Hello everyone! We're here with another #IMPOCUS case for those of you as excited about pocus as you are about the holidays.
65 yo F w hx HFpEF, COPD on 3L O2 at home who presents after a recent CHF admission (diuresed and improved) with fevers, SOB, and diarrhea. COVID+.
1/
65 yo F w hx HFpEF, COPD on 3L O2 at home who presents after a recent CHF admission (diuresed and improved) with fevers, SOB, and diarrhea. COVID+.
1/
2/
She is HDS without significant respiratory distress, requiring 4L O2.
Before we start, some polls for you all:
1. How often do you find lung POCUS useful in COVID19?
She is HDS without significant respiratory distress, requiring 4L O2.
Before we start, some polls for you all:
1. How often do you find lung POCUS useful in COVID19?
3/
(poll) Do you feel lung POCUS can help distinguish between cardiogenic pulmonary edema and COVID19 PNA?
(poll) Do you feel lung POCUS can help distinguish between cardiogenic pulmonary edema and COVID19 PNA?
4/
Back to our patient. 94% on 4L. HR 110, BP 120/80. Exam notable for crackles bilaterally, unable to appreciate JVP, trace lower extremity edema. Takes 40 mg furosemide daily at home. His Cr is normal, has not had much appetite over past day or so.
Representative CXR:
Back to our patient. 94% on 4L. HR 110, BP 120/80. Exam notable for crackles bilaterally, unable to appreciate JVP, trace lower extremity edema. Takes 40 mg furosemide daily at home. His Cr is normal, has not had much appetite over past day or so.
Representative CXR:
5/
POLL: Pre-POCUS, what would you do with volume?
POLL: Pre-POCUS, what would you do with volume?
7/
1R / RT AP
1R / RT AP
8/
4R/RT AX
4R/RT AX
9/
1L/ LT AP
1L/ LT AP
10/
3L / LT AX
3L / LT AX
