1/25 nursing homes make up ~50% of Covid19 deaths but just ~1% of the population all over the Western world. we are proposing an INTERDISCIPLINARY APPROACH to improve outcomes and understanding. a thread with questions and sources @LTCcovid @AdelinaCoHe @keiserolivia @samiahurst
2/n Terminology: why are we using "nursing home" instead of "long term care facility" in this thread. we are using NH as a synonym for LTCF in because 1. it is better understood by laypersons and 2. it is shorter. In some visualizations shown below the French acronym is EMS.
3a/n Nursing home residents make up ~1% of the overall population? yes, look at bed capacities published by WHO and national/local governments. in many countries it is even less https://gateway.euro.who.int/en/indicators/hfa_490-5100-nursing-and-elderly-home-beds-per-100-000/
3b/n USA has 1.7 mio licensed NH beds for 328 mio people = 0.5% https://www.cdc.gov/nchs/fastats/nursing-home-care.htm US nursing home Covid-19 death share is over 100'000 already = ~40% of deaths https://www.kff.org/policy-watch/covid-19-has-claimed-the-lives-of-100000-long-term-care-residents-and-staff/
4a/n Nursing home residents make up ~50% of Covid-19 deaths all over the Western world? Yes. Raw data (following in subsequent tweets) is showing a range ~30-70% but keep in mind testing differences in NHs and counting of suspected deaths (not tested) in some jurisdictions (BEL).
4b/n use excess mortality data as a control for reporting and counting differences of covid19 deaths, especially in nursing homes https://twitter.com/CoronaReduit/status/1335961622599364612
4c/n SAGE (UK) has done a comparison between excess mortality and covid deaths before 2nd wave hit Europe and the US. It showed a wide range of underreporting (ESP -40%) or even slight overreporting (BEL +10%) of covid deaths relative to excess mortality. https://journals.sagepub.com/doi/full/10.1177/0141076820956802
4d/n @LTCcovid @AdelinaCoHe has collected a wide range of data on covid deaths in nursing homes that should be interpreted in light of reporting differences mentioned above https://ltccovid.org/wp-content/uploads/2020/06/Mortality-associated-with-COVID-among-people-who-use-long-term-care-26-June.pdf
4e/n we have visualized some of the raw data for the 1st wave. It shows the disproportionate burden covid imposes on the ~1% of the population living in nursing homes. symmetry exists between C19 deaths inside NHs and outside regardless of seroprevalence https://public.tableau.com/views/CoronaReduit/Deathsinnursinghomes
4f/n this symmetry/correlation was incredibly constant over the trajectory of both spring and autumn waves in Sweden: nursing home ("äldreboende") C19 deaths ("avlidna") vs rest of population ("ej"). NH bed capacity is 1.3% of Swedish population. https://www.folkhalsomyndigheten.se/globalassets/statistik-uppfoljning/smittsamma-sjukdomar/veckorapporter-covid-19/2020/covid-19-veckorapport-vecka-47-final.pdf
5/n symmetry raises question why hygienical precautions in nursing homes don't seem to work while more effective in hospitals? 1. dementia limiting grasp of hygiene? 2. personnel shortages (sick working)? 3. unfiltered air conditioning? 4. lack of (quick) testing? 5. trade-offs?
