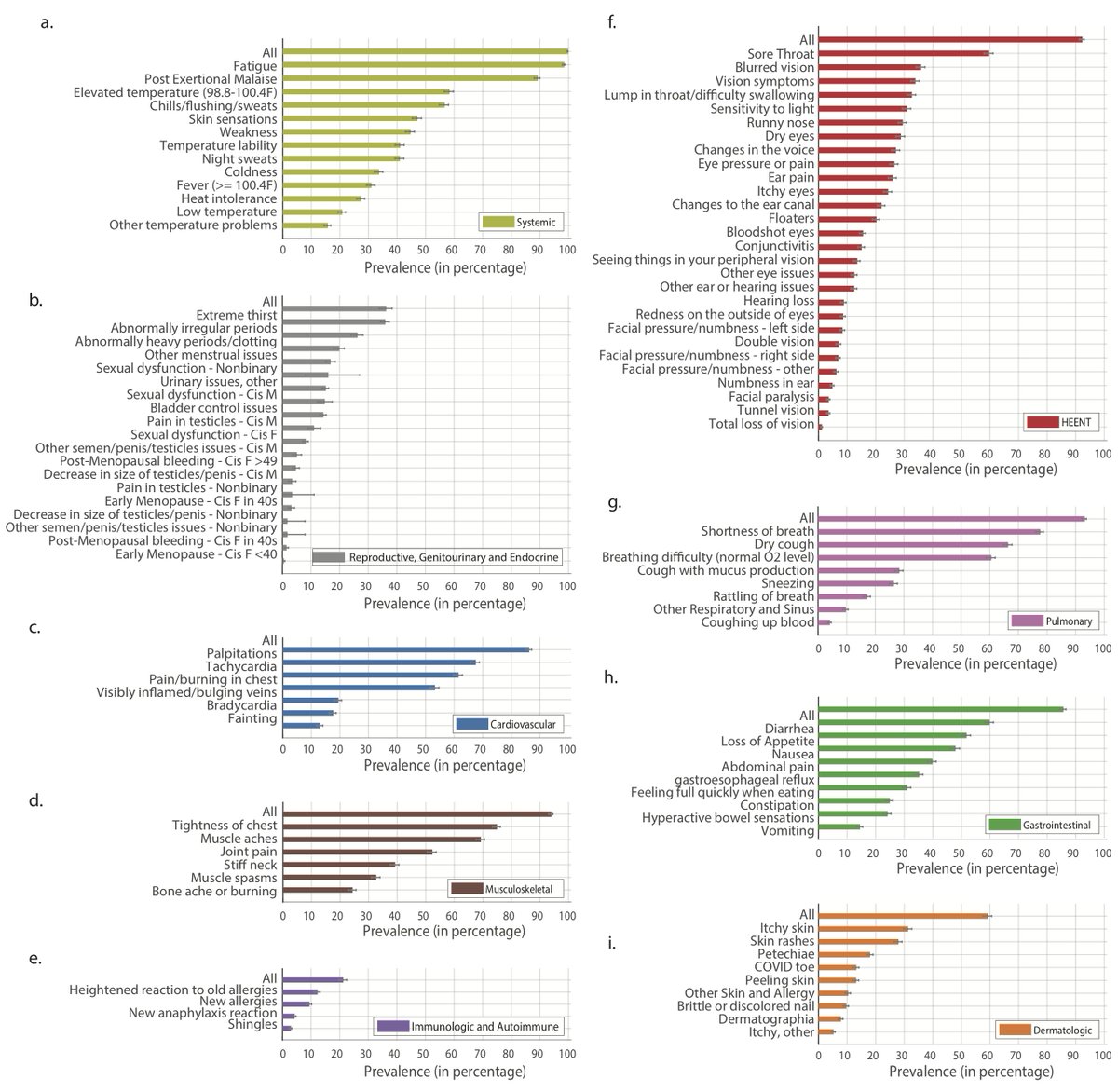
and prevalence estimates for neuropsychiatric symptoms in 9 groups:
-Cognitive Functioning (>85%)
-Memory (>70%)
-Speech and Language (~50%)
-Sensorimotor symptoms (>90%)
-Sleep (~80%)
-Headaches (~80%)
-Emotion and Mood (~90%)
-Taste and Smell (~60%)
-Hallucinations (>15%)
5/
-Cognitive Functioning (>85%)
-Memory (>70%)
-Speech and Language (~50%)
-Sensorimotor symptoms (>90%)
-Sleep (~80%)
-Headaches (~80%)
-Emotion and Mood (~90%)
-Taste and Smell (~60%)
-Hallucinations (>15%)
5/
88.0% of the total respondents (3310) experienced either cognitive dysfunction or memory loss, with substantial impact on daily life, particularly Work.
