Why are kidney stones so interesting?
Why are kidney stones so interesting? Because the
 tubules > glomeruli
tubules > glomeruliDisagree if you like, but it’s true.
A short thread on some mechanisms associated with calcium stones...
#nephtwitter #FOAMed #MedEd #uronephrology #kidneystone #nephrolith
Which is a risk factor for calcium oxalate stones?
Correct!
Risk factors for calcium oxalate stones classically include hypercalciuria and
hypercalciuria and  hyperoxaluria along with
hyperoxaluria along with  low urine volume.
low urine volume.
#Hypercalciuria can stem from a LOT of different causes and clinical settings. The most common in adults is idiopathic.
Risk factors for calcium oxalate stones classically include
 hypercalciuria and
hypercalciuria and  hyperoxaluria along with
hyperoxaluria along with  low urine volume.
low urine volume.#Hypercalciuria can stem from a LOT of different causes and clinical settings. The most common in adults is idiopathic.
There is debate about whether hyperuricosuria can serve as a nidus for CaOx stones.
https://pubmed.ncbi.nlm.nih.gov/18059457/
Hypocitraturia and high urine pH (>7.0) tend to be stronger risk factors for CaP stones (we’ll discuss that later!)
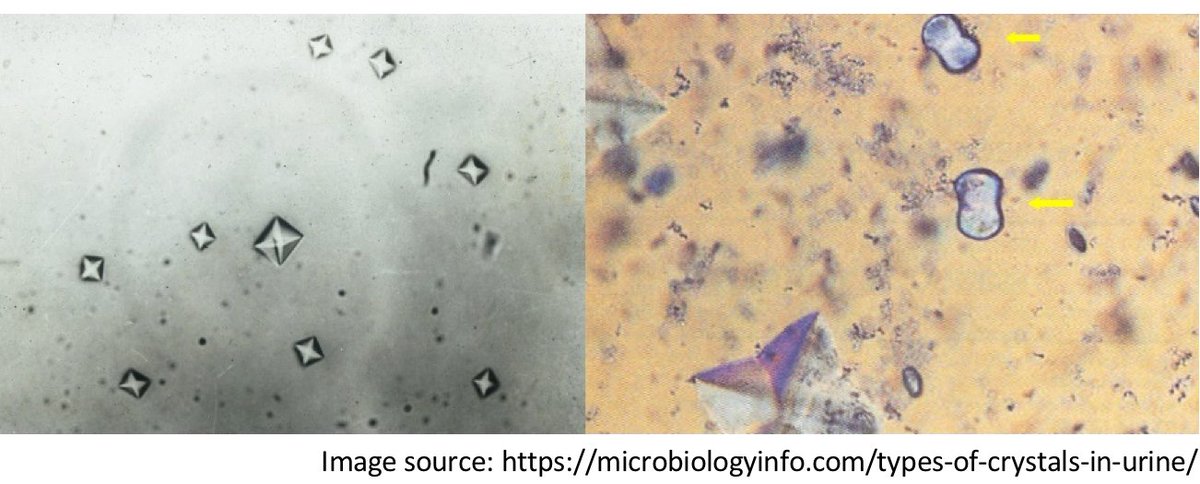
Photo courtesy of @porische
https://pubmed.ncbi.nlm.nih.gov/18059457/
Hypocitraturia and high urine pH (>7.0) tend to be stronger risk factors for CaP stones (we’ll discuss that later!)
Photo courtesy of @porische
What is the link between hypercalciuria and salt ( NaCl) intake?
NaCl) intake?
 NaCl) intake?
NaCl) intake?
Right!  More NaCl -->
More NaCl -->  Urine Calcium
Urine Calcium
 How does this happen?!
How does this happen?!
 The kidney has the answer.
The kidney has the answer.
In the proximal tubule, Ca reabsorption is linked with
Ca reabsorption is linked with  Na reabsorption.
Na reabsorption.
With more Na reabsorption,
Na reabsorption,  H2O follows paracellularly and “drags”
H2O follows paracellularly and “drags”  Ca along with it. #solventdrag
Ca along with it. #solventdrag
 More NaCl -->
More NaCl -->  Urine Calcium
Urine Calcium How does this happen?!
How does this happen?! The kidney has the answer.
The kidney has the answer.In the proximal tubule,
 Ca reabsorption is linked with
Ca reabsorption is linked with  Na reabsorption.
Na reabsorption.With more
 Na reabsorption,
Na reabsorption,  H2O follows paracellularly and “drags”
H2O follows paracellularly and “drags”  Ca along with it. #solventdrag
Ca along with it. #solventdrag
In the DCT,  increased
increased  Na delivery reduces the stimulus for Na/Ca exchange on the basolateral membrane
Na delivery reduces the stimulus for Na/Ca exchange on the basolateral membrane
This results in less Ca influx via TRVP5 channel.
less Ca influx via TRVP5 channel.
