Is #COVID19 associated to acute pancreatitis? A very simple question, but difficult to answer, let's discuss it in this Twitter thread based on the review written by @lelecapurso and me for @NatRevGastroHep
#UEGambassador @my_ueg @aegastro


 https://www.nature.com/articles/s41575-020-00389-y
https://www.nature.com/articles/s41575-020-00389-y
#UEGambassador @my_ueg @aegastro


 https://www.nature.com/articles/s41575-020-00389-y
https://www.nature.com/articles/s41575-020-00389-y
To determine the causality of a certain disease has troubled physicians for centuries. Robert Koch identified the bacteria causing of tuberculosis, cholera, and anthrax. He develop causality criteria for infectious diseases
Koch´s postulates are:
1 The microorganism (mo) is present in patients
2 The mo is isolated from a patient/animal and grow in cultures
3 The cultured mo produces disease in animals
4 Re-isolation from inoculated animals show that mo, and disease develops from that new isolation
1 The microorganism (mo) is present in patients
2 The mo is isolated from a patient/animal and grow in cultures
3 The cultured mo produces disease in animals
4 Re-isolation from inoculated animals show that mo, and disease develops from that new isolation
Those postulates can’t be applied to the relationship between #COVID19 and pancreatitis, as this is apparently a very infrequent complication. We have to look for other postulates addressing more subtle associations between exposition to an agent and disease
