1/
Today, a brief #dermtwitter #tweetorial on a topic particularly important during the #COVID19 #pandemic:
PRESSURE ULCERS (PU)!
#MedEd #FOAMEd #medtwitter #nursetwitter #medstudenttwitter #dermatology No COI
PC: @dermnetnz and @grepmeded
Today, a brief #dermtwitter #tweetorial on a topic particularly important during the #COVID19 #pandemic:
PRESSURE ULCERS (PU)!
#MedEd #FOAMEd #medtwitter #nursetwitter #medstudenttwitter #dermatology No COI
PC: @dermnetnz and @grepmeded
First, a disclaimer: while #dermatologists can certainly help in the management of PU, the vast majority are expertly cared for by the #nursing teams in our hospitals. So a huge  to them!
to them!
Let's chat pathophysiology: What is the main underlying mechanism in PU development?
 to them!
to them!Let's chat pathophysiology: What is the main underlying mechanism in PU development?
Ischemia is the most important contributor to PU. The interruption of blood flow leads to tissue necrosis.
PU are staged based on depth from 1 (non-blanching erythema) to 4 (bone/tendon exposed), and suspected deep tissue injury or when the PU is unstageable.
PC: @uptodate
PU are staged based on depth from 1 (non-blanching erythema) to 4 (bone/tendon exposed), and suspected deep tissue injury or when the PU is unstageable.
PC: @uptodate
4/
While we usually see PU on the lower back/buttock/heels for obvious reasons, in #COVID19 patients who are prone, we are seeing reports of PU on the face and arms. This article estimated 57% of prone patients develop a PU!
https://www.magonlinelibrary.com/doi/abs/10.12968/jowc.2020.29.6.312?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
While we usually see PU on the lower back/buttock/heels for obvious reasons, in #COVID19 patients who are prone, we are seeing reports of PU on the face and arms. This article estimated 57% of prone patients develop a PU!
https://www.magonlinelibrary.com/doi/abs/10.12968/jowc.2020.29.6.312?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
5/
In terms of treatment, the most important step is prevention. Patients should be moved at least Q2h. In our #COVID patients, where we may not be in the room as frequently to prevent HCW transmission, use of other equipment (eg: airbeds, foam dressings, etc) can be helpful!
In terms of treatment, the most important step is prevention. Patients should be moved at least Q2h. In our #COVID patients, where we may not be in the room as frequently to prevent HCW transmission, use of other equipment (eg: airbeds, foam dressings, etc) can be helpful!
6/
But once it happens, what can we do? Well, Stage 1 PU can be treated with a foam dressing (for example, an Allevyn or Mepilex border lite). It’s best to catch them early to prevent worsening. (Some suggest using these prophylactically in high risk spots before PU develops!).
But once it happens, what can we do? Well, Stage 1 PU can be treated with a foam dressing (for example, an Allevyn or Mepilex border lite). It’s best to catch them early to prevent worsening. (Some suggest using these prophylactically in high risk spots before PU develops!).
7/
If the ulcer has overlying fibrinous debris, debridement is helpful. Skin ulcers heal from the periphery in, so anything standing in the way needs to be removed. An easy way to start is to use chemical debridement first with collagenase (Santyl) or Medi-honey.
If the ulcer has overlying fibrinous debris, debridement is helpful. Skin ulcers heal from the periphery in, so anything standing in the way needs to be removed. An easy way to start is to use chemical debridement first with collagenase (Santyl) or Medi-honey.
