Hi #econjobmarket, I am an applied microeconomist working on health economics. Here is an overview of my #JMP.
“Do subsidized nursing homes and home care teams reduce hospital bed-blocking? Evidence from Portugal”
Full version here:
https://anamoura.site/files/MouraJMP.pdf
 1/15
1/15
“Do subsidized nursing homes and home care teams reduce hospital bed-blocking? Evidence from Portugal”
Full version here:
https://anamoura.site/files/MouraJMP.pdf
 1/15
1/15
An importance source of inefficiency in healthcare is excessive length of stay at the hospital due to lack of alternative care arrangements following a hospitalization (aka bed-blocking)
2/n
2/n
Bed-blocking is associated with higher hospital costs, has potential detrimental impacts on patients' health & creates delays for elective care.
Despite growing concerns about bed-blocking across various countries, there is limited evidence on *how* to reduce bed-blocking
3/n
Despite growing concerns about bed-blocking across various countries, there is limited evidence on *how* to reduce bed-blocking
3/n
Research question:
I investigate whether, and to what extent, the availability of nursing homes (NH) and home care teams (HC) reduces hospital bed-blocking
4/n
I investigate whether, and to what extent, the availability of nursing homes (NH) and home care teams (HC) reduces hospital bed-blocking
4/n
Setting:
I focus in the Portuguese context my dataset contains the universe of inpatient hospital admissions at public hospitals in PT, for 2000-2015. Public hospitals have no financial motivation to prolong lengths of stay
my dataset contains the universe of inpatient hospital admissions at public hospitals in PT, for 2000-2015. Public hospitals have no financial motivation to prolong lengths of stay
5/n
I focus in the Portuguese context
 my dataset contains the universe of inpatient hospital admissions at public hospitals in PT, for 2000-2015. Public hospitals have no financial motivation to prolong lengths of stay
my dataset contains the universe of inpatient hospital admissions at public hospitals in PT, for 2000-2015. Public hospitals have no financial motivation to prolong lengths of stay 5/n
Empirics:
My identification strategy exploits 2 sources of variation.
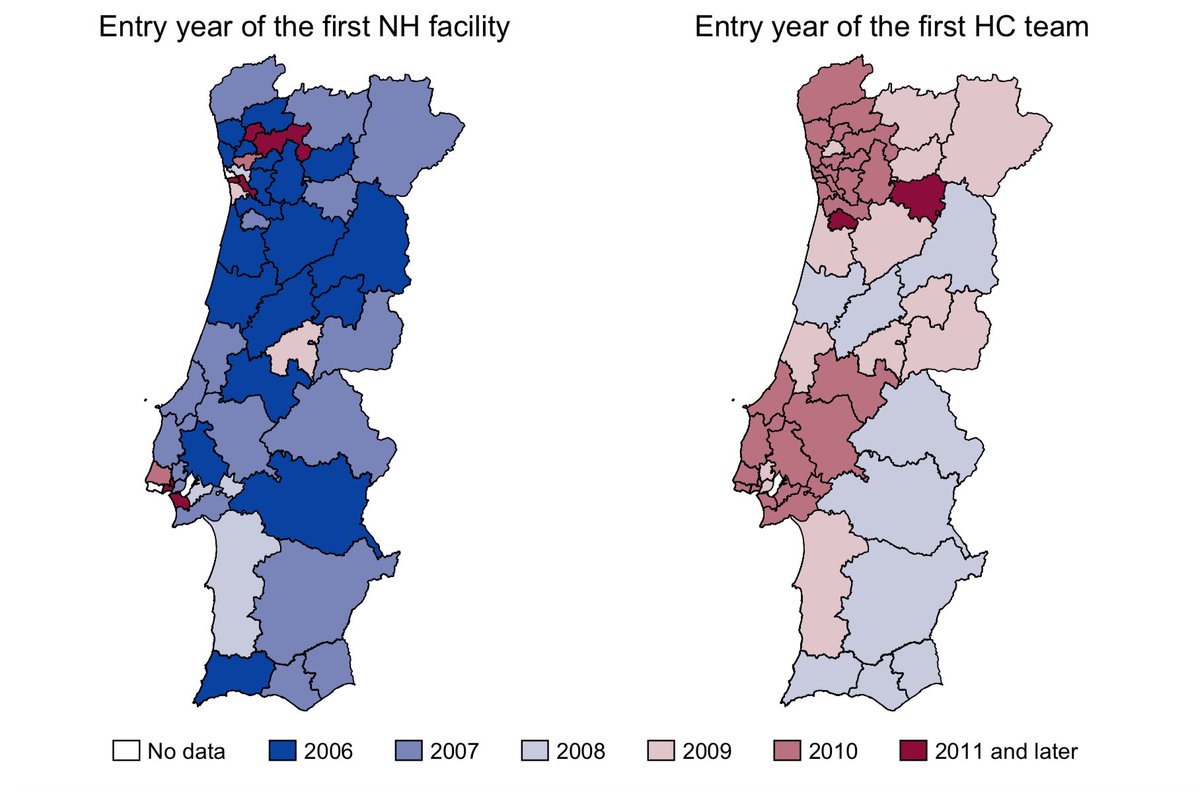
1st, variation across regions and time in the availability of NH and HC teams originating from the staggered introduction of a public policy reform
6/n
My identification strategy exploits 2 sources of variation.
1st, variation across regions and time in the availability of NH and HC teams originating from the staggered introduction of a public policy reform

