New publication alert!
New publication alert!

Delighted to share this paper describing our team's love & sweat over the past few years
Our hospital didn’t have an addiction medicine consultation service, so us trainees started one!

https://www.tandfonline.com/doi/full/10.1080/08897077.2020.1856291
( #OpenAccess & thread!
 ) /1
) /1
A lot of patients are admitted to hospital for medical complications of substance use disorders
For example, as @IDDoc1978 & co. showed, hospital admissions for injection drug use-related endocarditis (a life-threatening heart infection) are rising /2
https://academic.oup.com/ofid/article/3/3/ofw157/2593299
For example, as @IDDoc1978 & co. showed, hospital admissions for injection drug use-related endocarditis (a life-threatening heart infection) are rising /2
https://academic.oup.com/ofid/article/3/3/ofw157/2593299
And as @DrSarahWakeman & team found, nearly 1 in 6 hospital patients screen positive for high-risk substance use:
https://www.tandfonline.com/doi/full/10.1080/08897077.2019.1635961
In fact, in we have more hospital admissions for alcohol-related problems than we do for heart attacks! /3 https://www.theglobeandmail.com/canada/article-more-canadians-hospitalized-per-day-for-health-conditions-and-injuries/
we have more hospital admissions for alcohol-related problems than we do for heart attacks! /3 https://www.theglobeandmail.com/canada/article-more-canadians-hospitalized-per-day-for-health-conditions-and-injuries/
https://www.tandfonline.com/doi/full/10.1080/08897077.2019.1635961
In fact, in
 we have more hospital admissions for alcohol-related problems than we do for heart attacks! /3 https://www.theglobeandmail.com/canada/article-more-canadians-hospitalized-per-day-for-health-conditions-and-injuries/
we have more hospital admissions for alcohol-related problems than we do for heart attacks! /3 https://www.theglobeandmail.com/canada/article-more-canadians-hospitalized-per-day-for-health-conditions-and-injuries/
Sow while all hospital-based clinicians treat medical complications of addictions every day, that doesn't mean we're necessarily comfortable providing hospital inpatients with evidence-based care for their underlying addiction. 4/ https://www.tandfonline.com/doi/full/10.1080/08897077.2016.1187240?src=recsys
E.g., @serotavirus & @DrMelissaWeimer explain how its normal for hospital clinicians to focus on complicated antibiotics & surgeries for patients w/ endocarditis, without ever offering opioid agonist treatment for their underlying opioid use disorder. 5/ https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2626861
& here @honoraenglander & team capture the "moral distress" that some hospital providers feel when they don't know how to help patients with substance use disorders. /6 https://www.journalofhospitalmedicine.com/jhospmed/article/163562/hospital-medicine/weve-learned-its-medical-illness-not-moral-choice?utm_source=News%5FJHM%5FeNL%5F042518%5FF&utm_medium=email&utm_content=Medical%20Illness%20vs%20Moral%20Choice%20%7C%20Text%20Message%20Interruptions%20%7C%20Transport%20Medicine
(As an aside, reasons why mainstream medicine has not considered addiction care part of its job are long+complicated, influenced by stigma & criminalization of people who use drugs - but it's important to know that we now have evidence-based treatments to offer!) /7
Beyond offering addiction treatments, aggressively treating opioid withdrawal & pain can help patients w/ opioid use disorder stay in hospital & get needed antibiotics/surgeries
Check out this great @CrismCan guideline (authors tagged in pic):
https://crismprairies.ca/management-of-substance-use-in-acute-care-settings-in-alberta-guidance-document/
/8
Check out this great @CrismCan guideline (authors tagged in pic):
https://crismprairies.ca/management-of-substance-use-in-acute-care-settings-in-alberta-guidance-document/
/8
Addiction medicine consultation services (AMCS) can add a lot of value in helping hospital patients understand treatment options & start treatment in hospital if they want
& also in supporting the whole hospital to improve care
https://www.medical.theclinics.com/article/S0025-7125(18)30020-8/pdf /9
@ZoeWeinstein
& also in supporting the whole hospital to improve care
https://www.medical.theclinics.com/article/S0025-7125(18)30020-8/pdf /9
@ZoeWeinstein
For example, AMCS can team up with infectious disease specialists, cardiologists, and cardiac surgeons to provide the best patient-centred, multidisciplinary plan of care for patients with injection drug use-associated infective endocarditis. /10 https://openheart.bmj.com/content/4/2/e000699.responses#multidisciplinary-infective-endocarditis-care-teams-should-address-substance-use-disorders-and-harm-reduction-services
Which finally brings us to our paper!
Our hospital in Nova Scotia, Canada, has not had an addiction medicine consultation service, even though we're the academic, tertiary care referral centre for the whole province. /11 https://www.tandfonline.com/doi/full/10.1080/08897077.2020.1856291?scroll=top&needAccess=true
Our hospital in Nova Scotia, Canada, has not had an addiction medicine consultation service, even though we're the academic, tertiary care referral centre for the whole province. /11 https://www.tandfonline.com/doi/full/10.1080/08897077.2020.1856291?scroll=top&needAccess=true
& when I was a medical student, I participated in some really bad care - we forced patients into withdrawal and made them leave hospital only to come back even sicker. We did not make them feel welcome or loved.
I know we weren't the only ones:
https://www.sciencedirect.com/science/article/pii/S0277953614000355?via%3Dihub /12
I know we weren't the only ones:
https://www.sciencedirect.com/science/article/pii/S0277953614000355?via%3Dihub /12
The care team was made up of health professionals who really wanted to do a good job, including many people I still consider mentors!
I just think we didn't know how to help, and we were influenced by widespread stigma towards people who use drugs.
https://harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-019-0285-7 /13
I just think we didn't know how to help, and we were influenced by widespread stigma towards people who use drugs.
https://harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-019-0285-7 /13
It was also system-level factors; e.g., there was no doctor across the whole hospital who knew how to prescribe methadone or buprenorphine to start people on treatment for opioid use disorders
And we weren't learning this stuff in the classroom!
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0229713 /14
And we weren't learning this stuff in the classroom!
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0229713 /14
So a few of us started seeking out learning opportunities (from @AMentorship @CAMHnews & others) and talking to experts in the community outside the hospital about how we could change things ( @needleexchange2 @MOSHHalifax @Direction180). /15
Dr John Fraser, a community-based addiction & family physician at @NorthEndCHC invited me to do a clinical elective with him, and we spread the word that we were open for business!
https://www.tandfonline.com/doi/pdf/10.1080/08897077.2020.1856291?needAccess=true
https://www.tandfonline.com/doi/pdf/10.1080/08897077.2020.1856291?needAccess=true
We started a model where a hospital-based resident (initially just me) would see the patient and review with a community-based addiction physician (initially just him) over the phone, then once per week the community physician would round in person. 17/
After the elective ended, John and I kept it going in our "spare" time.
Obviously a 2-person program is not sustainable or healthy, and I can't ever overstate the contributions of @ejmacadam when she joined the team as the second resident, just when I might have burned out /18
Obviously a 2-person program is not sustainable or healthy, and I can't ever overstate the contributions of @ejmacadam when she joined the team as the second resident, just when I might have burned out /18
The team grew to include hospital-based residents in internal medicine, anesthesia, and psychiatry who wanted to learn more addiction medicine & were passionate about improving hospital care for our patients with substance use disorders @AdiNidumolu @CapnBMo @JFrancheville /19
& also more community-based addiction & primary care physicians who were willing to volunteer their time to supervise us, because their patients with substance use disorders were being admitted to hospital (I don't think any are on Twitter, but they're all co-authors 
 ) /20
) /20