 If you understand this, you understand why normal saline is effective in hypercalcemia.
If you understand this, you understand why normal saline is effective in hypercalcemia.
https://pubmed.ncbi.nlm.nih.gov/27009338/
 increased
increased  Na delivery reduces the stimulus for Na/Ca exchange on the basolateral membrane
Na delivery reduces the stimulus for Na/Ca exchange on the basolateral membraneThis results in
 less Ca influx via TRVP5 channel.
less Ca influx via TRVP5 channel. If you understand this, you understand why normal saline is effective in hypercalcemia.
If you understand this, you understand why normal saline is effective in hypercalcemia.https://pubmed.ncbi.nlm.nih.gov/27009338/
Now, what is the link between hypercalciuria and  acidosis?
acidosis?
 acidosis?
acidosis?
Essentially besides leaching Ca from  bones, acidosis
bones, acidosis  uncouples Na reabs from Ca reabs in the DCT.
uncouples Na reabs from Ca reabs in the DCT.
In acidosis,
 PT: Na and Ca reabs linked
PT: Na and Ca reabs linked
 DCT:
DCT:  LESS Ca influx due to inhibition of TRPV5 and reduced TRPV5 mRNA due to H+
LESS Ca influx due to inhibition of TRPV5 and reduced TRPV5 mRNA due to H+
 Net effect:
Net effect:  more UrCa
more UrCa
https://pubmed.ncbi.nlm.nih.gov/27468975/
 bones, acidosis
bones, acidosis  uncouples Na reabs from Ca reabs in the DCT.
uncouples Na reabs from Ca reabs in the DCT.In acidosis,
 PT: Na and Ca reabs linked
PT: Na and Ca reabs linked DCT:
DCT:  LESS Ca influx due to inhibition of TRPV5 and reduced TRPV5 mRNA due to H+
LESS Ca influx due to inhibition of TRPV5 and reduced TRPV5 mRNA due to H+ Net effect:
Net effect:  more UrCa
more UrCahttps://pubmed.ncbi.nlm.nih.gov/27468975/
In the work up of hypercalciuria in calcium stone formers, it is important to consider  monogenetic causes (esp in pediatrics)
monogenetic causes (esp in pediatrics)
https://pubmed.ncbi.nlm.nih.gov/15689405/
https://pubmed.ncbi.nlm.nih.gov/18446382/
https://pubmed.ncbi.nlm.nih.gov/18836558/
 monogenetic causes (esp in pediatrics)
monogenetic causes (esp in pediatrics)https://pubmed.ncbi.nlm.nih.gov/15689405/
https://pubmed.ncbi.nlm.nih.gov/18446382/
https://pubmed.ncbi.nlm.nih.gov/18836558/
When the initial screen and/or work up are negative, we’re stuck with  idiopathic hypercalciuria.
idiopathic hypercalciuria.
 idiopathic hypercalciuria.
idiopathic hypercalciuria.
 You may ask, should you counsel patients to reduce Ca intake to reduce risk of Ca stones and hypercalciuria?!
You may ask, should you counsel patients to reduce Ca intake to reduce risk of Ca stones and hypercalciuria?!
Correct, you should not.
Calcium intake has been found to reduce risk of stone formation likely by binding intestinal oxalate and reducing oxalate absorption.
https://pubmed.ncbi.nlm.nih.gov/8441427/
Calcium intake has been found to reduce risk of stone formation likely by binding intestinal oxalate and reducing oxalate absorption.
https://pubmed.ncbi.nlm.nih.gov/8441427/
But, (a) #PUSHing fluid increases urine volume (ie lower the concentration of urinary calcium and reduce the relative supersaturation)
increases urine volume (ie lower the concentration of urinary calcium and reduce the relative supersaturation)
Coffee, tea, wine, beer, high citrate juices seem ok.
https://twitter.com/lieske_john/status/1334890304617541633
https://pubmed.ncbi.nlm.nih.gov/23676355/
 increases urine volume (ie lower the concentration of urinary calcium and reduce the relative supersaturation)
increases urine volume (ie lower the concentration of urinary calcium and reduce the relative supersaturation)Coffee, tea, wine, beer, high citrate juices seem ok.

https://twitter.com/lieske_john/status/1334890304617541633
https://pubmed.ncbi.nlm.nih.gov/23676355/
Encourage low salt diet (UrNa goal < 80-100 mEq per day) and consider thiazide diuretics.
https://pubmed.ncbi.nlm.nih.gov/20042524/
https://pubmed.ncbi.nlm.nih.gov/20042524/
Hope that helps the next time you have a calcium stone former with hypercalciuria.
Suggestions/comments are always welcome! #uronephrology #kidneystone #nephrolith
Next up?
Suggestions/comments are always welcome! #uronephrology #kidneystone #nephrolith
Next up?

 Read on Twitter
Read on Twitter