1/ #IDtwitter ! shameless plug to check out our recently published study
We examined the effectiveness of adjunctive clindamycin in β-lactam treated pts with invasive group A streptococcal (GAS) and invasive non-group A/B streptococcal (NABS) infections https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30523-5/fulltext?rss=yes
We examined the effectiveness of adjunctive clindamycin in β-lactam treated pts with invasive group A streptococcal (GAS) and invasive non-group A/B streptococcal (NABS) infections https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30523-5/fulltext?rss=yes
2/ I know everyone is super busy, and consumed by all things COVID so I'll briefly walk y'all through some of the highlights paper in this thread 

3/ As way of background, check out this prior tweetorial where I delved into some of the rationale and in vitro evidence behind clindamycin use in GAS (don't miss the pic at the end of the thread!)
There is v little data on NABS (just one clinical study) https://twitter.com/Ahmed_HBabiker/status/1173987194937253888?s=20
There is v little data on NABS (just one clinical study) https://twitter.com/Ahmed_HBabiker/status/1173987194937253888?s=20
4/ We used an EMR dataset which contains de-identified electronic health record-based data from 233 US hospitals
The final cohort contained 1956 patients with mono-microbial invasive hemolytic strep (GAS and NABS) admitted to 118 hospitals over a 15-year period (2000-2015)
The final cohort contained 1956 patients with mono-microbial invasive hemolytic strep (GAS and NABS) admitted to 118 hospitals over a 15-year period (2000-2015)
5/ Inclusion criteria?
- Positive sterile site culture (eg. blood) for GAS or NABS
Positive sterile site culture (eg. blood) for GAS or NABS
= proven disease
OR
- Positive non sterile site culture (eg. sputum) + compatible ICD-9 code (eg for pneumonia) = probable disease
Positive non sterile site culture (eg. sputum) + compatible ICD-9 code (eg for pneumonia) = probable disease
AND
 And B-lactam therapy within 3 days of culture
And B-lactam therapy within 3 days of culture
-
 Positive sterile site culture (eg. blood) for GAS or NABS
Positive sterile site culture (eg. blood) for GAS or NABS = proven disease
OR
-
 Positive non sterile site culture (eg. sputum) + compatible ICD-9 code (eg for pneumonia) = probable disease
Positive non sterile site culture (eg. sputum) + compatible ICD-9 code (eg for pneumonia) = probable diseaseAND
 And B-lactam therapy within 3 days of culture
And B-lactam therapy within 3 days of culture
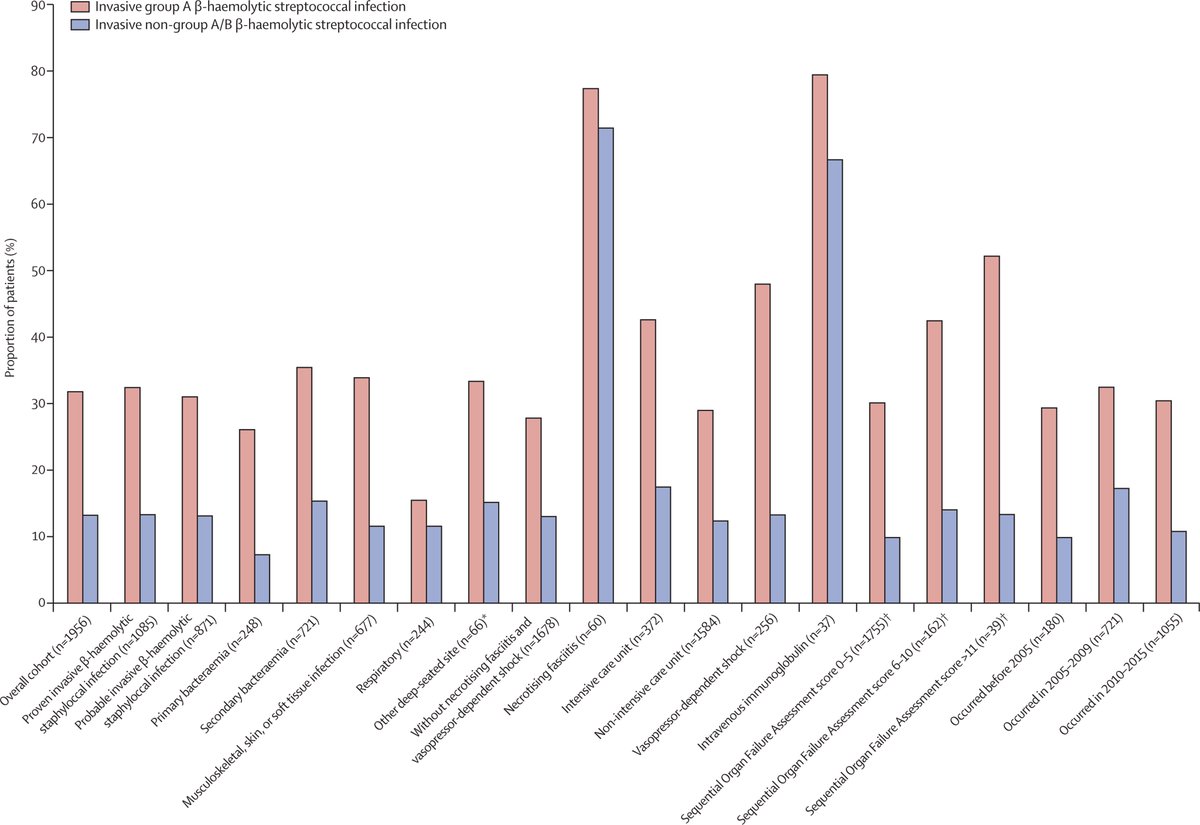
6/ Because pts who receive clindamycin are generally younger but sicker, than those who don't (more pressors, more ICU stay, more NF) we propensity matched clindamycin and non-clindamycin pts
To make sure we compared apples to apples GAS and NABS groups were analyzed separately
To make sure we compared apples to apples GAS and NABS groups were analyzed separately
7/ Our primary outcome of interest was adjusted odds ratio (aOR) of in-hospital mortality, including discharge to hospice
On top of propensity matching we also did down stream adjustment for proven invasive disease status, vasopressor use, and ICU status.