 ) /20
) /20
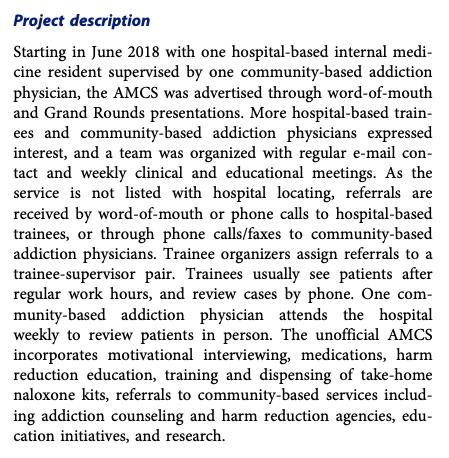
Though we were never listed w/ hospital locating (& never actually had anyone "on call", or doing this for a day job), over the first 16 months we had 59 referrals for 50 different patients/admissions.
95% were for patients who inject drugs /21 https://www.tandfonline.com/doi/full/10.1080/08897077.2020.1856291?scroll=top&needAccess=true
95% were for patients who inject drugs /21 https://www.tandfonline.com/doi/full/10.1080/08897077.2020.1856291?scroll=top&needAccess=true
("Why pick 16 months for an evaluation period?" you may ask - that's when I had to take a little/long break for @Royal_College studying, and at that point the other residents tagged above took the lead 


