My last #tweetorial focused on the GCS. Now let's look at another hugely important clinical window into the brain: the pupil. What does a 'blown pupil' really imply? What about small fixed pupils? To understand this, we need to see how pupil size is governed. #FOAMed 1/20
The pupil has two functions, constriction and dilation, both under autonomic control. Sympathetics dilate the pupil and open the eyelid - easy to remember, because in 'fight or flight' mode, maximum information needs to get in to keep you alive. 2/20
By contrast, constriction is parasympathetic. Its main function is to regulate the amount of light on the retina, so in response to high light intensity (like a pen torch), both pupils constrict. 3/20
These parasympathetics have a straightforward course (literally). They hitchhike on the third nerve, which runs forward from the midbrain to the orbit to supply most of the extraocular muscles and eyelid. As they're superficial, they're vulnerable to extrinsic compression. 4/20
Plenty of things can compress the third nerve and produce mydriasis (a dilated pupil) - most classically a posterior communicating artery aneurysm. But in the context of an acutely comatose patient, it suggests something worrying: 'uncal herniation'. Why is this? 5/20
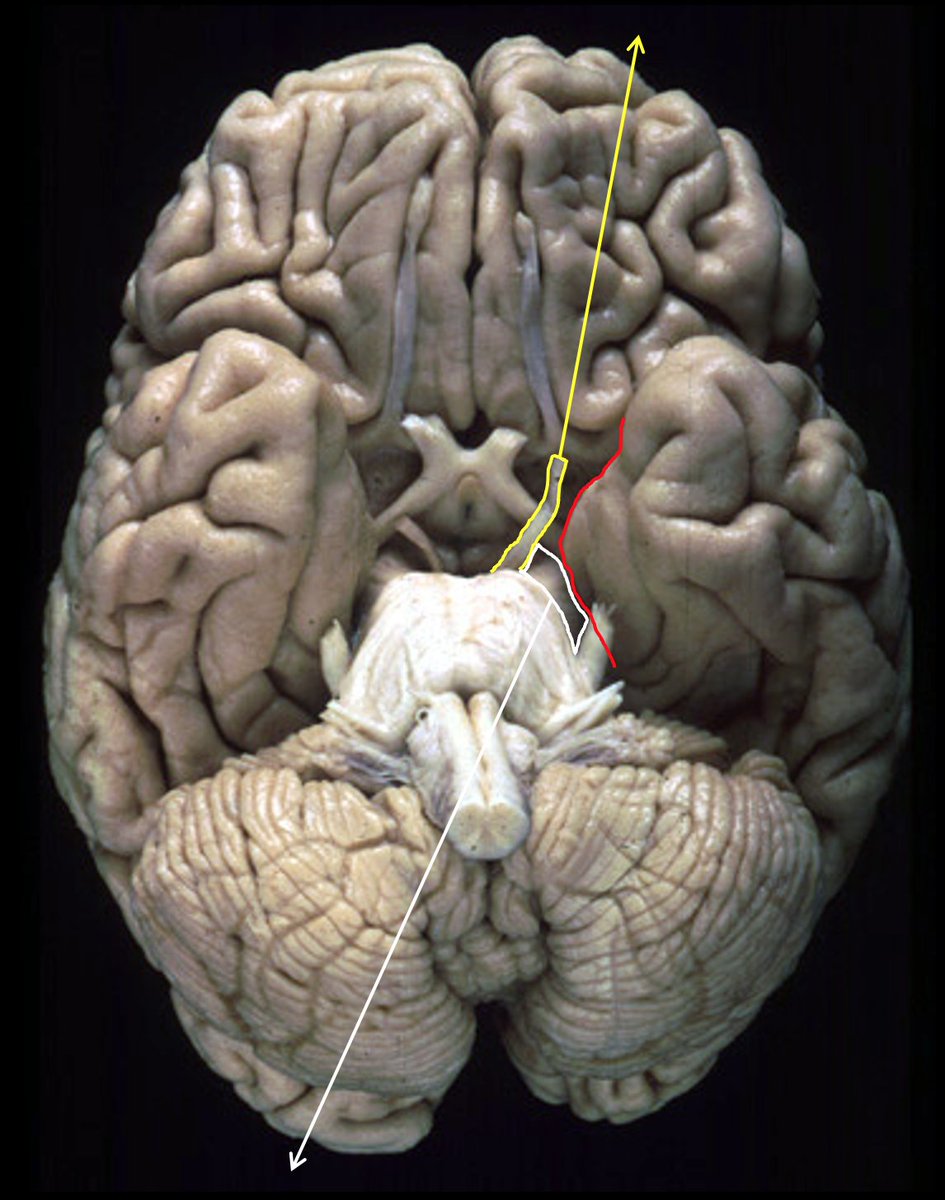
Here's the uncus (red). It's the lowest, most medial part of the temporal lobe, right on the skull base. See how close it is to the third nerve (yellow), and the cerebral peduncle (white, bringing the motor fibres down to the other side of the body) 6/20
When you have raised intracranial pressure, or an enlarging intracranial mass lesion like a haematoma over the hemisphere, you can see how the uncus might press down on these structures. The result - blown pupil, contralateral weakness and coma from brainstem compression. 7/20
So a blown pupil is a failure of parasympathetic pupilloconstriction allowing unchallenged sympathetic dilation. What about when sympathetic control of the pupil fails? This causes miosis, or a constricted pupil. 8/20
Horner's syndrome. "Miosis, ptosis, anhydrosis… Miosis, ptosis, anhydrosis"... The sympathetics have a frustratingly long course, but understanding it helps you get your head around the clinical picture and causes of a Horner's. 9/20
The pupillary sympathetics start in the hypothalamus, with input from the cerebral hemisphere. They descend in the cord, where they exit in the T1 root. They then ascend in the sympathetic chain, hitchhiking on the internal carotid back into the head again and to the pupil. 10/20
