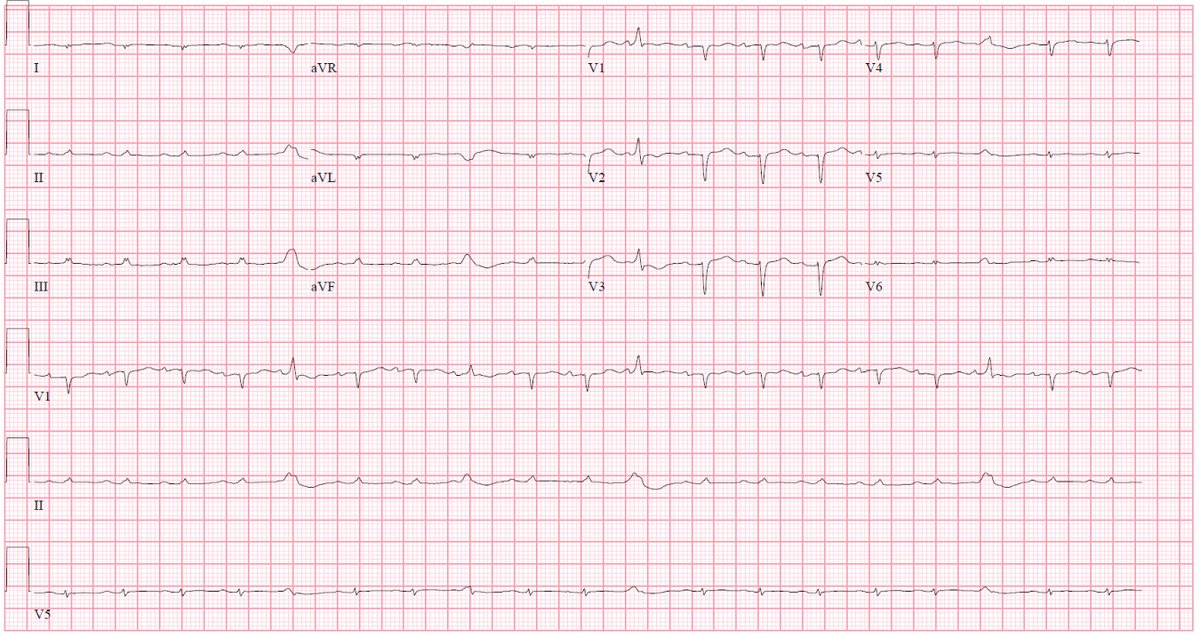
Case: 70 yo woman w/paroxysmal AFib, HTN, T2DM hasn’t seen MD in a few years admitted w/acute decompensated HF. ECG with low volts. Echo: LVEF 32%,  LV wall thickness, & severely
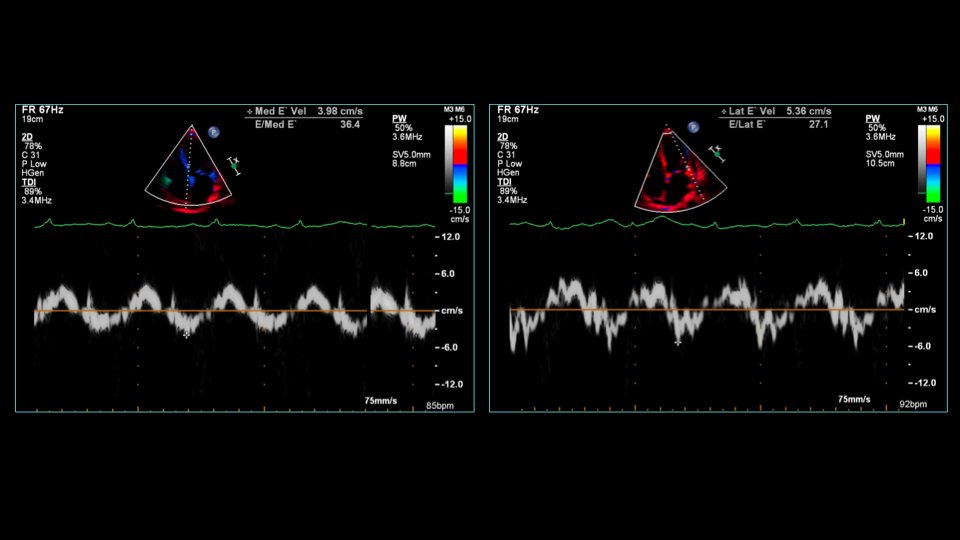
LV wall thickness, & severely  TDI velocities (s’, e’, and a’ < 5 cm/s at the septum, nearly this low at lateral mitral annulus).