These symptoms had similar impacts across all age groups. 6/
These symptoms had similar impacts across all age groups. 6/
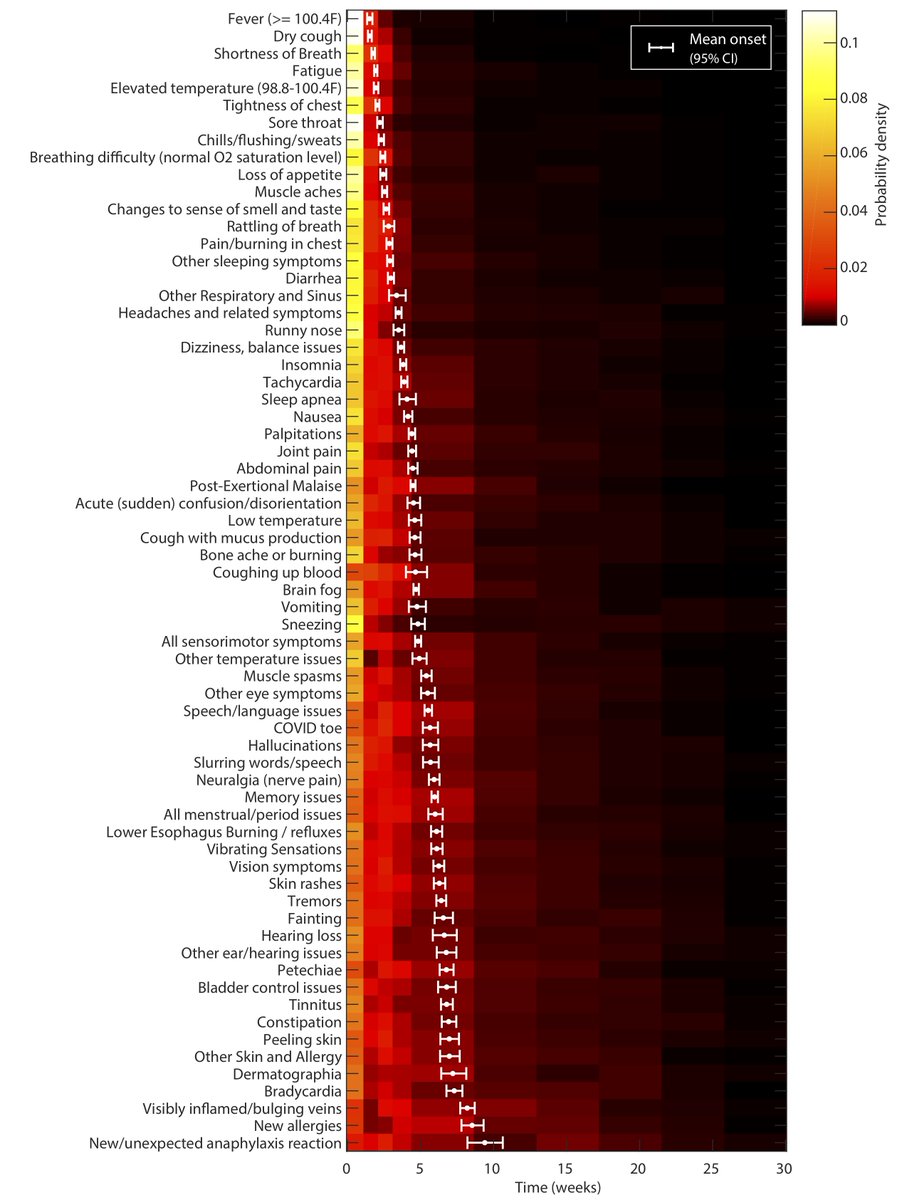
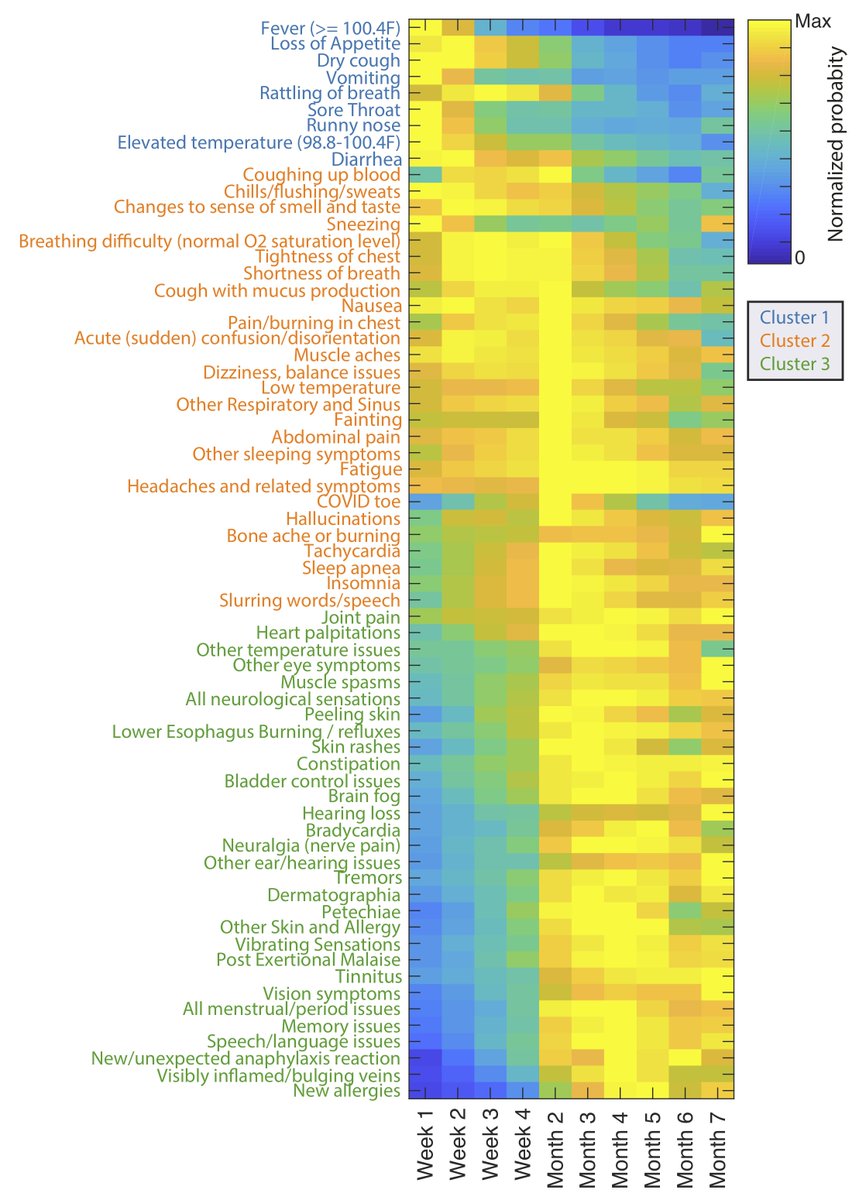
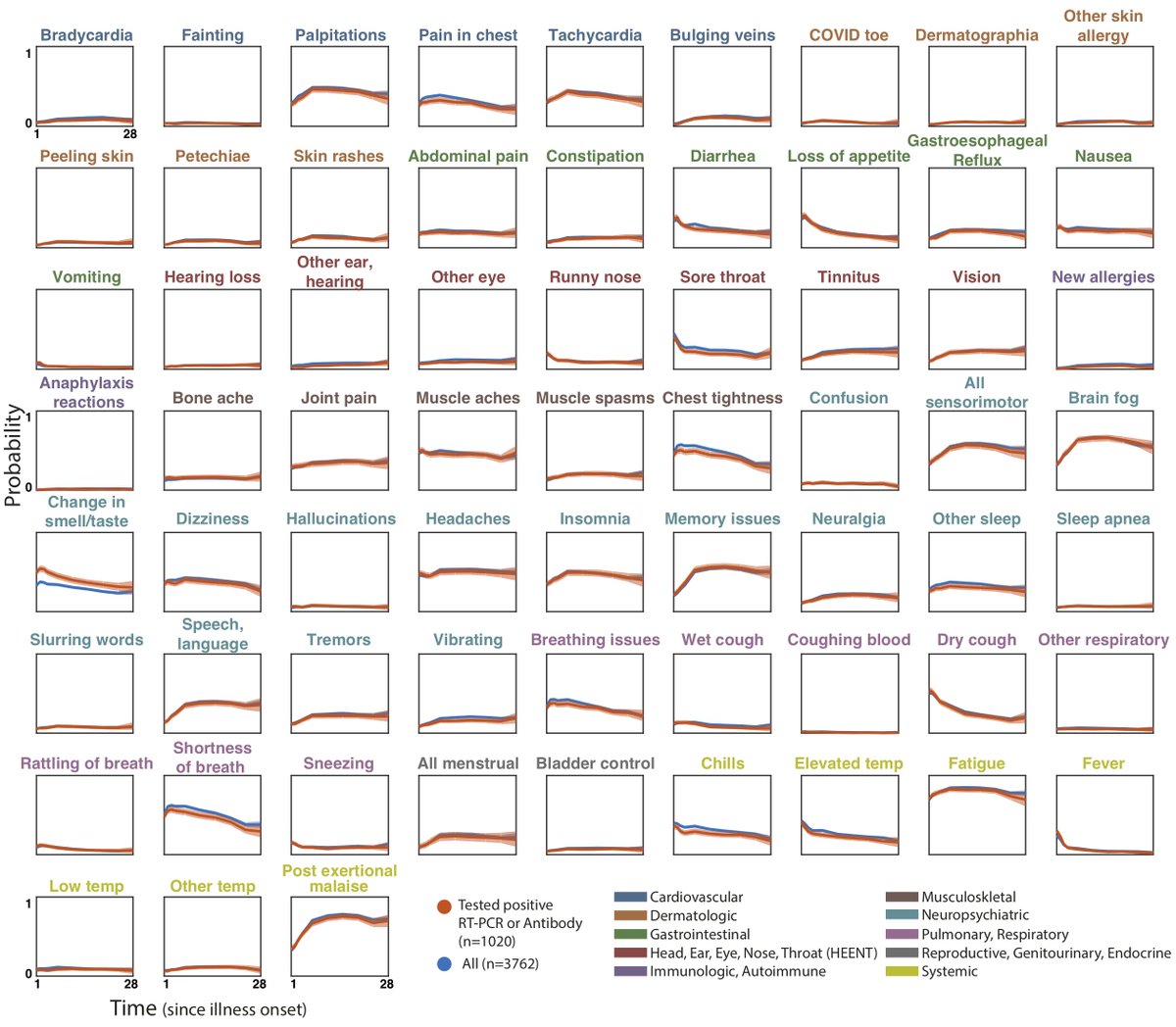
To characterize the progression of the 66 symptoms over seven months, we estimated symptom time courses—the probability of experiencing each symptom at each time point, given that recovery has not yet occurred. 7/
We also estimated the distribution of onset times for each symptom.
White points and error bars show the mean onset time and 95% pointwise confidence intervals. As you can see, some symptoms are most likely to start in the 1st week, whereas others would start later (month 2) 8/
