alright buckle up for a tweetorial on every resuscitationists' least favorite drug, epinephrine-
Very proud to share our newest publication with @lipidguy, @long_brit and best of all my colleague future Dr. Della Porta @MedEdtweeter! https://www.sciencedirect.com/science/article/pii/S0735675720309268?utm_campaign=STMJ_AUTH_SERV_PUBLISHED&utm_medium=email&utm_acid=11828904&SIS_ID=&dgcid=STMJ_AUTH_SERV_PUBLISHED&CMX_ID=&utm_in=DM106360&utm_source=AC_
Very proud to share our newest publication with @lipidguy, @long_brit and best of all my colleague future Dr. Della Porta @MedEdtweeter! https://www.sciencedirect.com/science/article/pii/S0735675720309268?utm_campaign=STMJ_AUTH_SERV_PUBLISHED&utm_medium=email&utm_acid=11828904&SIS_ID=&dgcid=STMJ_AUTH_SERV_PUBLISHED&CMX_ID=&utm_in=DM106360&utm_source=AC_
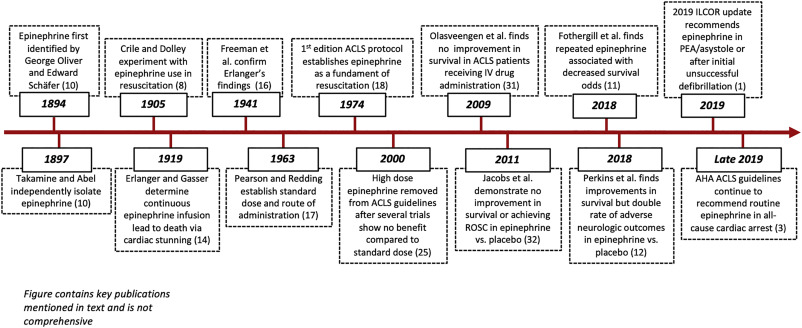
Ok, y'all know epinephrine. Here's the backstory. It was the late 19th century & scientists were still grinding up and tincturing organs to see what effects they had on a whole organism. Epinephrine was independently sourced from the adrenal glands in Europe, the US and Japan.
Oliver & Schafer, two British doctors, remarked upon epinephrine injection while using a newly developed manometer:"like some watcher of the skies, when a new planet swims into his ken" they watched the mercury rise in the manometer with amazing rapidity and to astounding height.
What they identified was the potent vasoconstrictive property of epinephrine, which would go on to set the stage for the development of hemodynamic research & the field of resuscitation science.
Prior to this, resuscitative efforts were laughable:
Prior to this, resuscitative efforts were laughable:
"Blowing smoke up your ass" refers literally to the 18th-century practice of rectal tobacco insufflation via bellows in the heroic effort to reanimate a corpse. Turn of the century materia medica was on the cusp of scientific pharmacology but often killing patients with ether.
1905: Along come Crile & Dolley, who subjected dogs to chloroform, ether, + asphyxial arrest, performing cardiac massage with IV/arterial/intracardiac epi.
Crile and Dolley report that resuscitation efforts among dogs receiving 1–2 mg of epinephrine alongside “cardiac massage, artificial respiration, and intravenous saline infusion… were in a slightly greater proportion successful.”
If this sounds familiar, it's because it's ACLS.
If this sounds familiar, it's because it's ACLS.
Their experiments are repeated dozens of times until formalized in the first edition of Advanced Cardiac Life Support and every edition following.
However, one piece was missing from this.
However, one piece was missing from this.
Crile and Dolley noted that in “[resuscitations] in which a considerable [amount] was given… and in those after fifteen to twenty minutes; while circulation and respiration were satisfactory, the animal did not regain consciousness.”
This finding would prove prescient as current evidence indicates epi improves rates of ROSC after cardiac arrest but no improvement in neurologic or long-term outcomes.
Perkins (2018) found that while epi resulted in significantly greater 30-day survival vs placebo, no significant difference existed between groups re: favorable neuro outcomes. ~Twice the rate of severe neuro impairment was seen among survivors in the epi group vs controls.
Why is this?
Hypothetically, it gets back to Oliver & Schafer. Pressure climbs in the vasculature via vasoconstriction. Following reperfusion, coagulation cascade activation induces microthrombus formation, impairing cerebral microvascular perfusion, further compromised by epi α1 agonism
That's not all. Weil and others identified severe, adverse effects of epinephrine on neurologic function in animal cardiac arrest models resulting from impaired post-resuscitation microcirculatory perfusion, cortical tissue oxygen tension, and increased inflammatory milieu.
So what works? CPR, clearly.
But why targeted temperature management?
But why targeted temperature management?
Improved neurological function from post-resuscitation hypothermia may derive from inhibition of inflammatory mediator production (ROS, NF-κB, TNF-α, matrix metalloproteinases, and neuron-specific enolase, which contribute to reperfusion injury and intracranial edema.
Post-ROSC epi levels are strongly associated with markers of vascular endothelial injury & inflammation. These increase following resuscitation as a result of reperfusion itself; however, in-vitro, translational & clinical evidence demonstrate epi magnifies reperfusion injury.
The best evidence suggest epi is only truly useful in improving outcomes in PEA and asystole arrest, with worse all-comer neurologic outcomes. Increasing doses lead to diminishing returns.

 Read on Twitter
Read on Twitter