Seeing as the COVID-19 #vaccine will be an extremely limited resource initially, should we consider testing each potential recipient for SARS-CoV-2 IgG positivity before administering the vaccine in distribution Phase 1a? 1b?
#MedTwitter
#epitwitter
#MedTwitter
#epitwitter
Let's turn this into a #MedTwitter thread to explore this question!
1/
First, the ACIP announced its recommending to @CDCgov that healthcare personnel and residents of long-term care facilities be prioritized in phase 1a for the COVID-19 vaccine. https://twitter.com/DrNancyM_CDC/status/1333906487178047489?s=20
1/

First, the ACIP announced its recommending to @CDCgov that healthcare personnel and residents of long-term care facilities be prioritized in phase 1a for the COVID-19 vaccine. https://twitter.com/DrNancyM_CDC/status/1333906487178047489?s=20
2/
The Advisory Committee on Immunization Practices (ACIP) says its recs to @CDCgov were built upon 3 published early COVID-19 vaccine allocation frameworks:
 @WHO SAGE
@WHO SAGE
 @JohnsHopkinsSPH
@JohnsHopkinsSPH
 @theNASEM
@theNASEM
https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-09/COVID-06-Oliver.pdf
(slide 3)
The Advisory Committee on Immunization Practices (ACIP) says its recs to @CDCgov were built upon 3 published early COVID-19 vaccine allocation frameworks:
 @WHO SAGE
@WHO SAGE @JohnsHopkinsSPH
@JohnsHopkinsSPH  @theNASEM
@theNASEM https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-09/COVID-06-Oliver.pdf
(slide 3)
3/
The primary question we are asking is, I think, deceptively simple:
"Should individuals undergo serologic testing prior to SARS-CoV-2 vaccination in phase 1a?"
CC:
@DrNancyM_CDC @nataliexdean @BillHanage @covidperspectiv @DrEricDing @EricTopol @DrTomFrieden
The primary question we are asking is, I think, deceptively simple:
"Should individuals undergo serologic testing prior to SARS-CoV-2 vaccination in phase 1a?"
CC:
@DrNancyM_CDC @nataliexdean @BillHanage @covidperspectiv @DrEricDing @EricTopol @DrTomFrieden
4/
Let's first explore what each of the early COVID-19 vaccine allocation frameworks has to say on the topic:
 The @WHO SAGE framework says they considered existing immunity but did not specifically take it into account in developing their "Roadmap"
The @WHO SAGE framework says they considered existing immunity but did not specifically take it into account in developing their "Roadmap"
https://www.who.int/docs/default-source/immunization/sage/covid/sage-prioritization-roadmap-covid19-vaccines.pdf?Status=Temp&sfvrsn=bf227443_2&ua=1
Let's first explore what each of the early COVID-19 vaccine allocation frameworks has to say on the topic:
 The @WHO SAGE framework says they considered existing immunity but did not specifically take it into account in developing their "Roadmap"
The @WHO SAGE framework says they considered existing immunity but did not specifically take it into account in developing their "Roadmap"https://www.who.int/docs/default-source/immunization/sage/covid/sage-prioritization-roadmap-covid19-vaccines.pdf?Status=Temp&sfvrsn=bf227443_2&ua=1
5/
 @JohnsHopkinsSPH's framework touches on seropositivity briefly, stating that at that time time, way back in August, it was unclear if seropositivity = proof of effective immunity, and thus they did not plan to take this into account in prioritizing allocation.
@JohnsHopkinsSPH's framework touches on seropositivity briefly, stating that at that time time, way back in August, it was unclear if seropositivity = proof of effective immunity, and thus they did not plan to take this into account in prioritizing allocation.
 @JohnsHopkinsSPH's framework touches on seropositivity briefly, stating that at that time time, way back in August, it was unclear if seropositivity = proof of effective immunity, and thus they did not plan to take this into account in prioritizing allocation.
@JohnsHopkinsSPH's framework touches on seropositivity briefly, stating that at that time time, way back in August, it was unclear if seropositivity = proof of effective immunity, and thus they did not plan to take this into account in prioritizing allocation.