White points and error bars show the mean onset time and 95% pointwise confidence intervals. As you can see, some symptoms are most likely to start in the 1st week, whereas others would start later (month 2) 8/
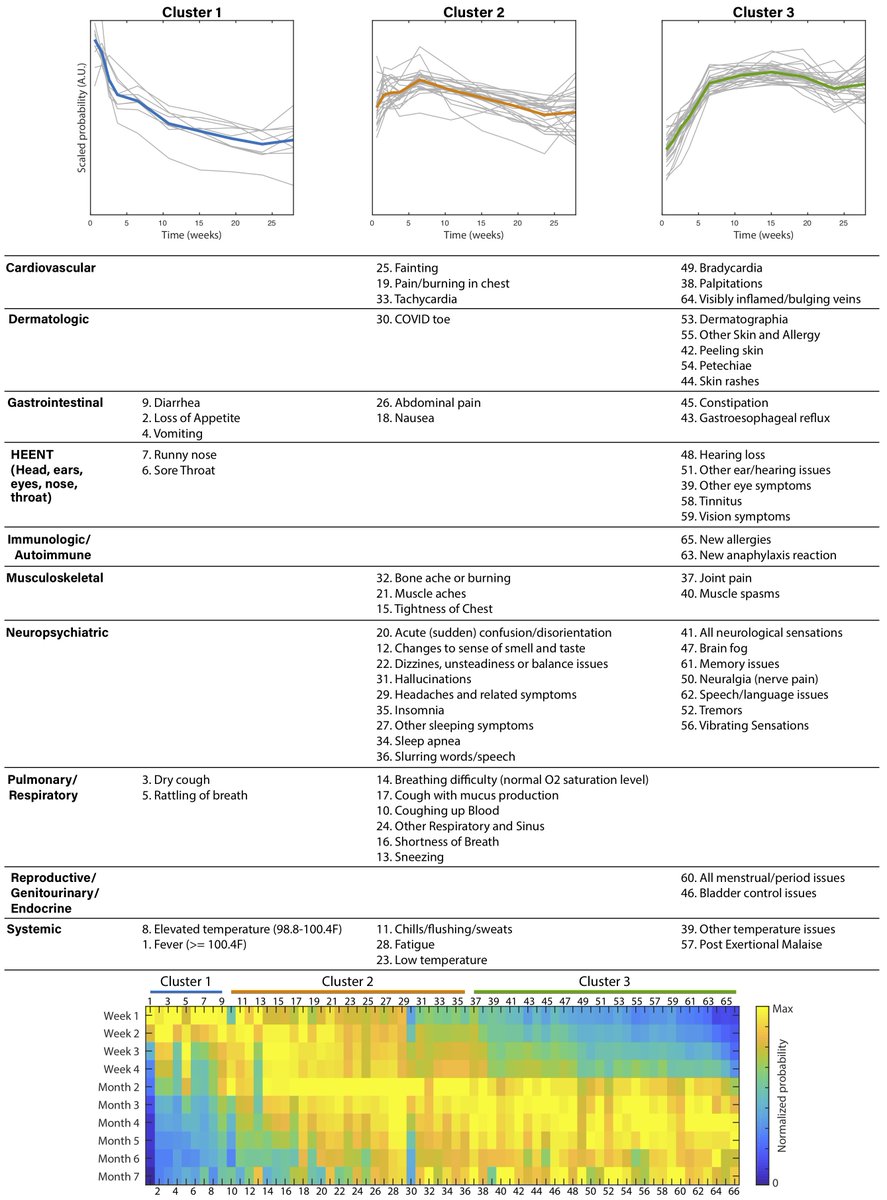
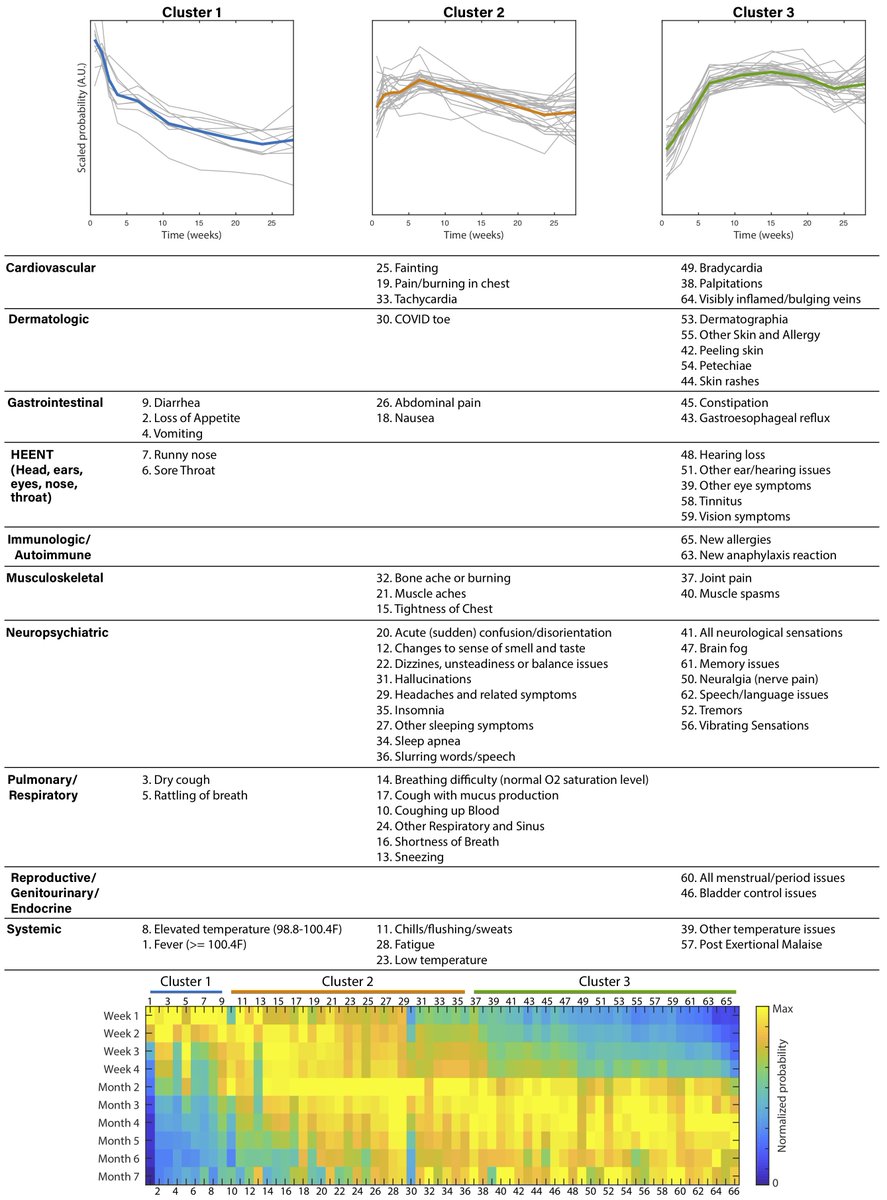
To summarize general patterns in the progression of symptoms over time, we used a clustering algorithm to group theses symptms into 3 clusters, according to the shapes of their time courses (i.e. changes in relative amplitude over time, ignoring their overall prevalence) 9/
Cluster 1: symptoms with early peak (the first 2 or 3 weeks), then a decreasing trend in probability over time
Cluster 2: symptoms w a slow decrease, slow increase, or unchanging probability over time