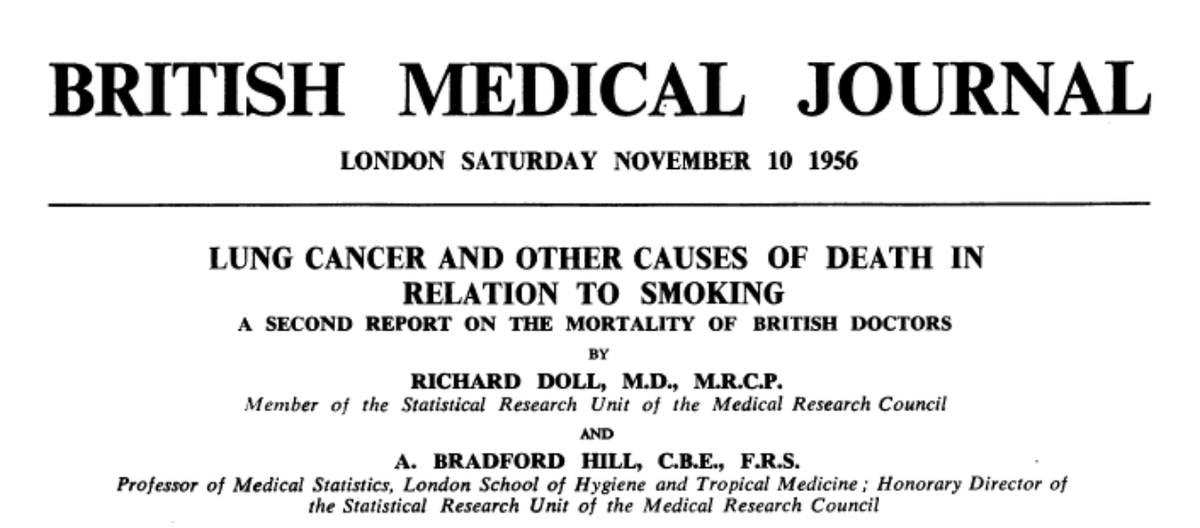
Sir Austin Bradford Hill (BH) was an English epidemiologist and statistician. R. Doll and BH demonstrated the relationship between smoking and lung cancer, for that purpose they followed British physicians for several years, an epic study in the history of medicine @bmj_latest
BH also developed his causality criteria, less simplistic than Koch's ones, less deterministic, more adapted to the multi-causality reality of disease (not all smokers develop lung cancer but it is a risk factor!)
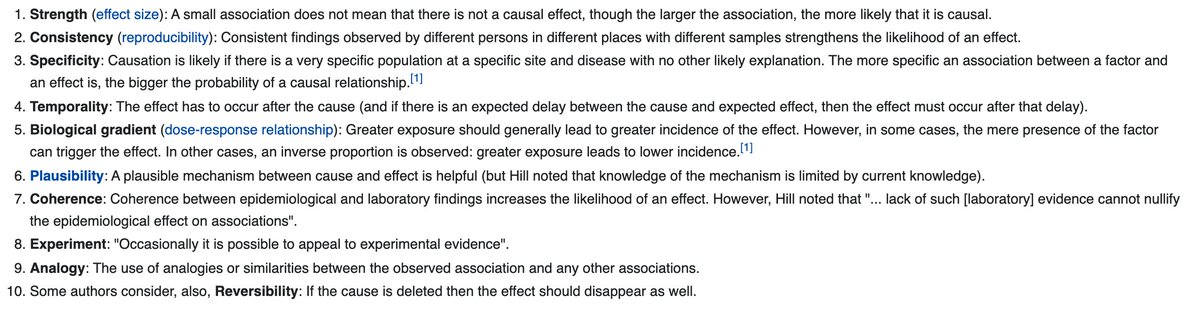
Let's review all the BH criteria applied to #COVID19- pancreatitis
Let's review all the BH criteria applied to #COVID19- pancreatitis
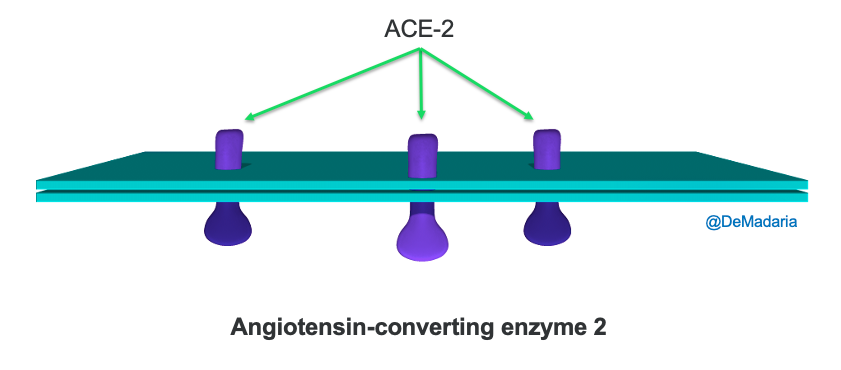
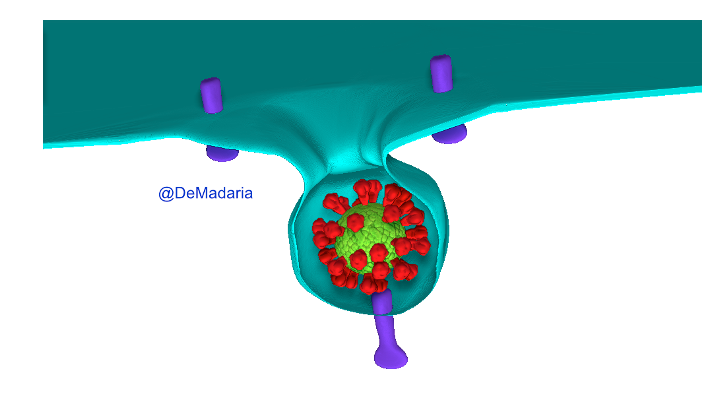
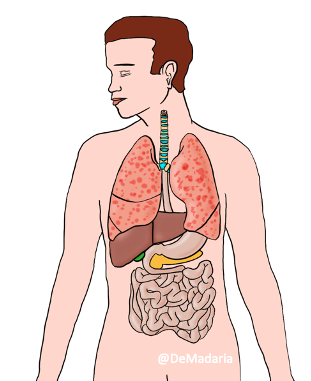
SARS-CoV-2 enters human cells by interacting with the ACE2 receptor.
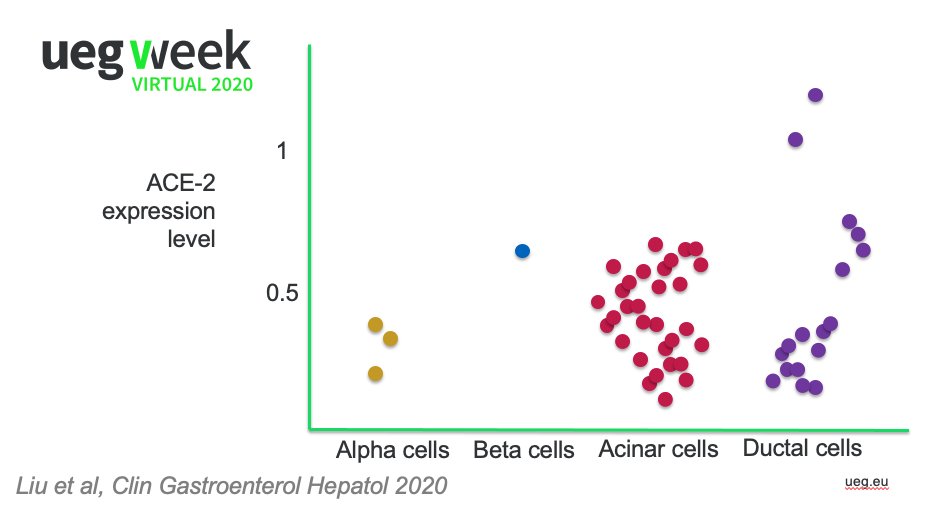
Well, ACE2 is present in the GI epithelium, in the pancreatic ductal and acinar cells, so BH PLAUSABILITY criteria
@AGA_Gastro https://www.gastrojournal.org/article/S0016-5085(20)30282-1/fulltext?referrer=https%3A%2F%2Fwww.nature.com%2F
@AGA_CGH https://www.cghjournal.org/article/S1542-3565(20)30537-1/fulltext
Well, ACE2 is present in the GI epithelium, in the pancreatic ductal and acinar cells, so BH PLAUSABILITY criteria

