As the year comes to a close, here's one more discussion on pediatric ambulatory #bloodpressure monitoring...this time, let's discuss the use of BP load and how it came to be part of the pediatric ABPM analysis criteria. 1/
What is load? By definition, it's the percentage of high readings in a given time period during ABPM, comparing each BP reading to a set threshold. In essence it captures the cumulative effect of the high readings during that time period. 2/
How did this value find its way into the pediatric ABPM criteria? For that, we can blame Drs. Lurbe, Sorof and Daniels who published this paper in 2004. It was one of the first comprehensive reviews of ABPM in children. 3/ https://pubmed.ncbi.nlm.nih.gov/14722512/
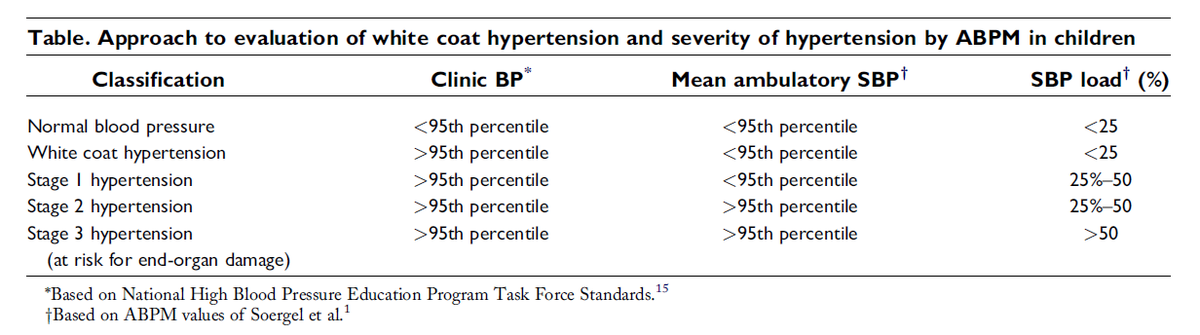
In it, they published this table which was their expert opinion of how ABPM studies in children should be classified: 4/
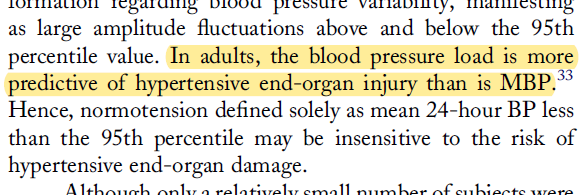
They made the decision to include load into the criteria based on one study conducted in adults - 5/
That study (White et al 1989) can be found here: 6/ https://pubmed.ncbi.nlm.nih.gov/2529749/
And there is an earlier review by Dr. White on the use of BP load (not cited by Lurbe at al) here: 7/ https://pubmed.ncbi.nlm.nih.gov/1301258/
But I digress - back to pediatric ABPM.
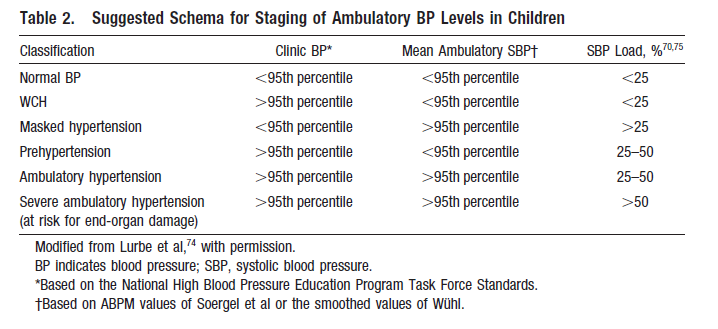
In 2008, the @AHAScience convened a group of experts in pediatric ABPM to develop a consensus approach to pediatric ABPM interpretation. That group revised and refined the classification scheme of Lurbe at al and published this table: 8/
In 2008, the @AHAScience convened a group of experts in pediatric ABPM to develop a consensus approach to pediatric ABPM interpretation. That group revised and refined the classification scheme of Lurbe at al and published this table: 8/
The full paper can be found here: 9/