Cluster 3: symptoms w sharp ramp in the first 2 months, then plateau
10/
Cluster 2: symptoms w a slow decrease, slow increase, or unchanging probability over time
Cluster 3: symptoms w sharp ramp in the first 2 months, then plateau
10/
The mean # of organ systems affected in each respondent was 9.08/10. Symptoms in the same organ-based category didn't necessarily cluster together & could appear across clusters
Systemic & neuro/cognitive symptoms were most likely to persist from disease onset to month 7
11/
Systemic & neuro/cognitive symptoms were most likely to persist from disease onset to month 7
11/
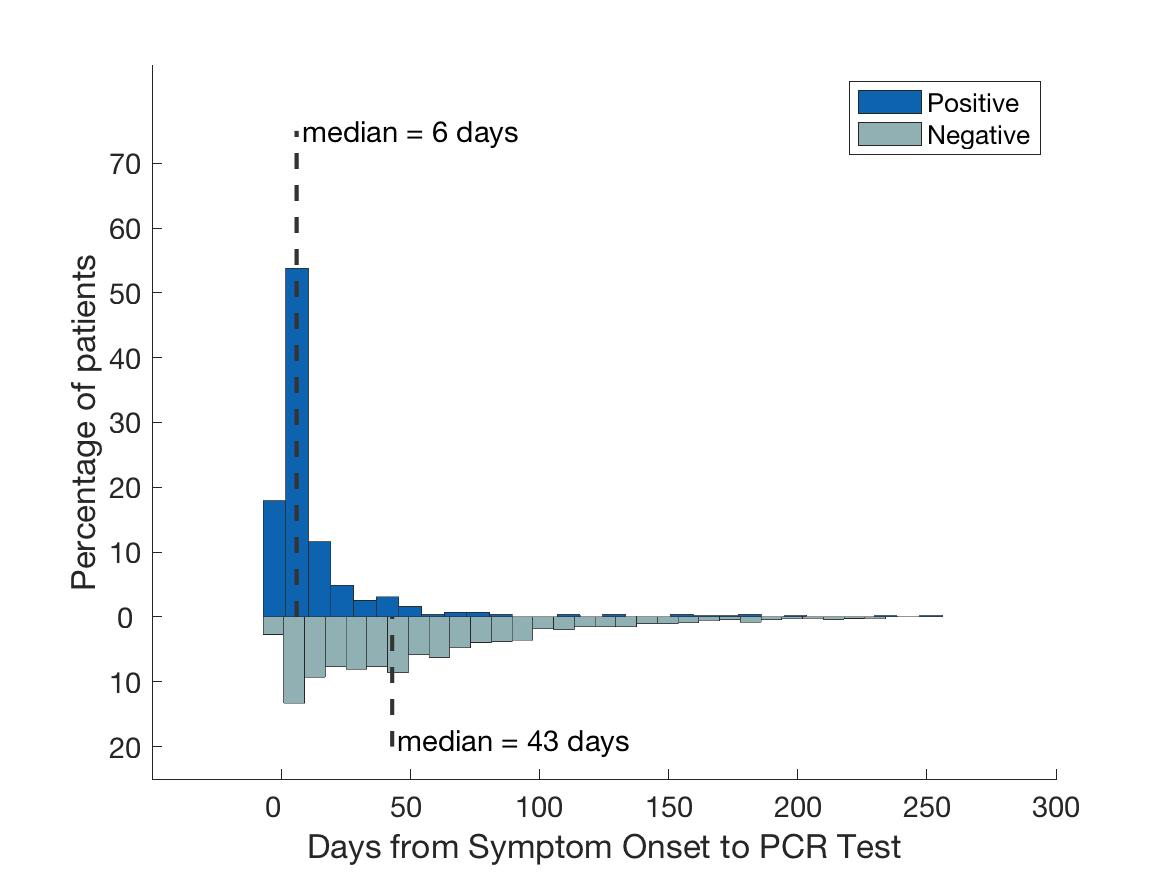
Did all respondents test + for COVI19? No.
