Big news on surprise billing .
There's a bicameral agreement on addressing surprise billing.
Overall, this isn't what I would have done, but arbitration linked to in-network payments isn't crazy.
A thread with a summary + initial thoughts: 1/n
https://energycommerce.house.gov/sites/democrats.energycommerce.house.gov/files/documents/No%20Surprise%20Act%20Section-by-Section%2012-11-20.pdf https://twitter.com/FrankPallone/status/1337560369678708736
There's a bicameral agreement on addressing surprise billing.
Overall, this isn't what I would have done, but arbitration linked to in-network payments isn't crazy.
A thread with a summary + initial thoughts: 1/n
https://energycommerce.house.gov/sites/democrats.energycommerce.house.gov/files/documents/No%20Surprise%20Act%20Section-by-Section%2012-11-20.pdf https://twitter.com/FrankPallone/status/1337560369678708736
The bipartisan proposal includes a hold harmless provision that requires patients, if treated by an out-of-network doctor at an in-network facility, only be subject to in-network cost-sharing & no balance billing (eg MDs/staffing companies can't go after them for charges). 2/n
Providers & insurers have a 30-day window to negotiate over out-of-network bills. If they fail to reach an agreement, bills go to baseball rules arbitration: one bid from payers, one bid from MDs. Program is administered by independent entity without MD/insurer affiliation. 3/n
In theory, baseball rules arbitration can generate an equilibrium outcome that approximates an in-network payment. In this case, the arbitration body must consider in-network rates. This is in stark contrast to what occurred in New York, where arbitrators consider charges. 4/n.
. @ProfFionasm @NathanShekita and I have an article in the Journal of Political Economy that analyzes which docs bill out-of-network (EmCare physicians primarily) and we study what occurred after NY introduced baseball rules arbitration. 5/n https://www.journals.uchicago.edu/doi/abs/10.1086/708819
As anyone who has studied this issue knows, there's intense lobbying on both sides. Here's what our paper actually shows (with our event studies). The NY law reduced the incidence of out-of-network billing by 12.8 percentage points (88%). 6/n
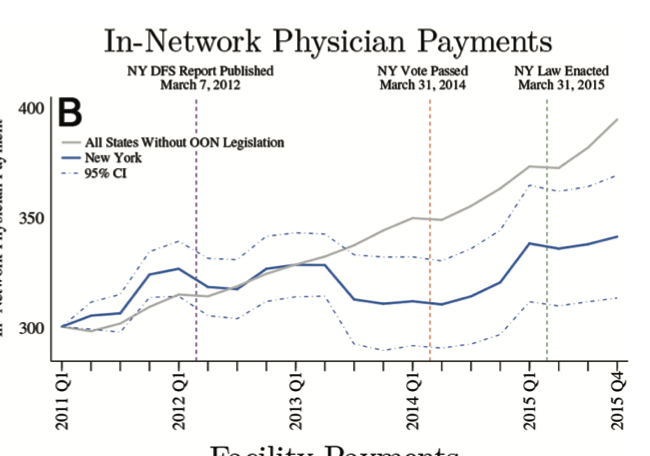
Theory suggests that arbitration weakens providers outside option and therefore should lower in-network payments. We find that the NY law lowered in-network payments by 15 percent. The change happened BEFORE the law was passed but after work on it began. 7/n
Our guess for why prices went down pre the passage of the law: out-of-network providers in NY knew the writing was on the wall. Some likely left and the intro of arbitration gave insurers more bargaining leverage. 8/n
Strengths of the proposal
- It stops balance billing. This is a big deal.
- Arbitration is linked to in-network payments. This is better than NY
- The proposal includes air ambulances
9/n
- It stops balance billing. This is a big deal.
- Arbitration is linked to in-network payments. This is better than NY
- The proposal includes air ambulances
9/n
In an ideal world, I would not have introduced arbitration. I would have forced hospitals to sell a bundle of services that included physician and facility services. Alternatively, there could be rapid payment of in-network rates with arbitration as a backstop. 10/n
My concern with arbitration is that it's clunky: the last thing the US health system needs is more administrative cost. Arbitration is also subject to regulatory capture. It looks like the drafters of this leg are aware of that, but hard to stop it in practice. 11/n
The other concern I have is constant arbitration. I have some concerns that really nasty providers will just send everything to arbitration. While I think this is unlikely, there should be a mechanism to stop providers who are taking advantage of the system. 12/n
Overall, I'd sleep better if this law passed. It would mean fewer families getting crushed. This isn't a miracle balm, but my guess is that, in the long run, this would likely lower health spending. 13/n

 Read on Twitter
Read on Twitter