6/
@JohnsHopkinsSPH's framework forces us to asks an important question, namely:
 Does SARS-CoV-2 IgG positivity provide "proof" of effective #immunity?
Does SARS-CoV-2 IgG positivity provide "proof" of effective #immunity?
This will be a key part of our assumptions in building an answer to our primary question a bit later.
@JohnsHopkinsSPH's framework forces us to asks an important question, namely:
 Does SARS-CoV-2 IgG positivity provide "proof" of effective #immunity?
Does SARS-CoV-2 IgG positivity provide "proof" of effective #immunity?This will be a key part of our assumptions in building an answer to our primary question a bit later.
7/
 @theNASEM's framework does give some thought to the possibility that a population with high prevalence of prior infection might not be an ideal group to allocate an extremely limited vaccine.
@theNASEM's framework does give some thought to the possibility that a population with high prevalence of prior infection might not be an ideal group to allocate an extremely limited vaccine.
 @theNASEM's framework does give some thought to the possibility that a population with high prevalence of prior infection might not be an ideal group to allocate an extremely limited vaccine.
@theNASEM's framework does give some thought to the possibility that a population with high prevalence of prior infection might not be an ideal group to allocate an extremely limited vaccine.
8/
Now let's see if ACIP has addressed our primary question in their recommendations to @CDCgov in @CDCMMWR
In short, no explicit mention is made of prior SARS-CoV-2 infection or existing immunity in individuals or in specific populations. However... https://www.cdc.gov/mmwr/volumes/69/wr/mm6947e3.htm
Now let's see if ACIP has addressed our primary question in their recommendations to @CDCgov in @CDCMMWR
In short, no explicit mention is made of prior SARS-CoV-2 infection or existing immunity in individuals or in specific populations. However... https://www.cdc.gov/mmwr/volumes/69/wr/mm6947e3.htm
9/
...the ACIP does recommend identifying groups who would derive *greatest* benefit.
The groups they chose: healthcare personnel and residents of LTC facilities, seem totally reasonable!
But how do we make sure we aren't mis-allocating individual doses of the #vaccine?
...the ACIP does recommend identifying groups who would derive *greatest* benefit.
The groups they chose: healthcare personnel and residents of LTC facilities, seem totally reasonable!
But how do we make sure we aren't mis-allocating individual doses of the #vaccine?
10/
This is important because although on average, these groups are at "highest-risk" for infection (HCP) or severe #COVID-19 & death (LTC residents), individual risk varies *widely* and is particularly impacted by...
...you guessed it:
-->pre-existing immunity to SARS-CoV-2!
This is important because although on average, these groups are at "highest-risk" for infection (HCP) or severe #COVID-19 & death (LTC residents), individual risk varies *widely* and is particularly impacted by...
...you guessed it:
-->pre-existing immunity to SARS-CoV-2!
12/
A critical aside: based on the findings of Iyer et. al in @medrxivpreprint, it seems reasonable to assume, for the purposes of our discussion, that SARS-CoV-2 IgG seropositivity is in fact a good surrogate for durable and effective immunity.
Study: https://pubmed.ncbi.nlm.nih.gov/32743600/
A critical aside: based on the findings of Iyer et. al in @medrxivpreprint, it seems reasonable to assume, for the purposes of our discussion, that SARS-CoV-2 IgG seropositivity is in fact a good surrogate for durable and effective immunity.
Study: https://pubmed.ncbi.nlm.nih.gov/32743600/
13/
4) So we'll use this number, 3,201, to represent our prevalence of *immunity*.
If we had a perfect diagnostic test, it would correctly identify all 3,201 ppl with (+)IgG and all 96,799 ppl with (-)IgG, enabling us to save 3,201*2 doses/person = 6,402 doses of the vaccine.
4) So we'll use this number, 3,201, to represent our prevalence of *immunity*.
If we had a perfect diagnostic test, it would correctly identify all 3,201 ppl with (+)IgG and all 96,799 ppl with (-)IgG, enabling us to save 3,201*2 doses/person = 6,402 doses of the vaccine.
