With the rollout of SARS-CoV2 vaccines imminent, many are asking about the scientific evidence behind prioritization strategies. Here, I summarize the evidence from our past work (on influenza) that can help us think about COVID vaccination. (1/)
1a. One classic question is whether a limited supply of vaccines should be #1: used to protect the vulnerable directly; or #2: used to protect healthy & more transmissible individuals to protect the vulnerable indirectly. We see [link ] while strategy #2 does minimize morbidity,
] while strategy #2 does minimize morbidity,
 ] while strategy #2 does minimize morbidity,
] while strategy #2 does minimize morbidity,
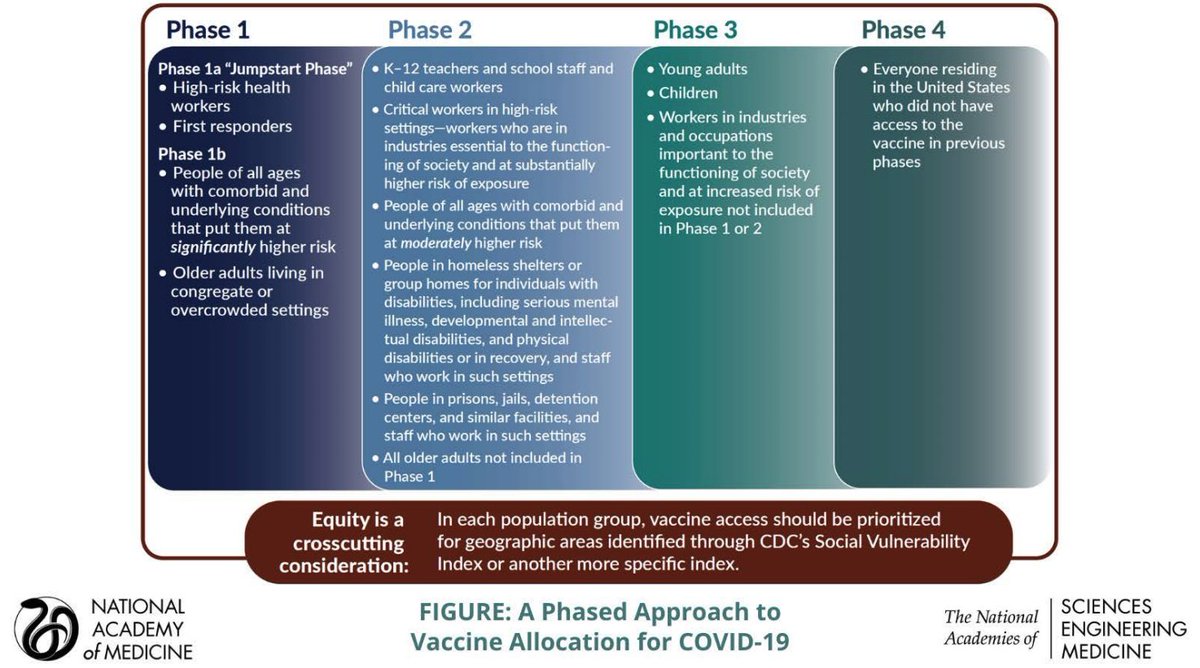
1b. strategy #1 is key for minimizing mortality, particularly for diseases with high transmission rate (such as COVID-19). This is why Phase 1c of the proposed COVID prioritization is focused on vaccinating the elderly and those with co-morbidities. (3/)
http://bansallab.com/publications/flu.pdf
http://bansallab.com/publications/flu.pdf
2a. As COVID treatment improves, another question is whether treatment is an alternative for vaccination. We've found [link ] that even a targeted treatment cannot replace a robust vaccine (even with a low-efficacy vaccine, which is not an issue with COVID
] that even a targeted treatment cannot replace a robust vaccine (even with a low-efficacy vaccine, which is not an issue with COVID  )
)
 ] that even a targeted treatment cannot replace a robust vaccine (even with a low-efficacy vaccine, which is not an issue with COVID
] that even a targeted treatment cannot replace a robust vaccine (even with a low-efficacy vaccine, which is not an issue with COVID  )
)
2b. This work also illustrates the diff b/n transmission-blocking vs. susceptibility-reducing effects. We still don't know exactly how the Moderna/Pfizer vaccines protect individuals, but we do know that susceptibility-reducing >> transmission-blocking.
http://bansallab.com/publications/kramer_antivirals.pdf
http://bansallab.com/publications/kramer_antivirals.pdf
3a. Another issue is how we vaccinate in light of past transm. We've suggested [link ] that for a "2nd wave" of a novel disease, superspreaders are no longer most infected. Instead, those with moderate transmission potential are & should be vaccinated.
] that for a "2nd wave" of a novel disease, superspreaders are no longer most infected. Instead, those with moderate transmission potential are & should be vaccinated.
http://bansallab.com/publications/flushift.pdf
 ] that for a "2nd wave" of a novel disease, superspreaders are no longer most infected. Instead, those with moderate transmission potential are & should be vaccinated.
] that for a "2nd wave" of a novel disease, superspreaders are no longer most infected. Instead, those with moderate transmission potential are & should be vaccinated.http://bansallab.com/publications/flushift.pdf
3b. However, it's important to understand that most of US still has low seroprevalence (i.e. not done with 1st wave), and there are many superspreaders out there. This is why we must keep up social distancing & masks & reduce gatherings till we have sufficient vaccination.
3c. This is also why the COVID vaccination recommendations prioritize in Phase 1 and 2 essential workers, teachers, and those in high-density settings like prisons, factories, shelters.
4a. Then there's the question of whether we should vaccinate previously infected individuals. Our work shows that the population-level consequences of "wasting" vaccines on previously-infected individuals aren't dire.
http://bansallab.com/publications/mooring_article.pdf
http://bansallab.com/publications/mooring_article.pdf
4b. The current COVID vaccine recommendation (at least for healthcare workers in Phase 1a) is to not vaccinate those with known infection in the 90 days, though serologic testing is not recommended prior to vaccination.

 Read on Twitter
Read on Twitter