11/
RT POST/ 6R
RT POST/ 6R
12/
RT POST / 5R
RT POST / 5R
13/
LT POST/ 6L
LT POST/ 6L
14/
LT POST / 5L
LT POST / 5L
15/
Focused bedside cardiac echo performed which revealed preserved LV function, no pericardial effusion, normal RV with the following IVC view:
Focused bedside cardiac echo performed which revealed preserved LV function, no pericardial effusion, normal RV with the following IVC view:
16/
POLL - Are the lung ultrasound findings here predominantly due to COVID19 pneumonitis or cardiogenic pulmonary edema?
POLL - Are the lung ultrasound findings here predominantly due to COVID19 pneumonitis or cardiogenic pulmonary edema?
17/
Post POCUS, what would you do with volume?
Post POCUS, what would you do with volume?
18/
This lung ultrasound was interpreted as predominantly B-profile with some areas showing subpleural consolidations and thickened pleura, specifically 6L:
This lung ultrasound was interpreted as predominantly B-profile with some areas showing subpleural consolidations and thickened pleura, specifically 6L:
19/
The image above is a classic finding in COVD19 pnuemonitis, revealing confluent B lines, irregular pleura, and subpleural consolidations. In comparison, B-lines in the setting of pulmonary edema often appear more like this image:
The image above is a classic finding in COVD19 pnuemonitis, revealing confluent B lines, irregular pleura, and subpleural consolidations. In comparison, B-lines in the setting of pulmonary edema often appear more like this image:
20/
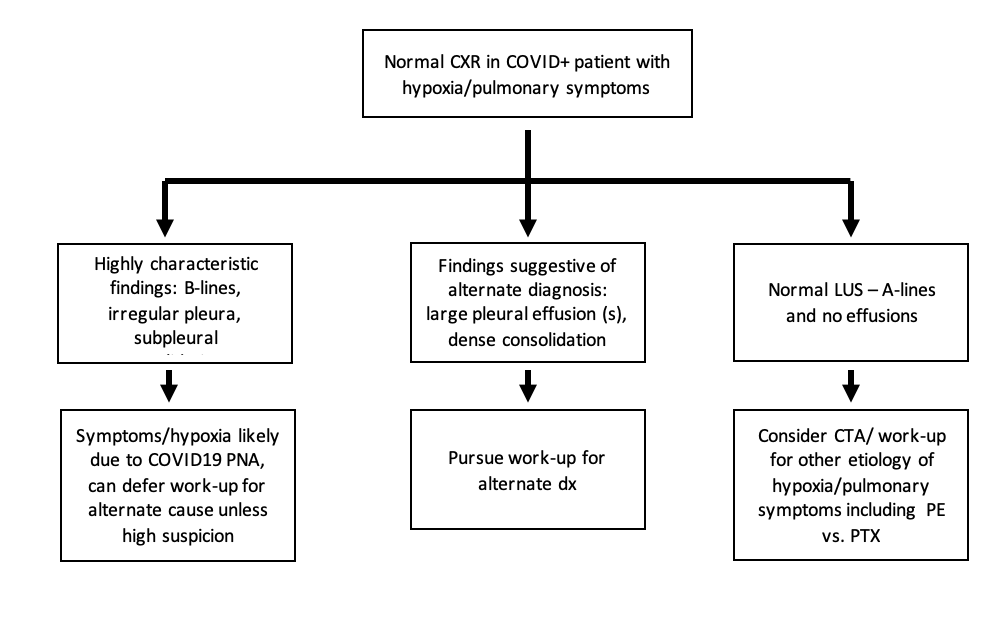
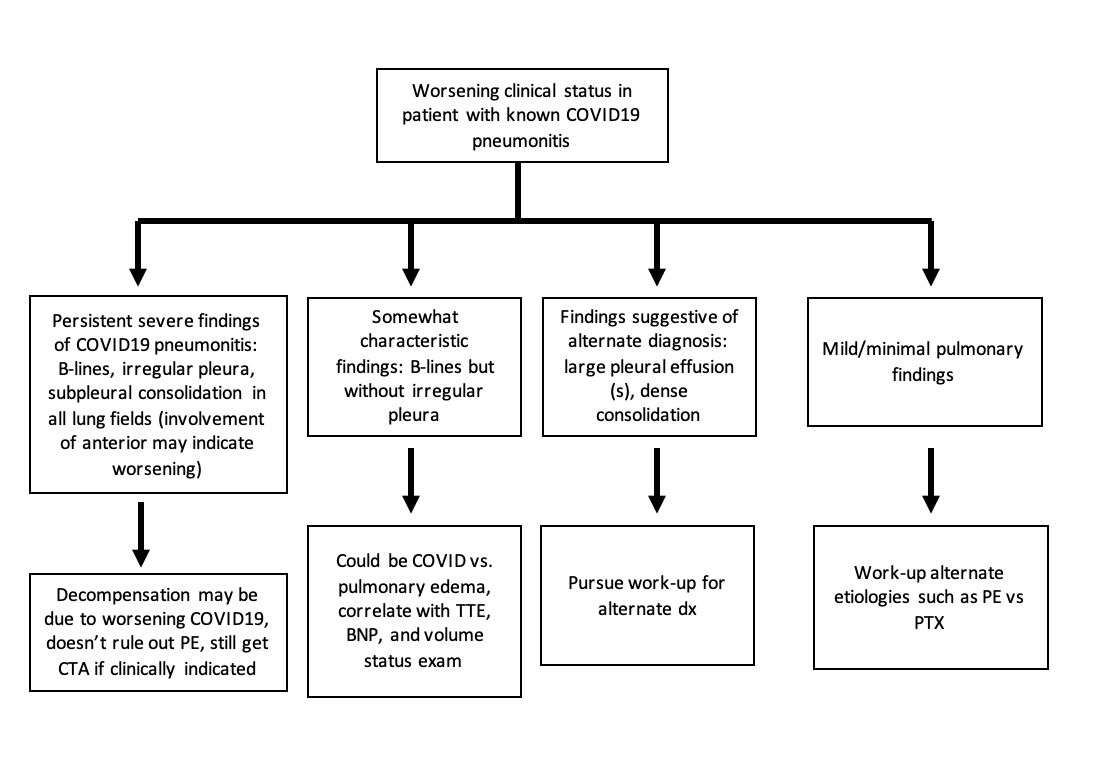
So, is it possible to distinguish between COVID19 pneumonitis and cardiogenic pulmonary edema on lung ultrasound?