TDI velocities (s’, e’, and a’ < 5 cm/s at the septum, nearly this low at lateral mitral annulus).
 LV wall thickness, & severely
LV wall thickness, & severely  TDI velocities (s’, e’, and a’ < 5 cm/s at the septum, nearly this low at lateral mitral annulus).
TDI velocities (s’, e’, and a’ < 5 cm/s at the septum, nearly this low at lateral mitral annulus).
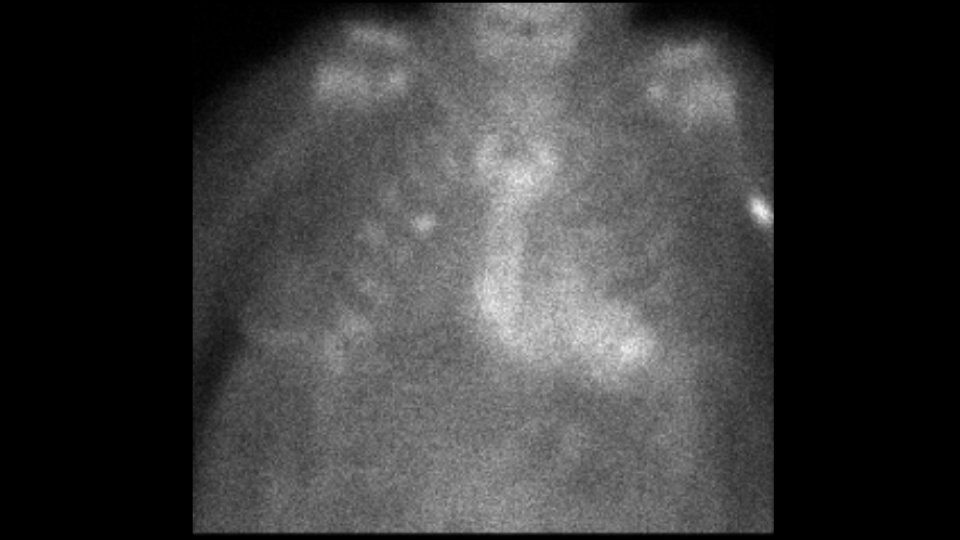
AL labs show no evidence of a plasma cell dyscrasia. PYP scan shows heart-to-contralateral lung ratio = 1.5, qualitative grade 3 uptake. Here is the planar image (myocardial uptake corroborated on SPECT):
What would you do next?
Answer: endomyocardial biopsy. Recent MI was the cause of false positive PYP scan. Given very +PYP uptake, would want to definitively rule out ATTR-CM so biopsy needed. Wall motion was tip-off to exclude MI. CMR would help but would still not answer Q about ATTR-CM definitively.
DON'T GIVE THIS PATIENT TAFAMIDIS! Need to be vigilant about potential for false positive PYP scans. Perform endomyocardial bx if any doubt. PYP is a great tool, but most published studies done in pts with  pre-test prob. As we use test more widely, will learn about best uses.
pre-test prob. As we use test more widely, will learn about best uses.
 pre-test prob. As we use test more widely, will learn about best uses.
pre-test prob. As we use test more widely, will learn about best uses.

 Read on Twitter
Read on Twitter