6a/n some Swiss cantons like Geneva, Zürich, Aargau have published data on locations of deaths. it shows that 1. nursing home residents are rarely hospitalized 2. almost nobody dies at home. it is either in the hospital or the nursing home. roughly 50/50. https://www.ge.ch/document/covid-19-bilan-epidemiologique-hebdomadaire
6b/n the low hospitalization rate of nursing home residents relative to age peers is not particular to Covid. it existed prior to Covid in Switzerland. people from other countries can probably confirm this pattern. https://www.bfs.admin.ch/bfs/fr/home/statistiques/catalogues-banques-donnees/publications.assetdetail.7267445.html
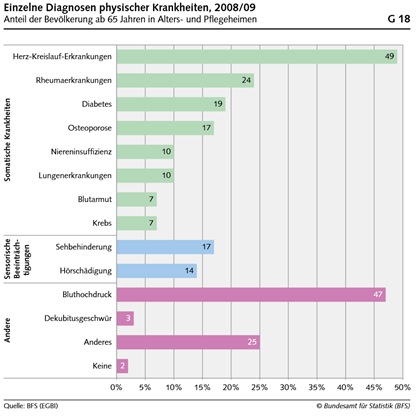
6c/n why are NH residents rarely hospitalized? likely rooted in palliative considerations and advance health care directives (living wills). most have high frailty score (FS) and prognoses of improvement for many serious health conditions are negative. https://docplayer.org/138436-Gesundheit-von-betagten-in-alters-und-pflegeheimen-erhebung-zum-gesundheitszustand-von-betagten-personen-in-institutionen-2008-09-gesundheit.html
6d/n clinical frailty score (CFS) is a good predictor of relative covid outcomes in hospitalizations, incl. ICU. frailty is the main reason why somebody lives in a nursing home. https://www.thelancet.com/journals/lanpub/article/PIIS2468-2667(20)30146-8/fulltext
7a/n this leads to the question of life expectancy. how many life months/years are nursing home residents losing due to premature death from Covid19? Studies claiming 10 years or more lost are clearly wrong for NH residents, ie ~50% of deaths. Data see following tweets.
7b/n we looked at Swiss yearly deaths in nursing homes since 2010 about 30% of bed capacity is dying every year. that is 42% of all deaths in 1% of pop. keep in mind: bed capacity includes short term care (~10%), is not fully occupied, some younger dementia patients stay >decade
7c/n in 2017, 1/2 of male NH residents in Switzerland died 12 months after moving in, 1/4 died in less than 3 months. we have been told that this has shortened since then due to shortage of beds and political prioritization of ambulant at home care. https://www.bfs.admin.ch/bfs/fr/home/statistiques/catalogues-banques-donnees/publications.assetdetail.7267445.html
7d/n similar data is available for the US and many other countries. somebody should do a proper statistical analysis. the data exists, but is scattered in public and private databases. given the relevance for planning and budgeting this is surprising. https://www.ucsf.edu/news/2010/08/98172/social-support-key-nursing-home-length-stay-death
8a/n given the high death toll relative to bed capacity, it is important to understand infection fatality rates (IFR), seroprevalence and transmission patterns. are some NHs at herd immunity threshold (HIT) while others are untouched? or is it more symmetrical?
8b/n infection fatality rates (IFR) for nursing home residents are estimated around ~25% https://www.sciencedirect.com/science/article/pii/S0163445320303480 higher than any other group. In the USA, 100'000/1'700'000 beds died = 5.9% of bed capacity. At ~25% IFR that is a seroprevalence of AT LEAST 23.5%. If IFR lower more!
8c/n Important for models: If seroprevalence is much higher in NH and IFR is also much higher: What does this mean for overall population wide IFR projections from seroprevalence studies that usually do not include samples from nursing homes?
8d/n we are calling on researchers conducting antibody and t cell studies to focus on NHs. this is important for IFR, VACCINATION strategy, and understanding/improvement of hygiene. this needs interdisciplinary cooperation. we can help to organize private funding and coordination
9/n besides nursing home residents, ambulant at home elderly care patients also seem to be affected disproportionally, 14.5% of deaths in data from Geneva below. they do not die at home, though. they are hospitalized. CASE fatality rate (not IFR) is <10% https://www.ge.ch/document/19696/telecharger
Finally, we are offering free support incl. private fundraising to any researchers, activists or journalists willing to work on these matters: [email protected] this is a sobering, sometimes even depressing topic. it needs to be approached rationally without any tabooization

 Read on Twitter
Read on Twitter