New evidence that COVID-19 may be drastically exacerbating the US opioid crisis:
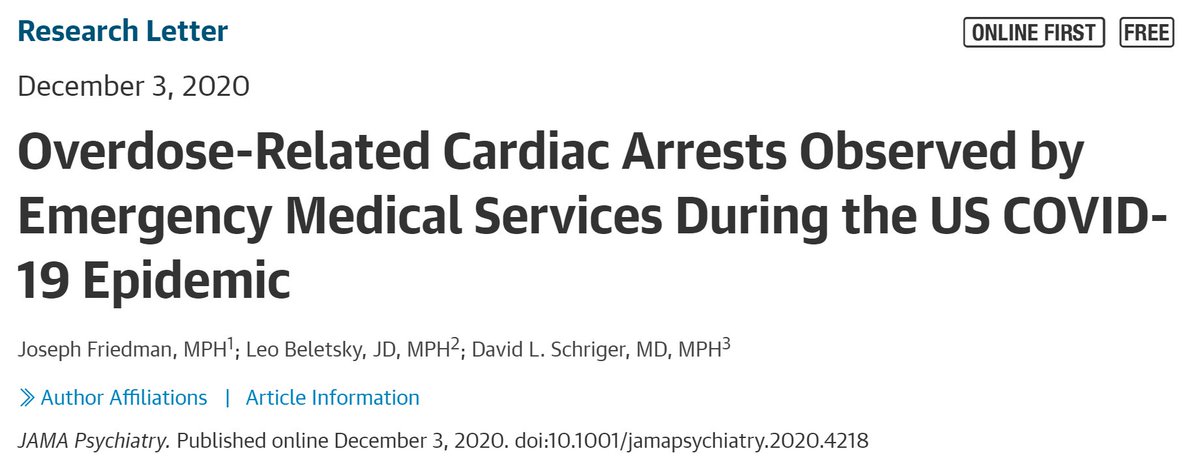
"Overdose-Related Cardiac Arrests Observed by Emergency Medical Services During the US COVID-19 Epidemic"
w/ @LeoBeletsky, available for free in @JAMAPsych
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2773768



"Overdose-Related Cardiac Arrests Observed by Emergency Medical Services During the US COVID-19 Epidemic"
w/ @LeoBeletsky, available for free in @JAMAPsych
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2773768



Many people are concerned that COVID-19 is exacerbating the (already growing) overdose crisis, but mortality databases have long lags that impede timely monitoring. The CDC did not release preliminary 2019 number until JULY of 2020.
While we wait, people have cobbled together preliminary data from coroners offices, etc (including a notable article from NYtimes, and great efforts from @OverdoseUpdates). But nothing nationally representative or with granular time info.
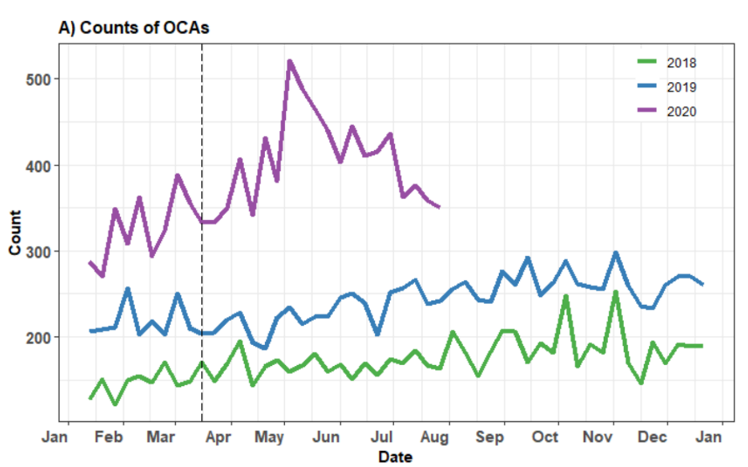
We use data from NEMSIS, a large registry of over 10,000 EMS agencies in 47 states that represented over 80% of all EMS activations nationally in 2020. Data are uploaded to NEMSIS in NEAR REAL TIME! So we can track shifts in a timely manner.
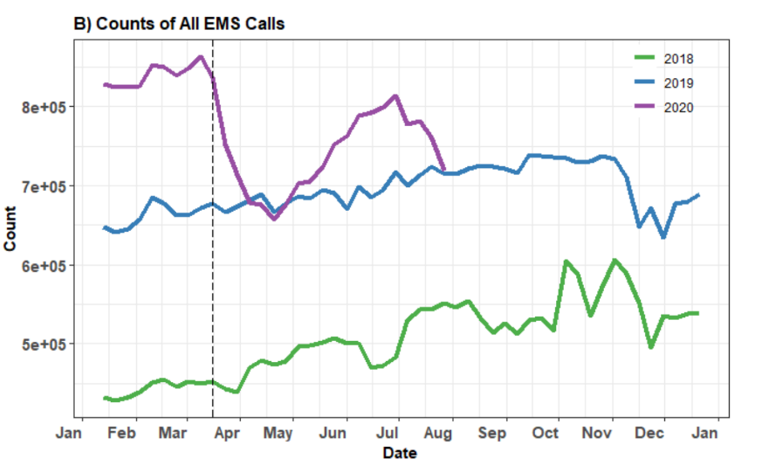
We calculated weekly rates of overdose-related cardiac arrests, and all overdose-related calls, observed by EMS.