1730 tested negative & 600 tested positive (RT-PCR). Difference? The median number of days between first experiencing symptoms & being tested was 6 days for those who tested + and 43 days for those who tested -.
12/
1730 tested negative & 600 tested positive (RT-PCR). Difference? The median number of days between first experiencing symptoms & being tested was 6 days for those who tested + and 43 days for those who tested -.
12/
Out of 205 symptoms, only loss of smell/taste was significantly different between the two groups, after stratifying the data based on comparing populations with equal test times. This is consistent with what we found in our first study. See here:
13/ https://twitter.com/AthenaAkrami/status/1260189116051963909?s=20
13/ https://twitter.com/AthenaAkrami/status/1260189116051963909?s=20
Moreover, symptom probability time courses for participants with confirmed COVID-19 (n=1020, RT-PCR, antigen, or antibody tests) overlapped significantly with probability estimates from the whole population, except again for "Changes in smell/taste".
14/
14/
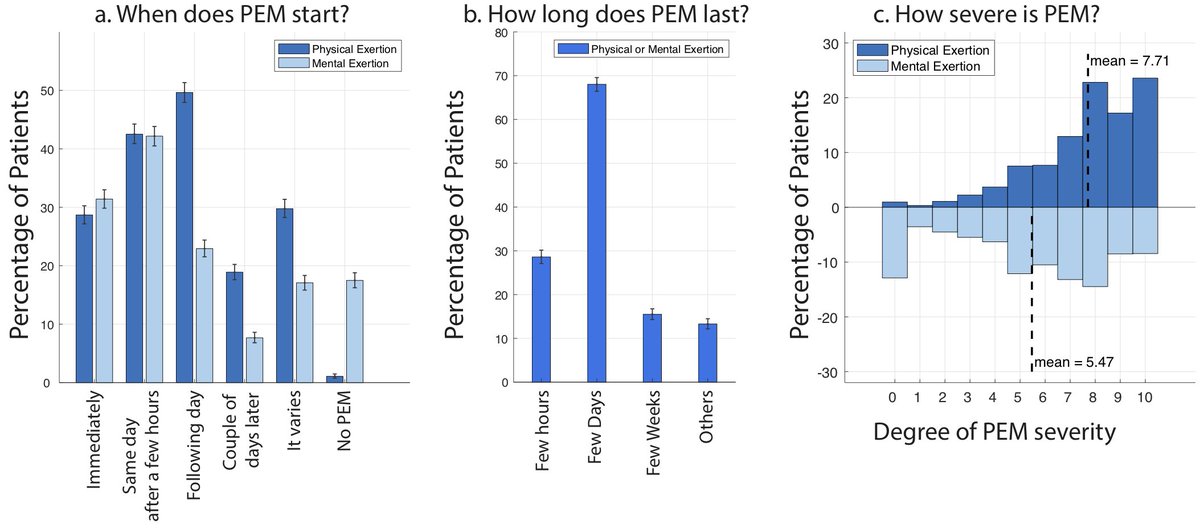
Going back to symptoms, 89.1% of participants reported experiencing either physical or mental Post-Exertional Malaise: "worsening or relapse of symptoms after physical or mental activity" one of the most demoralising features of #LongCOVID
/15
/15
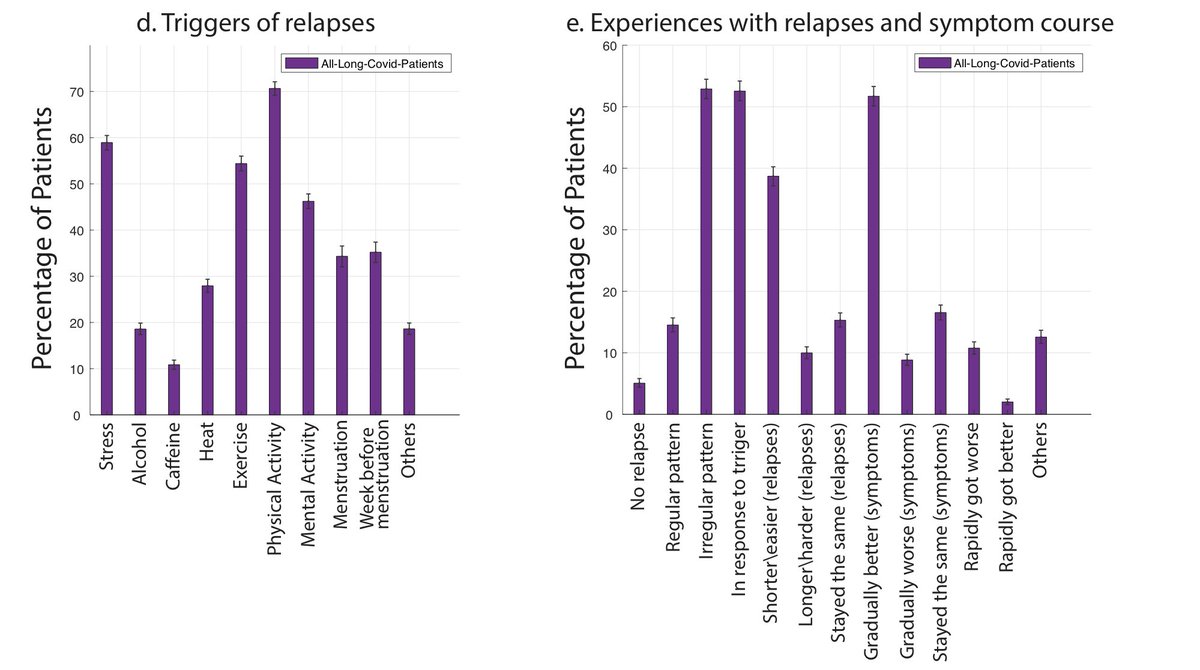
Majority of respondents experienced PEM after a few hours or the following day, and it can last for a few days.
Physical activity, stress, exercise, and mental activity were the most reported triggers of these relapses.
16/
Physical activity, stress, exercise, and mental activity were the most reported triggers of these relapses.