@AGA_Gastro https://www.gastrojournal.org/article/S0016-5085(20)30282-1/fulltext?referrer=https%3A%2F%2Fwww.nature.com%2F
@AGA_CGH https://www.cghjournal.org/article/S1542-3565(20)30537-1/fulltext
Furthermore, SARS-CoV2 RNA has been detected in a pancreatic pseudocyst sample https://doi.org/10.1016/j.pan.2020.05.016
SARS-CoV-2 could theoretically induce pancreatitis by an indirect mechanism by causing diffuse severe endotheliitis of the pancreatic microvasculature. In fact ischemia is one of the etiologies of pancreatitis
Other viruses have been associated to acute pancreatitis but SARS-CoV-1 was not, so BH COHERENCE 

Pancreatitis seems to be infrequent in COVID-19. A retrospective cohort study reported a point prevalence of 0.27% @AGA_Gastro https://doi.org/10.1053/j.gastro.2020.08.044
In 63,000 patients with #COVID19 in the ER, only 0.07% had pancreatitis @LlorensPere https://www.cambridge.org/core/journals/epidemiology-and-infection/article/frequency-of-five-unusual-presentations-in-patients-with-covid19-results-of-the-umc19s1/AA5F3253FDE6C1E2AF9D1AE5667C756F
So BH STRENGTH
In 63,000 patients with #COVID19 in the ER, only 0.07% had pancreatitis @LlorensPere https://www.cambridge.org/core/journals/epidemiology-and-infection/article/frequency-of-five-unusual-presentations-in-patients-with-covid19-results-of-the-umc19s1/AA5F3253FDE6C1E2AF9D1AE5667C756F
So BH STRENGTH

We have reports of #COVID19 + acute pancreatitis from different countries and regions, but the definition of acute pancreatitis differed between studies and some of them were not adequate @drkeithsiau @KarinaCrdenasJ1 @AGA_Gastro https://doi.org/10.1053/j.gastro.2020.04.044
so BH CONSISTENCY

so BH CONSISTENCY


There are reports suggesting that the proportion of patients with idiopathic acute pancreatitis + #COVID19 is higher than among patients with pancreatitis without #COVID19 @AGA_Gastro https://doi.org/10.1053/j.gastro.2020.08.044
...but...
...but...
...we hypothesized that patients with idiopathic pancreatitis + COVID19 undergo less frequently tests like endoscopic ultrasound and MRI due to the possibility of infection of the staff and due to the presence of pneumonia and respiratory symptoms https://www.nature.com/articles/s41575-020-00389-y
So BH SPECIFICITY 



According to case reports some cases of #COVID19-associated acute pancreatitis had the pancreatitis at the onset of COVID-19 disease, others had pancreatitis days after the onset of respiratory symptoms/fever, so BH TEMPORALITY 

Pancreatitis is not more frequent in patients with higher viral load, at least this is suggested by the fact that many patients had pancreatitis in mild #COVID19 disease, so BH BIOLOGICAL GRADIENT 

Finally we have no animal models of #COVID19 suggesting that acute pancreatitis is actually a complication of #COVID19 so BH EXPERIMENTAL EVIDENCE 

Finally in our prospective cohort study #TIVURON, we detected no case of pancreatitis among >800 patients!
Waiting for new studies to look at the real relationship between #COVID19 and pancreatitis! @COVID_PAN @NEndoscopy @sanjay_HPB @manuknayar @JohnAGMoir
Waiting for new studies to look at the real relationship between #COVID19 and pancreatitis! @COVID_PAN @NEndoscopy @sanjay_HPB @manuknayar @JohnAGMoir
@KM_Pawlak @drdalbir @BilalMohammadMD @KralJan @drkeithsiau @MZorniak @DCharabaty @RashidLui @SunilAminMD @SanchezLunaMD @stevenbollipo @Samir_Grover @RishadJkhan @drmoutaz @RodriguezParra_

 Read on Twitter
Read on Twitter