Unclear, but our opinion: not really (100% open to other ideas!). Here is a table summarizing our thoughts on how lung POCUS could be used in COVID19 PNA:
So, is it possible to distinguish between COVID19 pneumonitis and cardiogenic pulmonary edema on lung ultrasound?
Unclear, but our opinion: not really (100% open to other ideas!). Here is a table summarizing our thoughts on how lung POCUS could be used in COVID19 PNA:
21/
In sum, either variation of B lines could be found in both COVID19 pneumonitis and pulmonary edema, so its hard to tease these out. The one thing that may help is the presence of bilateral pleural effusions to point towards pulmonary edema over COVID.
In sum, either variation of B lines could be found in both COVID19 pneumonitis and pulmonary edema, so its hard to tease these out. The one thing that may help is the presence of bilateral pleural effusions to point towards pulmonary edema over COVID.
22/
Incorporating findings with cardiac POCUS and #VEXUS for our vexus lovers could be useful, but this is more nuanced and challenging for beginning POCUS-ers. There is one article that does discuss this: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7675430/
Incorporating findings with cardiac POCUS and #VEXUS for our vexus lovers could be useful, but this is more nuanced and challenging for beginning POCUS-ers. There is one article that does discuss this: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7675430/
23/
In this case, the absence of pleural effusions, collapsible IVC, and a patient who had been on diuretics at home with decreased appetite / PO intake in the setting of COVID19 was thought to be c/w the patient being on the dry side, so diuresis was held but no IVF was given.
In this case, the absence of pleural effusions, collapsible IVC, and a patient who had been on diuretics at home with decreased appetite / PO intake in the setting of COVID19 was thought to be c/w the patient being on the dry side, so diuresis was held but no IVF was given.
24/
But, there are no right answers and it wouldn't have been wrong to trial diuresis as well, as its likely beneficial to remain more dry if tolerable from a kidney, BP standpoint.
So when IS (lung) #POCUS useful in COVID19?
But, there are no right answers and it wouldn't have been wrong to trial diuresis as well, as its likely beneficial to remain more dry if tolerable from a kidney, BP standpoint.
So when IS (lung) #POCUS useful in COVID19?