16/
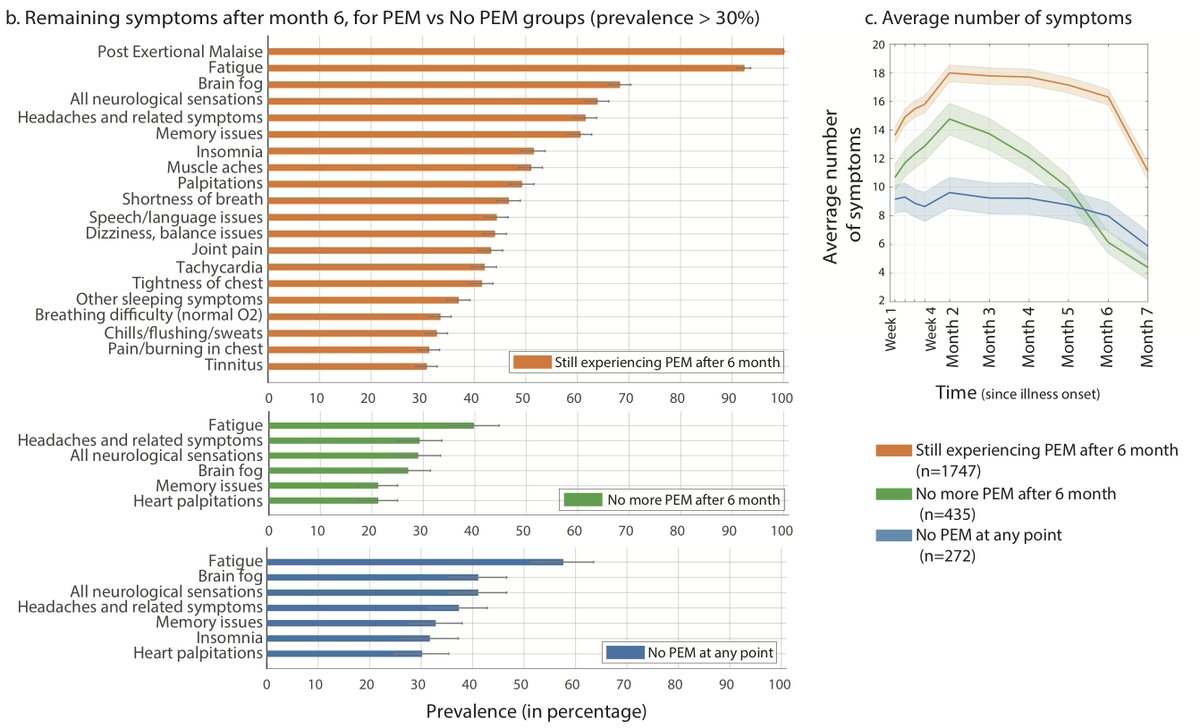
Those who still experience PEM after 6 month, on average experience a lot more symptoms, compared to those w no PEM.
PEM is a mandatory symptom for ME/CFS. Intriguingly, among those still experiencing symptoms at month 6 w no PEM, fatigue was still the most common symptom
17/
PEM is a mandatory symptom for ME/CFS. Intriguingly, among those still experiencing symptoms at month 6 w no PEM, fatigue was still the most common symptom
17/
This suggests that while a subset of the #LongCOVID population may meet #MECFS diagnostic criteria, there remains a subpopulation w significant fatigue who do not meet the criteria & therefore the mechanisms of fatigue require further investigation.
18/
18/
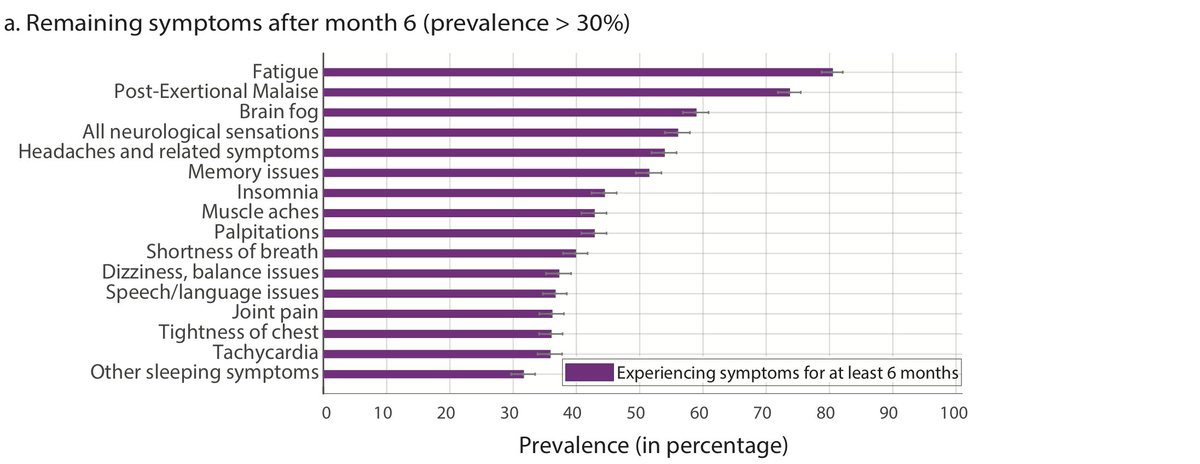
A total of 2454 (65.2%) respondents were experiencing symptoms for at least 6 months. For this population, the top remaining symptoms after 6 months were primarily a combination of systemic and neurological symptoms.