6/n
2nd, variation between patients who live in the same region & are admitted to the hospital in the same time period but have ≠ propensities to bed-block
Potential bed-blockers exhibit social needs (no family support, inadequate housing) that might hinder timely discharge
7/n
Potential bed-blockers exhibit social needs (no family support, inadequate housing) that might hinder timely discharge
7/n
I compare the length of stay of potential bed-blockers and the length of stay of regular patients, before & after the entry of NH and HC teams in a region, where ≠ regions experienced NH and HC entry at ≠ points in time (triple-differences)
8/n
8/n
Findings:
1. Prior to NH and HC entry, potential bed-blockers stayed at the hospital substantially longer than regular patients (over 10 days longer)
2. NH and HC entry does not affect the length of stay of regular patients
9/n
1. Prior to NH and HC entry, potential bed-blockers stayed at the hospital substantially longer than regular patients (over 10 days longer)
2. NH and HC entry does not affect the length of stay of regular patients
9/n
3. HC entry reduces the length of stay of potential bed-blockers by 4 days
4. NH entry only reduces the length of stay of potential bed-blockers for those with high care needs (stroke, recovery from surgery). Most potential bed-blockers are not complex enough to need a NH
10/n
4. NH entry only reduces the length of stay of potential bed-blockers for those with high care needs (stroke, recovery from surgery). Most potential bed-blockers are not complex enough to need a NH
10/n
Can these reductions in length of stay harm patients? 
I find that reductions in length of stay for potential bed-blockers are not accompanied by reductions in the intensity of treatment received at the hospital, nor by an increased prob of readmissions
11/n

I find that reductions in length of stay for potential bed-blockers are not accompanied by reductions in the intensity of treatment received at the hospital, nor by an increased prob of readmissions
11/n
What happens to the beds freed up by reducing bed-blocking? 
They do not remain empty! I find that they are used to increase the number of elective admissions (pulling patients off waiting lists, thus reducing waiting times for elective care)
12/n

They do not remain empty! I find that they are used to increase the number of elective admissions (pulling patients off waiting lists, thus reducing waiting times for elective care)
12/n
How much does the healthcare system save? 
Not much... My conservative estimates suggest that HC teams generate a 26% reduction in the cost burden bed-blocking imposes on the healthcare system. But the overall amount is small bc bed-blocking is a relatively rare event
13/n

Not much... My conservative estimates suggest that HC teams generate a 26% reduction in the cost burden bed-blocking imposes on the healthcare system. But the overall amount is small bc bed-blocking is a relatively rare event
13/n
Policy implications:
HC and NH target ≠ patients
HC teams are more effective than NH are reducing bed-blocking bc most potential bed-blockers are not sick enough to need NH care
Small savings suggest that, during my study-period, allocation of resources was about right
14/n
HC and NH target ≠ patients
HC teams are more effective than NH are reducing bed-blocking bc most potential bed-blockers are not sick enough to need NH care
Small savings suggest that, during my study-period, allocation of resources was about right
14/n
If you read until here, thank you! 
Feel free to browse the full version of the paper for all the institutional details, robustness checks, and additional analyses: https://anamoura.site/files/MouraJMP.pdf
15/15

Feel free to browse the full version of the paper for all the institutional details, robustness checks, and additional analyses: https://anamoura.site/files/MouraJMP.pdf
15/15

 Read on Twitter
Read on Twitter