25/
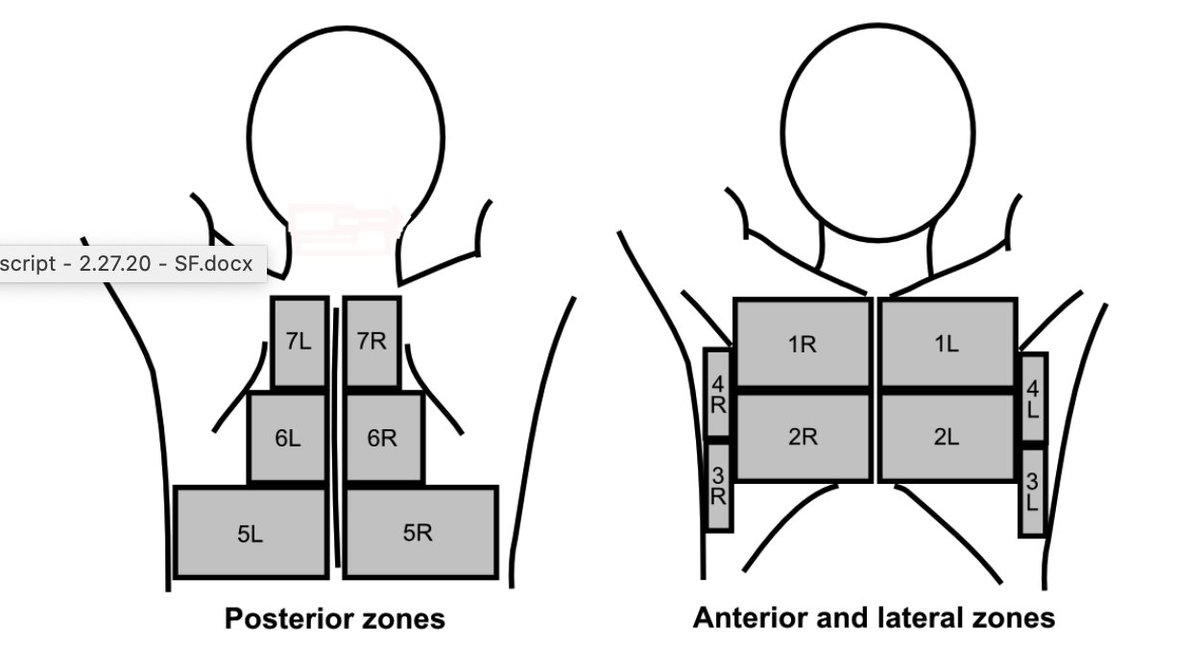
We propose 3 basic scenarios in which #POCUS can be useful with corresponding workflows of how to interpret potential findings.
1. Negative COVID19 test with high clinical suspicion.
We propose 3 basic scenarios in which #POCUS can be useful with corresponding workflows of how to interpret potential findings.
1. Negative COVID19 test with high clinical suspicion.
28/
Finally, we will finish off with a big shoutout to @IM_POCUS and and the CIMUS who came up with this expert consensus statement that is far more detailed and very well thought out: https://onlinelibrary.wiley.com/doi/full/10.1002/jum.15571#.X85em1RQ44g.twitter
Finally, we will finish off with a big shoutout to @IM_POCUS and and the CIMUS who came up with this expert consensus statement that is far more detailed and very well thought out: https://onlinelibrary.wiley.com/doi/full/10.1002/jum.15571#.X85em1RQ44g.twitter
29/
Thanks for reading, exciting times for #IMPOCUS, appreciate any and all thoughts on how everyone else has been using #POCUS during the pandemic.
Tagging POCUS friends:
@msenussiMD @iceman_ex @kyliebaker888 @collinflan @katiewiskar @Wilkinsonjonny @siddharth_dugar
Thanks for reading, exciting times for #IMPOCUS, appreciate any and all thoughts on how everyone else has been using #POCUS during the pandemic.
Tagging POCUS friends:
@msenussiMD @iceman_ex @kyliebaker888 @collinflan @katiewiskar @Wilkinsonjonny @siddharth_dugar
30/
@ria_dancel @ArgaizR @RogerAlvarezDO @laxswamy @emily_fri @cameron_baston @hraza222 @bryanboling @virenkaul @pedrodammert @criticalcareuk @redneeraj @ccpractitioner @ThinkingCC @cianmcdermott @jtanguay11 @TimRowesays @jelevenson @khldtaha
@DRsonosRD @NephroP @DrGalenMD
@ria_dancel @ArgaizR @RogerAlvarezDO @laxswamy @emily_fri @cameron_baston @hraza222 @bryanboling @virenkaul @pedrodammert @criticalcareuk @redneeraj @ccpractitioner @ThinkingCC @cianmcdermott @jtanguay11 @TimRowesays @jelevenson @khldtaha
@DRsonosRD @NephroP @DrGalenMD
31/
@buckeye_sanjay @Cometin007 @ScottTiltonCRNP @jminardi21 @drshahrul80 @JCHCheung
And a special shoutout (that should have come MUCH earlier in the thread!!!) to @ortizcx12 for these images!!
@buckeye_sanjay @Cometin007 @ScottTiltonCRNP @jminardi21 @drshahrul80 @JCHCheung
And a special shoutout (that should have come MUCH earlier in the thread!!!) to @ortizcx12 for these images!!

 Read on Twitter
Read on Twitter