19/
19/
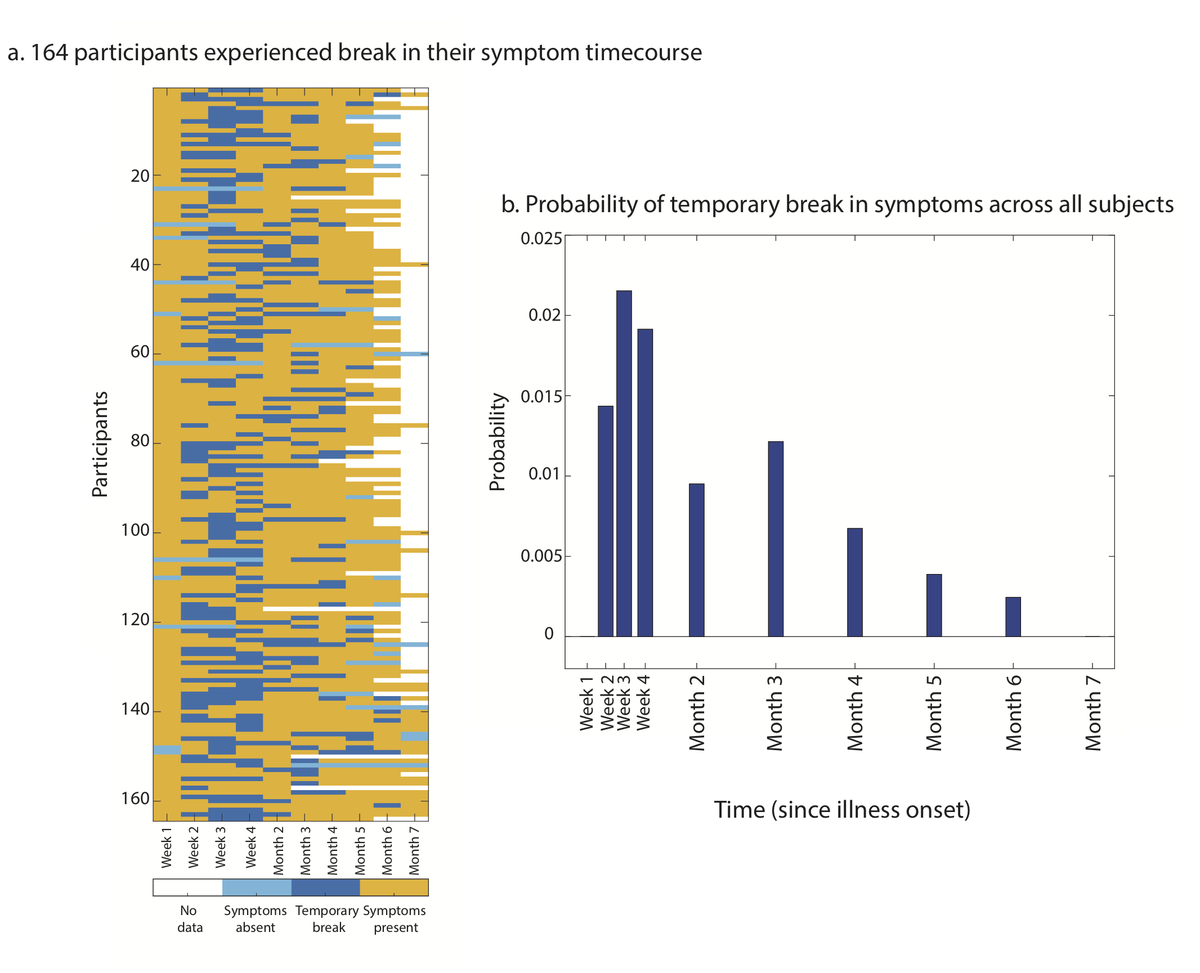
You may wonder, do patients usually have break in their symptoms? Only 164 out of 3762 participants (4.4%) experienced a temporary break in symptoms (to the precision of our study, which is week 1-4, then month 2-7)
20/
20/
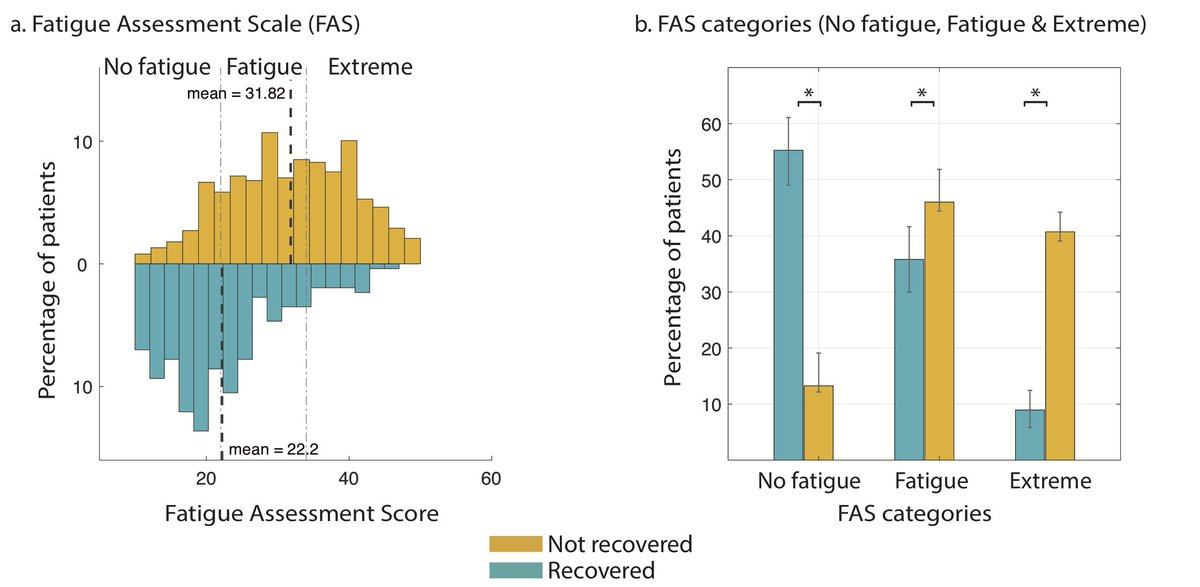
We also asked participants to answer the Fatigue Assessment Scale (FAS) questionnaire, based on their subjective report during the “past 1 week".
Majority of unrecovered respondents fall in "Fatigued" and "Severely Fatigued", compared to recovered.
21/
Majority of unrecovered respondents fall in "Fatigued" and "Severely Fatigued", compared to recovered.