Because new agencies joined NEMSIS over the 3-year study period, we calculated rates per 100,000 EMS activations/calls (more on this below).
Because new agencies joined NEMSIS over the 3-year study period, we calculated rates per 100,000 EMS activations/calls (more on this below).
We find a sharp increase in overdose-related cardiac arrests starting in April, reaching a peak in early May, and remaining elevated through the end of the study period (August 1st).
Compared to baseline (the average of 2018+2019), rates in 2020 were overall elevated by +48.5%. The peak in May was +123.4% over baseline.
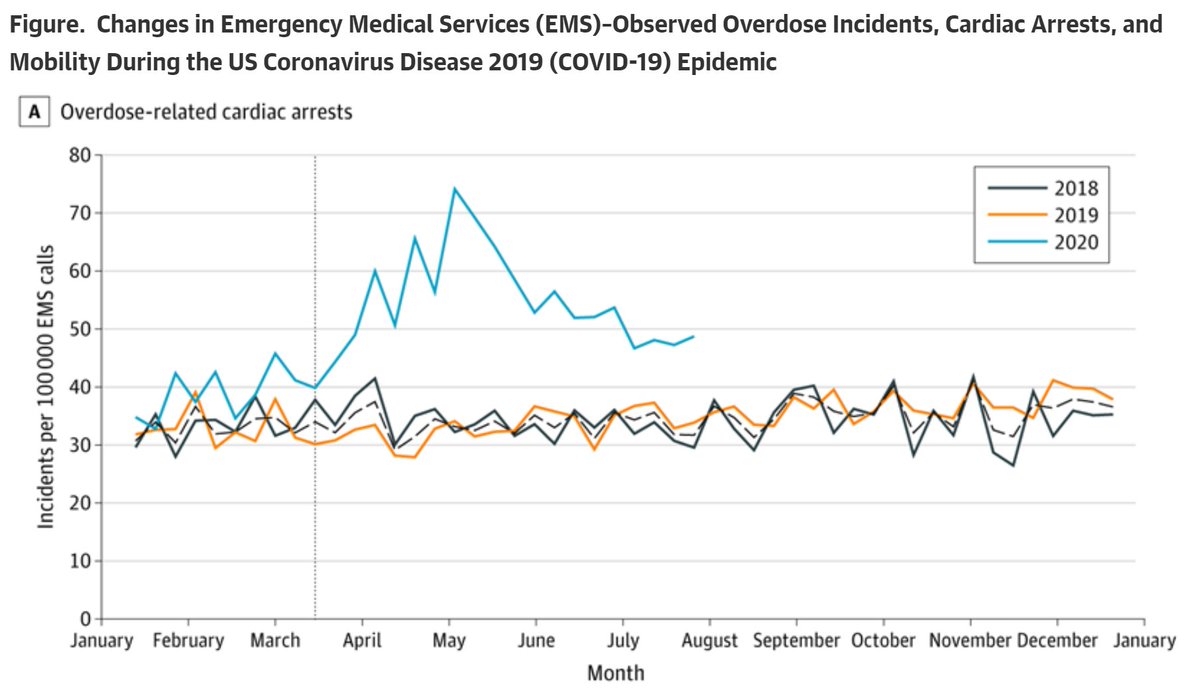
Increases in overdose-related cardiac arrests lined up well with reductions in mobility (measured using cellphone data). Both reach peak disruption early May, and slowly drift towards baseline through August.
To me this suggests that social isolation may play a key role.
To me this suggests that social isolation may play a key role.
We also measured changes in all overdose-related EMS calls. They were up ~17% in 2020.
If fatal overdose incidents are increasing faster than total (fatal+nonfatal) that could suggest a rising case fatality rate (each overdose incident becoming more deadly).
If fatal overdose incidents are increasing faster than total (fatal+nonfatal) that could suggest a rising case fatality rate (each overdose incident becoming more deadly).
Many trends predicted by experts could cause this: e.g. more people using alone, disruptions to the illicit or licit drug supply, reduced access to harm reduction and medical treatment.
See this insightful piece from @DrSarahWakeman & co. on the topic https://www.nature.com/articles/s41591-020-0898-0
See this insightful piece from @DrSarahWakeman & co. on the topic https://www.nature.com/articles/s41591-020-0898-0
Limitations: this is a large cohort of EMS data. EMS don't observe all overdose fatalities in the US. If the proportion of overdose deaths observed by EMS shifted during the pandemic that could bias our results up or down.
This is a just proxy for the total death rate.
This is a just proxy for the total death rate.