14/
However, we need to assess how this would play out w/ a real test that isn’t perfect:
SARS-CoV-2 IgG tests were found in an @CochraneLibrary review to have a sensitivity of 57.9% to 91.8% (strongly time-dependent) and a specificity of 98.3% to 99.6% https://pubmed.ncbi.nlm.nih.gov/32584464/
However, we need to assess how this would play out w/ a real test that isn’t perfect:
SARS-CoV-2 IgG tests were found in an @CochraneLibrary review to have a sensitivity of 57.9% to 91.8% (strongly time-dependent) and a specificity of 98.3% to 99.6% https://pubmed.ncbi.nlm.nih.gov/32584464/
15/
For the purpose of our modeling, we’ll ignore infections within the past 14 days (since they will be expected to contribute a relatively small % of the total number of true infections in our population), this would give us an expected sensitivity of ~84%.
PMID: 32584464
For the purpose of our modeling, we’ll ignore infections within the past 14 days (since they will be expected to contribute a relatively small % of the total number of true infections in our population), this would give us an expected sensitivity of ~84%.
PMID: 32584464
16/
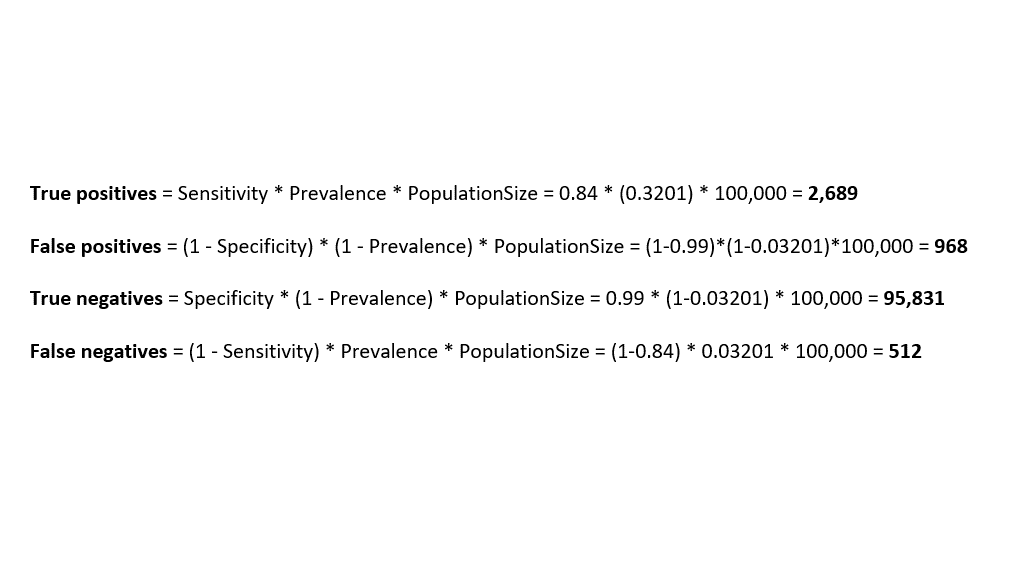
With an IgG test with a sensitivity of 84% and a specificity of 99%, in a population of 100,000 HCPs with prevalence of 3.201% true positives, we could expect:
-2,689 true positives
-968 false positives
-95,831 true negatives
-512 false negatives
With an IgG test with a sensitivity of 84% and a specificity of 99%, in a population of 100,000 HCPs with prevalence of 3.201% true positives, we could expect:
-2,689 true positives
-968 false positives
-95,831 true negatives
-512 false negatives
17/
Meaning:
- 2,689 ppl correctly DO NOT get the , as they are already immune
, as they are already immune
- 95,831 ppl correctly get the , as they are truly non-immune
, as they are truly non-immune
- 968 ppl incorrectly DO NOT get the , as they are actually non-immune
, as they are actually non-immune
- 512 ppl incorrectly get the , as they are already immune
, as they are already immune
Meaning:
- 2,689 ppl correctly DO NOT get the
 , as they are already immune
, as they are already immune- 95,831 ppl correctly get the
 , as they are truly non-immune
, as they are truly non-immune- 968 ppl incorrectly DO NOT get the
 , as they are actually non-immune
, as they are actually non-immune- 512 ppl incorrectly get the
 , as they are already immune
, as they are already immune
18/
So, after testing a population of 100,000 HCPs with an *immunity* prevalence of 3.2%, we could expect that we would administer (95,831 + 512)*2 =192,686 doses of the vaccine.