8/
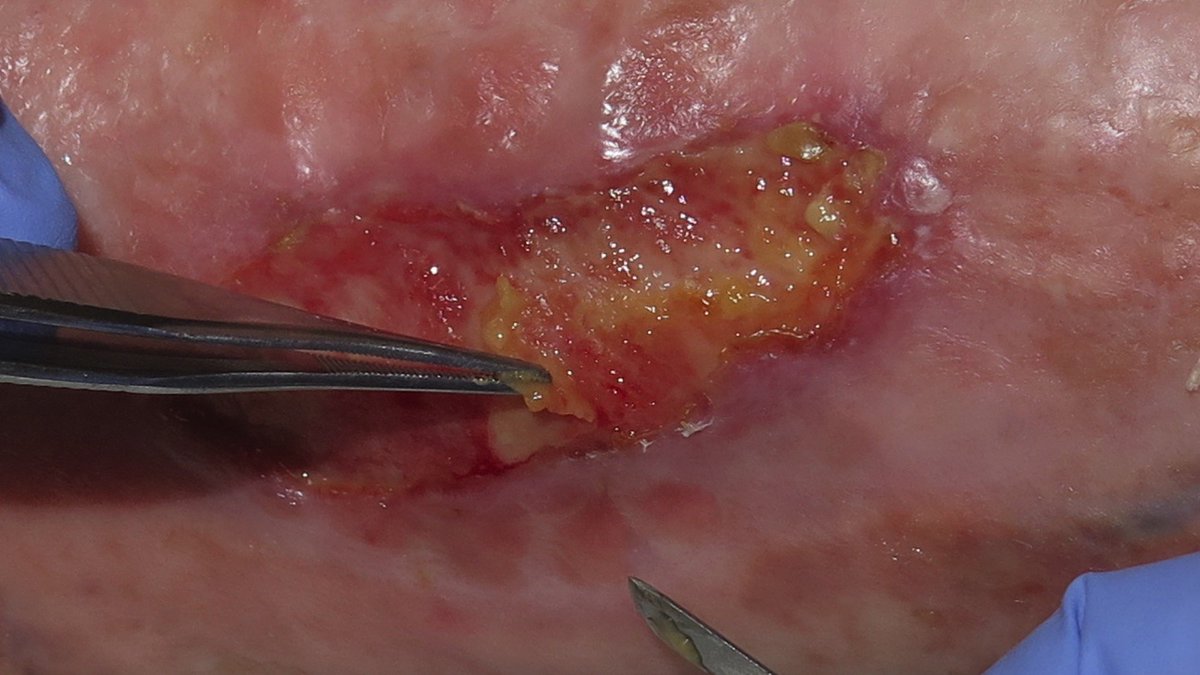
If chemical debridement doesn’t work, mechanical debridement can be done at the bedside with local anesthesia (see pic). If something more extensive is required, the OR may be required for deeper debridement with possible vac dressing or grafts.
PC: https://www.elenaconde.com/en/fibrinous-tissue-in-venous-ulcers-what-are-we-talking-about/
If chemical debridement doesn’t work, mechanical debridement can be done at the bedside with local anesthesia (see pic). If something more extensive is required, the OR may be required for deeper debridement with possible vac dressing or grafts.
PC: https://www.elenaconde.com/en/fibrinous-tissue-in-venous-ulcers-what-are-we-talking-about/
9/
A word on dressings - #dermatology and #surgery teams tend to disagree on this. We like to use non-traumatic means of dressing (Vaseline, non-stick). Surgery teams tend to like wet-to-dry dressings, which debride (ouch!) as it pulls off fibrinous debris at dressing changes.
A word on dressings - #dermatology and #surgery teams tend to disagree on this. We like to use non-traumatic means of dressing (Vaseline, non-stick). Surgery teams tend to like wet-to-dry dressings, which debride (ouch!) as it pulls off fibrinous debris at dressing changes.
10/
A couple unique scenarios:
Superinfection: topical antibiotics help clear it quickly. Topical metronidazole is good with anaerobes. Topical mupirocin is my go-to for gram positive organisms.
Granulation tissue (pic) that impedes healing: some AgNO3 sticks do the trick!
A couple unique scenarios:
Superinfection: topical antibiotics help clear it quickly. Topical metronidazole is good with anaerobes. Topical mupirocin is my go-to for gram positive organisms.
Granulation tissue (pic) that impedes healing: some AgNO3 sticks do the trick!
11/
And a quick word for all the healthcare workers with n95 induced PU on the nasal bridge. As above, a foam dressing may help it feel better BUT this can change the n95 fit, so it’s important to get re-fit tested with whatever dressings you are using!
And a quick word for all the healthcare workers with n95 induced PU on the nasal bridge. As above, a foam dressing may help it feel better BUT this can change the n95 fit, so it’s important to get re-fit tested with whatever dressings you are using!
12/
RECAP:
- Prevention of Pressure Ulcers (PU) is key - move pts q2h if able
- For stage 1, try a foam nonstick dressing
- Try chemical debridement for fibrinous debris
- Mechanical debridement if needed
- Topical antibiotics for superinfection
- Nurses are true PU experts!
RECAP:
- Prevention of Pressure Ulcers (PU) is key - move pts q2h if able
- For stage 1, try a foam nonstick dressing
- Try chemical debridement for fibrinous debris
- Mechanical debridement if needed
- Topical antibiotics for superinfection
- Nurses are true PU experts!
13/13
There are so many other nuances when it comes to PU care, but I wanted to put something brief & high yield out! Hope this helps some of you on the front lines.
Stay safe, and I definitely invite anyone else to share tips and tricks of their own! Thanks for joining!
There are so many other nuances when it comes to PU care, but I wanted to put something brief & high yield out! Hope this helps some of you on the front lines.
Stay safe, and I definitely invite anyone else to share tips and tricks of their own! Thanks for joining!

 Read on Twitter
Read on Twitter