A lesion anywhere along this path affects the fibres to the pupil and the eyelid, so you ALWAYS get miosis and ptosis. But as sweat sympathetics to the upper forequarter of the body leave at various points, the degree of anhydrosis varies… 11/20
CNS problems like haemorrhage/trauma affecting the descending fibres in the brain/brainstem/cervical cord cause miosis, ptosis, and anhydrosis to the face, neck, arm and chest on that side.
The classical example is pontine haemorrhage - deep coma and pinpoint pupils. 12/20
The classical example is pontine haemorrhage - deep coma and pinpoint pupils. 12/20
If the problem is affecting the lower sympathetic chain, the fibres to the arm and chest have already left - there will be anhydrosis to the face only. The most worrying cause is a Pancoast tumour of the lung affecting the T1 root. 13/20
Moving further along the pathway, there are problems higher up like internal carotid dissections or skull base tumours. All the sweat sympathetics have branched off by now, so there is miosis and ptosis only! 14/20
For me, this structure serves mostly to think systematically about the causes of Horner's, what other features/symptoms to think about, and which investigations might be most appropriate. But if you really want to check for anhydrosis - try a spoon! 15/20 https://link.springer.com/article/10.1007/s10286-017-0401-2?shared-article-renderer
Anyway, importantly, third nerve palsy causes ptosis with dilated pupil; Horner's causes ptosis with constricted pupil. So the size of the pupil - or the laterality of the ptosis - becomes essential to knowing which pathology is at play. 16/20
Never forget that opiates cause small pupils, and pupils are physiologically small in old age, and in infancy. They should still be reactive, but in small pupils this is very hard to appreciate. 17/20
Finally, there are couple of locations where pathology can affect both parasympathetics and sympathetics together. One is the midbrain, where the third nerves come out anteriorly whilst the sympathetics descend towards T1. Compression here can cause a midsized, fixed pupil. 18/20
The other place is the cavernous sinus, where the third nerve parasympathetics and the internal carotid sympathetics happen to run together to the orbit. A midsized, fixed pupil in a swollen, painful eye with restricted movements can occur with cavernous sinus syndrome. 19/20
I hope this helps to demonstrate how much information you can get from examining the pupils. There are other pupillary disturbances - but at the very least, thinking about pupil size in this anatomical way can help to make a confusing area a little more structured. Thanks! 20/20

 Read on Twitter
Read on Twitter