We will have “saved” 7314 doses of the vaccine, but in so doing...
So, after testing a population of 100,000 HCPs with an *immunity* prevalence of 3.2%, we could expect that we would administer (95,831 + 512)*2 =192,686 doses of the vaccine.
We will have “saved” 7314 doses of the vaccine, but in so doing...
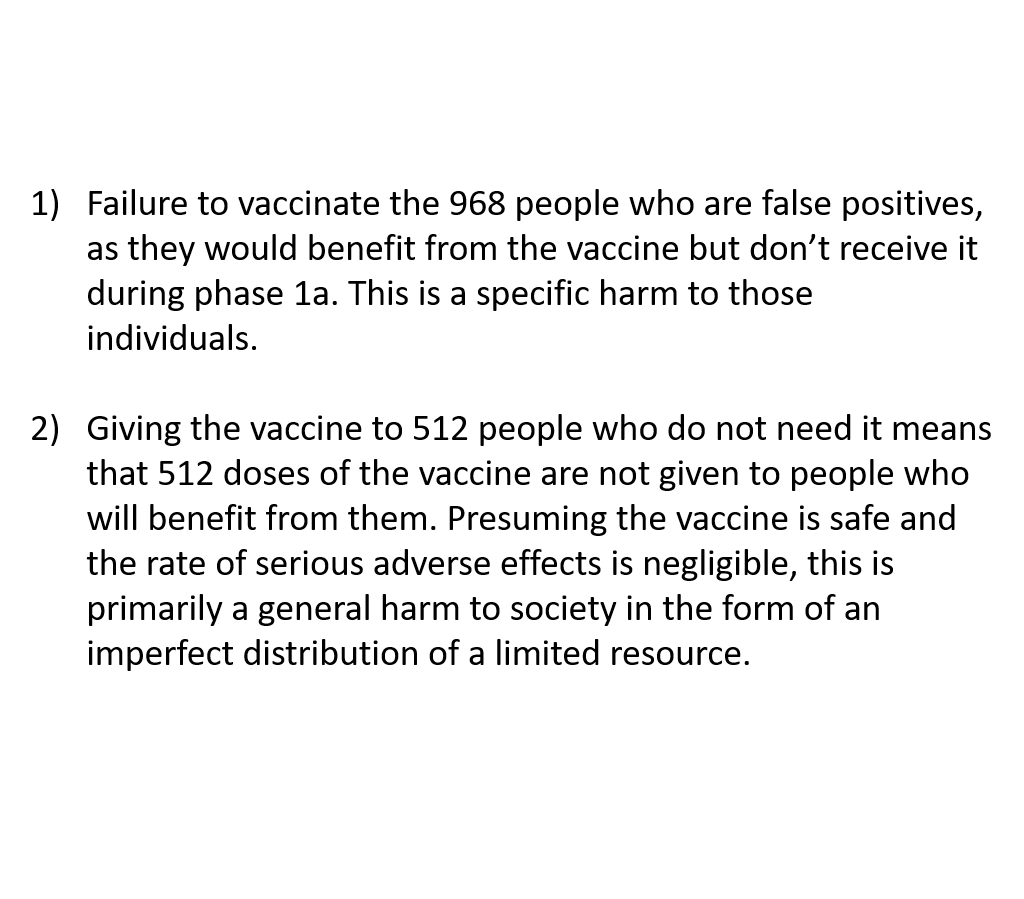
19/
...would have administered the vaccine to 512 individuals who DID NOT need one and failed to administer the vaccine to 968 individuals who DID need one.
Harm in this situation arises in two forms:
1) Harm to specific individuals
2) Harm to society in general
...would have administered the vaccine to 512 individuals who DID NOT need one and failed to administer the vaccine to 968 individuals who DID need one.