Despite limitations, our results do suggest that overdoses may be strongly on the rise in 2020. So, we need to invest heavily in substance use trx, harm reduction, and the structural drivers of overdose as core elements of the COVID-19 response.
Short term: we should reduce financial and logistical barriers for accessing safe opioid supply, allow pharmacies to dispense methadone, allow all physicians to prescribe buprenorphine without a special waiver, release emergency funds to make these medications affordable for all.
Long term: overdose is a symptom of structural problems in the US. We need to invest in making employment, housing, education, healthcare accessible to all to address the upstream drivers of overdose.
A huge thanks to my co-authors @LeoBeletsky and David Schriger! https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2773768
Here are answers to some of the most common questions we're received:
Q. Are overdose-related cardiac arrests the same as deaths?
A. We don't know for sure. But based on the clinical experience of the team, we think that many/most overdoses that proceed to cardiac arrests do ultimately result in death.
A. We don't know for sure. But based on the clinical experience of the team, we think that many/most overdoses that proceed to cardiac arrests do ultimately result in death.
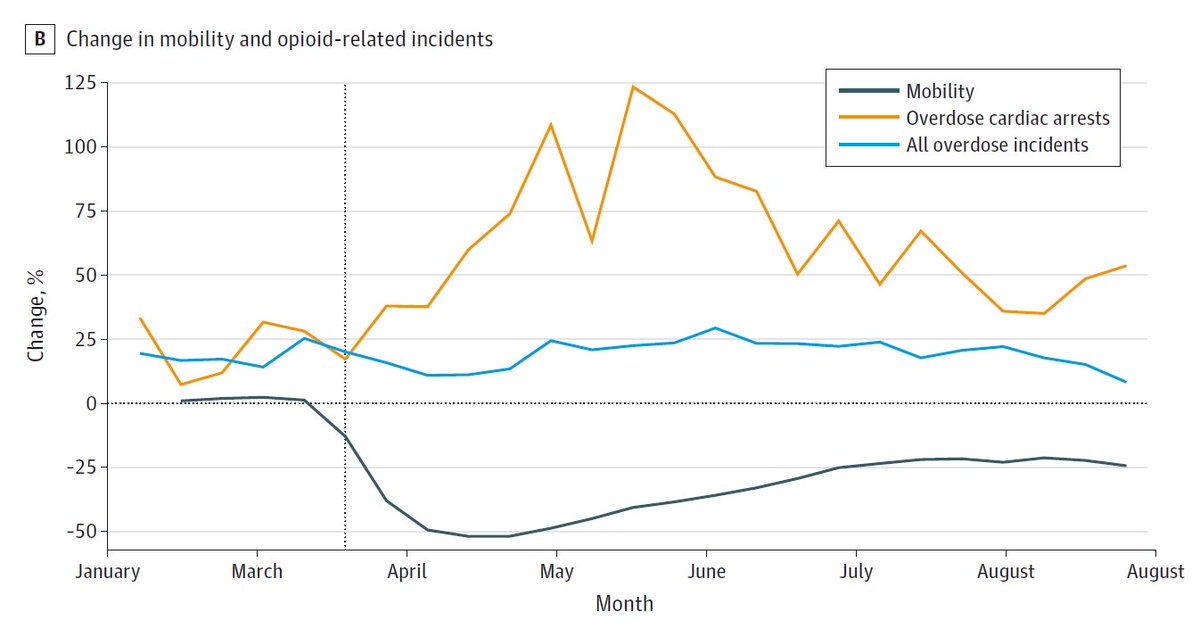
Q. Why don't you show absolute counts of cardiac arrests?
A. One challenge of working with NEMSIS data is that new agencies join over time. Therefore, we would expect the overdose-related cardiac arrests to go up over time too, just from more calls being recorded...
A. One challenge of working with NEMSIS data is that new agencies join over time. Therefore, we would expect the overdose-related cardiac arrests to go up over time too, just from more calls being recorded...
We therefore adjust by using a rate of cardiac arrests / call volume. This is a better approach for long-term analyses, but we were concerned that decreased call volume during COVID-19 could explain some of our findings. Therefore, we did a sensitivity analysis (in supplement)...
...where we held the denominator (call volume) constant for all of 2020 at the pre-pandemic call volume (from weeks 1-10).
After this adjustment, 2020 rates were still up about +40% of baseline, compared to about +%50 in the main analysis with a dynamic denominator.
After this adjustment, 2020 rates were still up about +40% of baseline, compared to about +%50 in the main analysis with a dynamic denominator.
Here's a graph (twitter exclusive, since JAMA doesn't allow graphs in the supplement for RLs) showing the absolute counts of overdose-related cardiac arrests. It illustrates -the issue with using counts for the whole analysis: the increases from 2018 to 2019 are artifact.
But they go away when we adjust for call volume. Yet here and above large increases can be seen during COVID-19.
Here is the (15%-20%) drop in call volume that concerned us, and caused us to do the sensitivity analysis.

 Read on Twitter
Read on Twitter