On top of propensity matching we also did down stream adjustment for proven invasive disease status, vasopressor use, and ICU status.
8/ So what did we find ?
Firstly we found clindamycin use varied by lancefield group type (GAS vs. NABS) and clinical syndrome
There was low use overall, especially in those that did not have shock, or NF.
Firstly we found clindamycin use varied by lancefield group type (GAS vs. NABS) and clinical syndrome
There was low use overall, especially in those that did not have shock, or NF.
9/What about mortality ?
In the propensity-matched GAS cohort (n=777) we found that adjunctive clindamycin decreased in-hosp mortality for GAS ! (aOR 0·44 [95% CI 0·23–0·81])
This was also seen among the various subgroups we examined
In the propensity-matched GAS cohort (n=777) we found that adjunctive clindamycin decreased in-hosp mortality for GAS ! (aOR 0·44 [95% CI 0·23–0·81])
This was also seen among the various subgroups we examined
10/We saw a different story w/ NABS
In the propensity-matched NABS cohort (n=295), mortality was numerically higher in the clindamycin pts.
So no benefit ! and this trended towards harm (aOR 2·60 [95% CI 0·94–7·52]
This was also seen among the various subgroups we examined
In the propensity-matched NABS cohort (n=295), mortality was numerically higher in the clindamycin pts.
So no benefit ! and this trended towards harm (aOR 2·60 [95% CI 0·94–7·52]
This was also seen among the various subgroups we examined
11/ To conclude I'll leave yall with this succinct summary tweet by the senior author @SameerKadri12 https://twitter.com/SameerKadri12/status/1338868986201698305?s=20
12/ What about Group B strep you say ?
We found very little use of adjunctive clindamycin among these patients.
Only 7% which is probably good due to high rates of clindamycin resistance among GBS.
Link to CDC AMR 2019 report https://www.cdc.gov/drugresistance/pdf/threats-report/gbs-508.pdf
We found very little use of adjunctive clindamycin among these patients.
Only 7% which is probably good due to high rates of clindamycin resistance among GBS.
Link to CDC AMR 2019 report https://www.cdc.gov/drugresistance/pdf/threats-report/gbs-508.pdf
13/ Some remaining unanswered questions in my mind:
-Linezolid? We excluded these pts and hope to delve into this in the future
-We cannot extrapolate this data to NF, as the rates of NF were low in our propensity matched cohort
-What was mechanism behind the NABS findings
-Linezolid? We excluded these pts and hope to delve into this in the future
-We cannot extrapolate this data to NF, as the rates of NF were low in our propensity matched cohort
-What was mechanism behind the NABS findings
14/ Big thanks to all involved in the study especially @SameerKadri12 for roping me into this back when I was clueless IM resident and twitter present and @sarahrenee314 @JeffreyStrichMD and twitterless co-authors for a lot of heavy lifting and critical input !

 Read on Twitter
Read on Twitter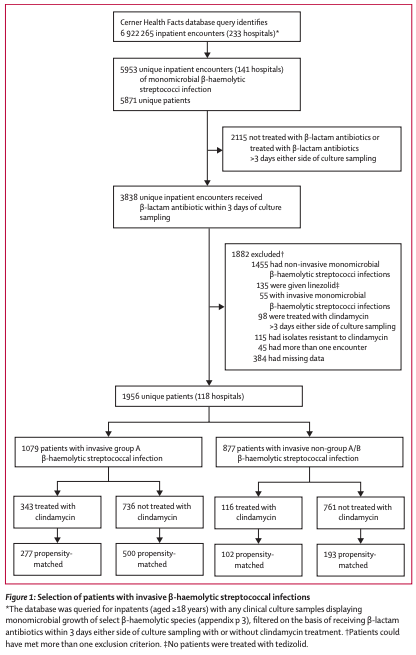
![9/What about mortality ?In the propensity-matched GAS cohort (n=777) we found that adjunctive clindamycin decreased in-hosp mortality for GAS ! (aOR 0·44 [95% CI 0·23–0·81])This was also seen among the various subgroups we examined 9/What about mortality ?In the propensity-matched GAS cohort (n=777) we found that adjunctive clindamycin decreased in-hosp mortality for GAS ! (aOR 0·44 [95% CI 0·23–0·81])This was also seen among the various subgroups we examined](https://pbs.twimg.com/media/EpZ5pbYXYAE1FWd.jpg)
![10/We saw a different story w/ NABS In the propensity-matched NABS cohort (n=295), mortality was numerically higher in the clindamycin pts.So no benefit ! and this trended towards harm (aOR 2·60 [95% CI 0·94–7·52]This was also seen among the various subgroups we examined 10/We saw a different story w/ NABS In the propensity-matched NABS cohort (n=295), mortality was numerically higher in the clindamycin pts.So no benefit ! and this trended towards harm (aOR 2·60 [95% CI 0·94–7·52]This was also seen among the various subgroups we examined](https://pbs.twimg.com/media/EpZ5hCiXEAAYD5c.jpg)