Harm in this situation arises in two forms:
1) Harm to specific individuals
2) Harm to society in general
20/
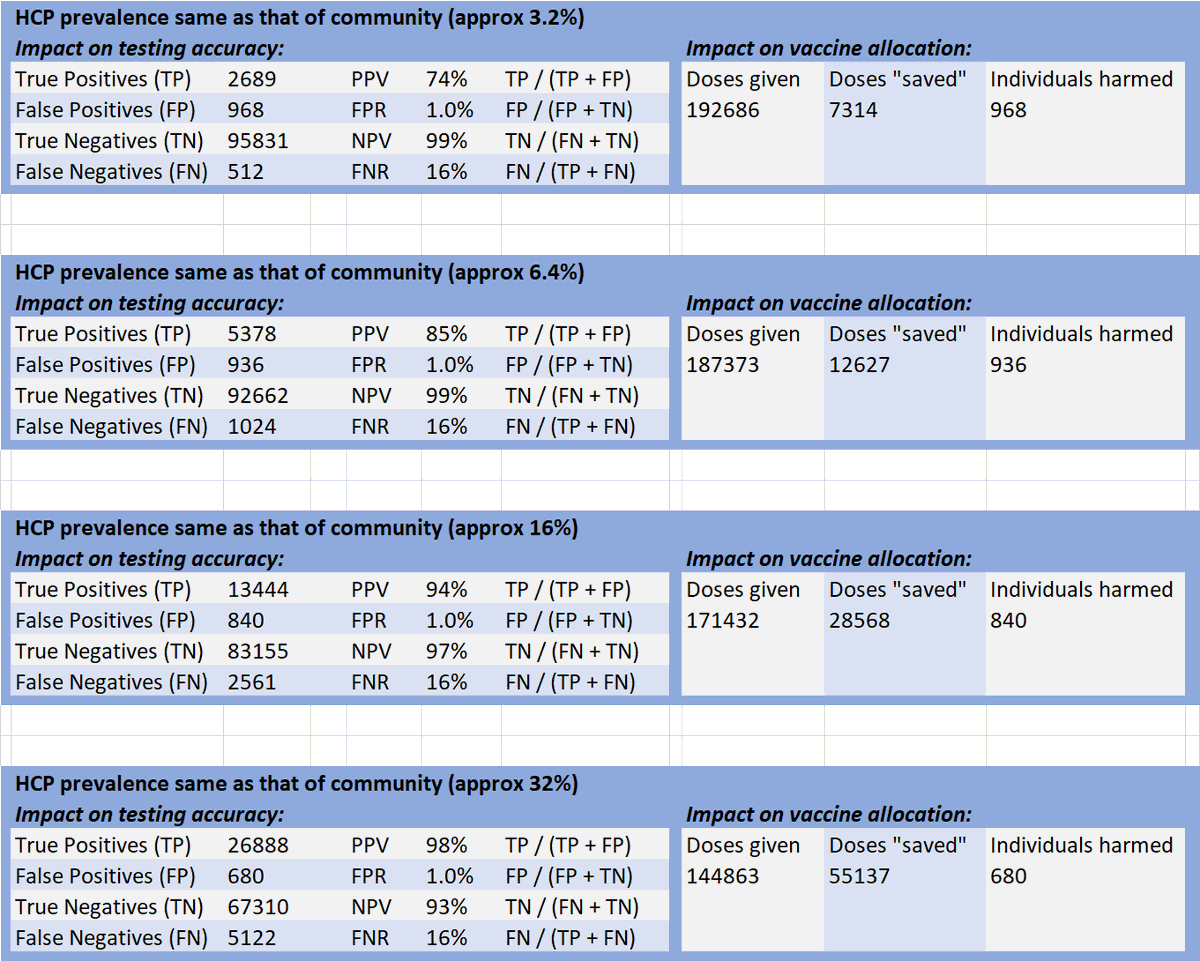
Now it’s critically important to revisit our assumption that the prevalence of prior SARS-CoV-2 infection in HCPs is the same as the community (i.e. only 3.3%).
Multiple studies have shown HCPs are infected at much higher rates than the community, but estimated rates vary.
Now it’s critically important to revisit our assumption that the prevalence of prior SARS-CoV-2 infection in HCPs is the same as the community (i.e. only 3.3%).
Multiple studies have shown HCPs are infected at much higher rates than the community, but estimated rates vary.

 Read on Twitter
Read on Twitter