21/
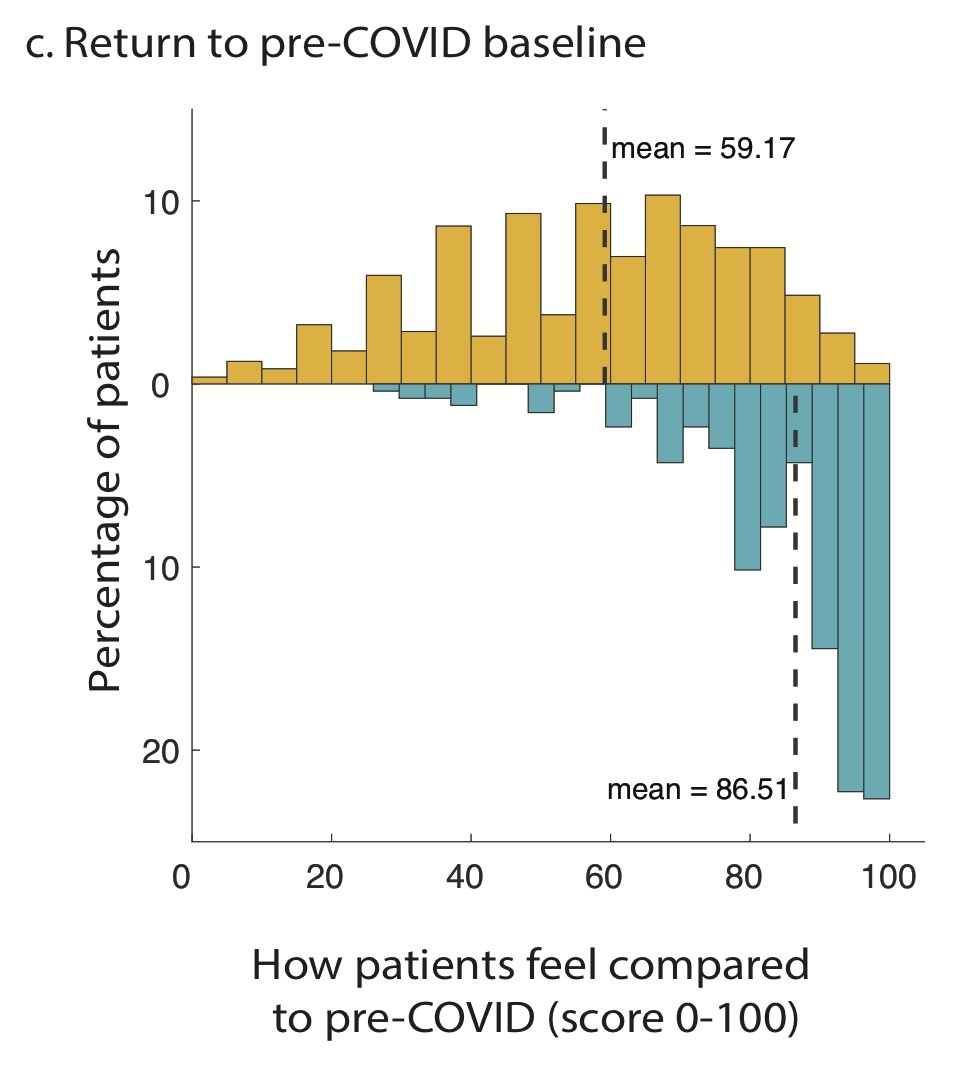
Respondents were also asked, “How would you rate how you feel today, on a scale of 0-100% (with 100% being your pre-COVID baseline)?"
Unrecovered participants reported a mean score of 59.2, while recovered participants reported a mean score of 86.5.
22/
Unrecovered participants reported a mean score of 59.2, while recovered participants reported a mean score of 86.5.
22/
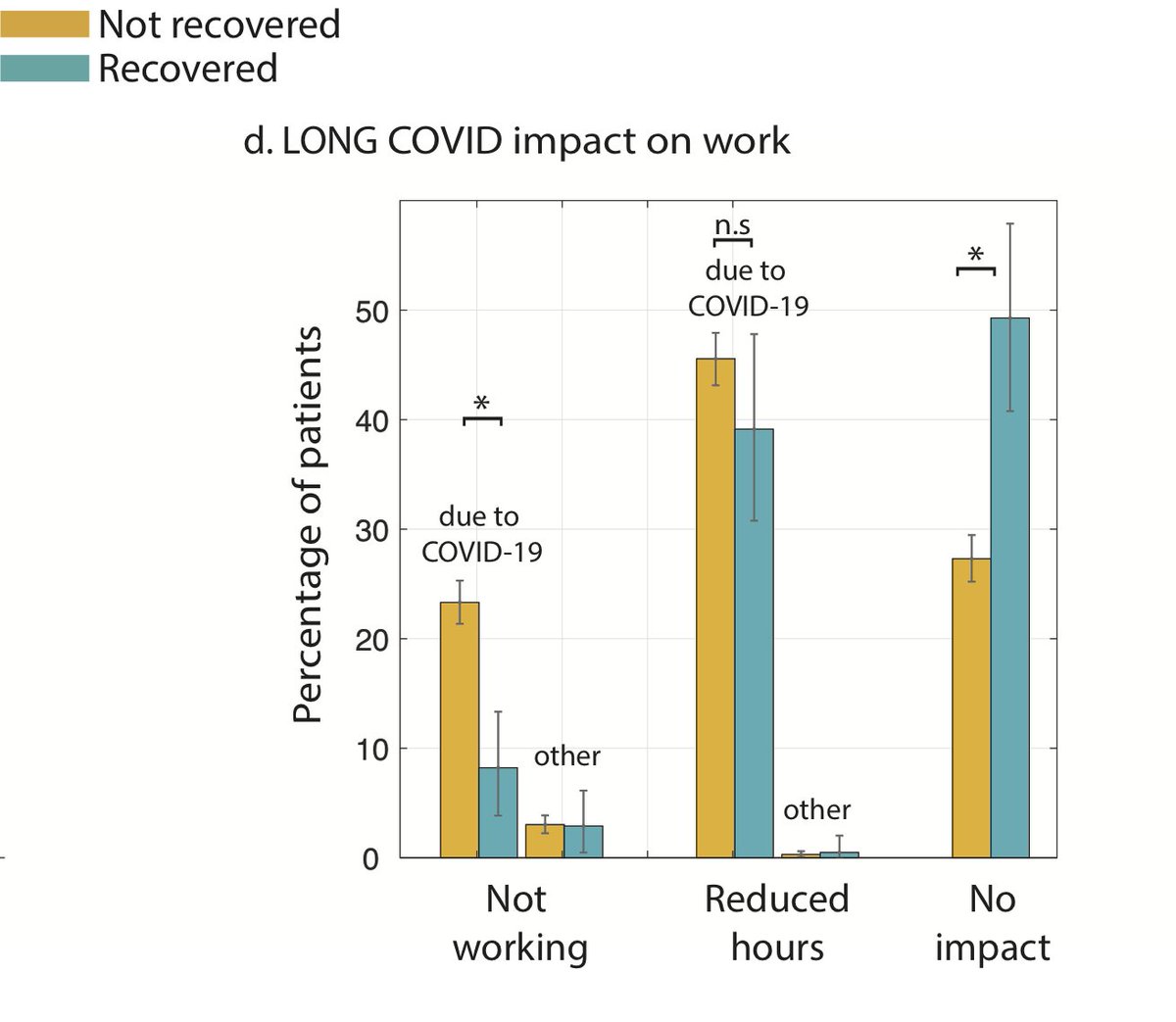
AND most importantly, 45.2% of respondents reported requiring a reduced work schedule compared to pre-illness. 22.3% were not working due to their health conditions. Unrecovered ones were impacted stronger (68.9% reported reduced work hrs or not working at all). This is HUGE
23/
23/
We hope this work would help with valuable future research to answer: What are the biological underpinnings of #LongCOVID & what are potential treatments? What can be done to support the suffers, both medically & through policy, until treatments are identified?
24/
24/

 Read on Twitter
Read on Twitter