https://www.ahajournals.org/doi/pdf/10.1161/HYPERTENSIONAHA.108.190329
https://www.ahajournals.org/doi/pdf/10.1161/HYPERTENSIONAHA.108.190329
And in 2014, the table was updated in this paper, which is the currently used standard for pediatric ABPM: 10/ https://pubmed.ncbi.nlm.nih.gov/24591341/
However, the question is, do we really need load to interpret ABPM? It has been carried forward in pediatrics w/0 much critical examination (IMHO). It's not used in the adult criteria - the early data by White did not carry forward. (perhaps @jordy_bc can explain why) 11/
And, even the @ESHypertension pediatric hypertension guideline published in 2016 by Lurbe et al (yes, the same author) has dropped load from their interpretation criteria: 12/ https://pubmed.ncbi.nlm.nih.gov/27467768/
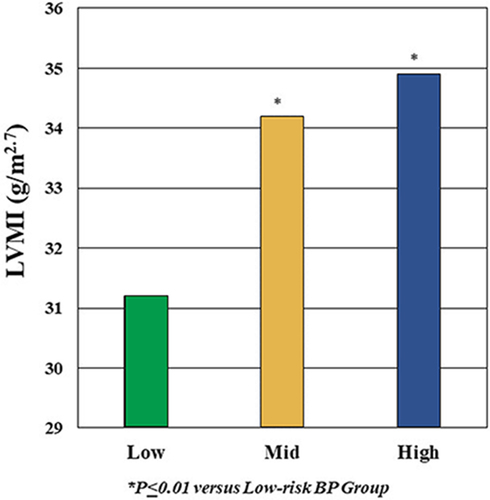
So do we need it? Data from the SHIP-AHOY study have shown that mean office SBP is the strongest predictor of increased left ventricular mass. Here we showed that as mean SBP increased, LV mass increased (starting at office BP <90th percentile, BTW): 13/
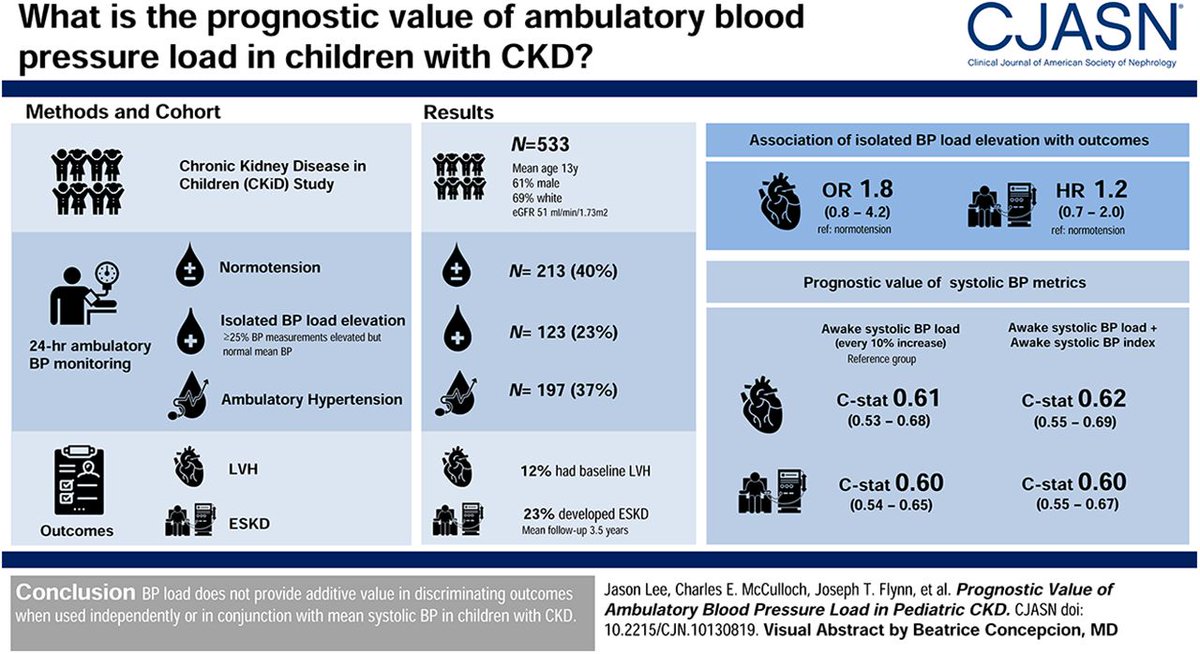
We have also looked at BP load in children with chronic #kidney disease and have found that use of BP load di not add to the prediction of GFR decline or to prediction of LVH 15/
But what about children without CKD? Is BP load necessary to interpret ABPM? Does it improve prediction of target organ damage? Stay tuned - we have another paper from SHIP-AHOY that will answer that question! 16/
And, in 2021 we will be revising the pediatric ABPM criteria, again under the auspices of @AHAScience. I have a feeling that I know what the next classification table will look like 17/
Until then, though, when @HalbachSusan, Coral Hanevold and I interpret ABPM at @seattlechildren, we're still using load criteria - are you? 18/18

 Read on Twitter
Read on Twitter