 ) /22
) /22



 ) /22
) /22
Of the 59 referrals, trainees were able to see 53 (90%) before the patient left hospital or was discharged...
And 52/53 (98%!!!) wanted to go ahead & chat about their substance use + potential treatment options. /23 https://www.tandfonline.com/doi/full/10.1080/08897077.2020.1856291?scroll=top&needAccess=true
And 52/53 (98%!!!) wanted to go ahead & chat about their substance use + potential treatment options. /23 https://www.tandfonline.com/doi/full/10.1080/08897077.2020.1856291?scroll=top&needAccess=true
Of course not every patient admitted to hospital w/ a medical illness caused by a substance use disorder (like endocarditis) was seeking addiction treatment when they woke up that morning, but turns out many folks are interested in discussing options! /24 https://www.journalofhospitalmedicine.com/jhospmed/article/136504/hospital-medicine/planning-and-designing-improving-addiction-care-team
We looked at how many patients w/ untreated moderate or severe opioid use disorder might be interested in starting methadone or buprenorphine treatment in-hospital; it turns out that most went ahead, started, and continued after hospital discharge /25
https://www.tandfonline.com/doi/full/10.1080/08897077.2020.1856291?scroll=top&needAccess=true
https://www.tandfonline.com/doi/full/10.1080/08897077.2020.1856291?scroll=top&needAccess=true
We were glad to be able to offer patients these opioid agonist treatments while in-hospital & link them into outpatient care after discharge
This is an evidence-based practice, and all patients in Nova Scotia deserve evidence-based treatment! /26 https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/1885989
This is an evidence-based practice, and all patients in Nova Scotia deserve evidence-based treatment! /26 https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/1885989
& while the evaluation period in this paper stopped in Sept 2019, we're still going strong with an even bigger team and weekly meetings over Zoom 
 /27
/27

 /27
/27
We discuss in the paper some factors that might have helped our service succeed:
1) We used existing resources, including take-home
naloxone kits provided free by @HealthNS
(Check out http://www.nsnaloxone.com/ ). /28
1) We used existing resources, including take-home
naloxone kits provided free by @HealthNS
(Check out http://www.nsnaloxone.com/ ). /28
2) We learned from the best, including @needleexchange2 who were already providing outreach ("in-reach"?) to their clients/participants in hospital long before we came along
3) I cannot overstate what incredible champions our hospital pharmacists have been, across all units /29
3) I cannot overstate what incredible champions our hospital pharmacists have been, across all units /29
We still have some challenges
We're “unofficial” - we're not formally recognized or resourced, and we don't have a call schedule or listing with hospital locating
(Thanks Dr. Fraser for providing - along w/ incredible teaching & supervision - the use of your fax machine!) /30
We're “unofficial” - we're not formally recognized or resourced, and we don't have a call schedule or listing with hospital locating
(Thanks Dr. Fraser for providing - along w/ incredible teaching & supervision - the use of your fax machine!) /30
We also introduced multiple new practices that are still catching on (but really do seem to be!) - aggressive treatment of opioid withdrawal with opioids, in-hospital methadone & buprenorphine starts, take-home naloxone kits, and in-hospital referrals to @needleexchange2 /31
We've been invited to give talks/workshops on different units with nursing colleagues, and at hospitals around the province -- most people ask, "why haven't we always been doing things this way?" /32 https://www.tandfonline.com/doi/full/10.1080/08897077.2020.1856291?scroll=top&needAccess=true
& I'm happy to say that @NSHealthMHA has expressed interest in working with us to get a formal AMCS organized & funded 

This would hugely increase capacity & learning opportunities, make the team available during day-time hours (rather than evening/weekends) /33


This would hugely increase capacity & learning opportunities, make the team available during day-time hours (rather than evening/weekends) /33
While trying to figure out what was possible & throughout this process, I had the most incredible role models & teachers who changed my life forever (including John) /34
These include Patti Melanson, RN, founder of
@MOSHHalifax and recipient of the Order of Nova Scotia
She showed us how to fight for people we care about https://www.thechronicleherald.ca/news/local/halifax-nurse-patti-melanson-was-a-champion-of-the-vulnerable-268977/
https://www.thechronicleherald.ca/news/local/halifax-nurse-patti-melanson-was-a-champion-of-the-vulnerable-268977/
@MOSHHalifax and recipient of the Order of Nova Scotia
She showed us how to fight for people we care about
 https://www.thechronicleherald.ca/news/local/halifax-nurse-patti-melanson-was-a-champion-of-the-vulnerable-268977/
https://www.thechronicleherald.ca/news/local/halifax-nurse-patti-melanson-was-a-champion-of-the-vulnerable-268977/
And Natasha Pace, a member of the Halifax Area Network of Drug Using People (HANDUP)
Over our many conversations, she was incredibly generous with her ideas about how to provide better health care for people who use drugs /35 https://www.thechronicleherald.ca/obituaries/natasha-lynn-pace-26731/
Over our many conversations, she was incredibly generous with her ideas about how to provide better health care for people who use drugs /35 https://www.thechronicleherald.ca/obituaries/natasha-lynn-pace-26731/
I'm glad that we could acknowledge their contributions in a small way - I carry their lessons with me every day
https://www.tandfonline.com/doi/full/10.1080/08897077.2020.1856291?scroll=top&needAccess=true /36
https://www.tandfonline.com/doi/full/10.1080/08897077.2020.1856291?scroll=top&needAccess=true /36

 Read on Twitter
Read on Twitter