It's #WAAW @ChelwestFT with @OllyTroise @mughal_nabeela @dr_luke_moore and team.
The WHY and the WHAT of AMS is easy! AMR bad & AMS good; Right drug, right time, right route etc.
The HOW is the hard part! We work in large complex systems dealing with heterogenous conditions
The WHY and the WHAT of AMS is easy! AMR bad & AMS good; Right drug, right time, right route etc.
The HOW is the hard part! We work in large complex systems dealing with heterogenous conditions
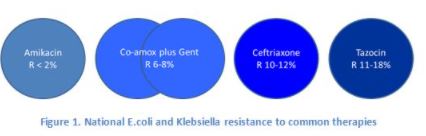
HOW you enable AMS in practice is hugely challenging. Translating complex microbiological concepts into easy-to-interpet guidelines is not easy. Our clinicians have complex decisions to make within tight deadlines (1 'golden' hour) so we must make it as easy as possible for them
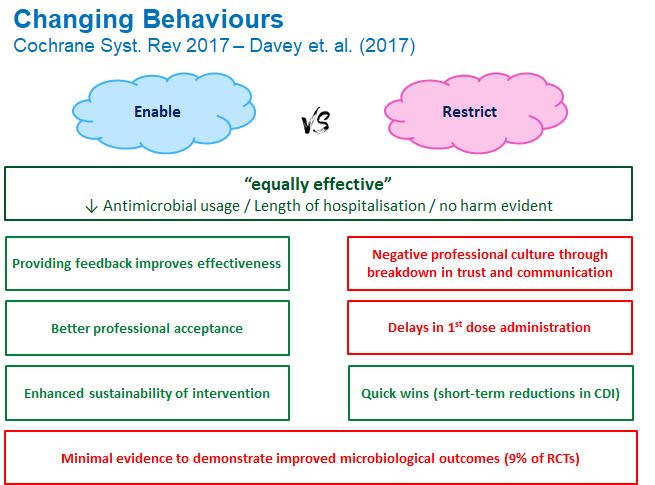
@ChelwestFT we adopt the 'enablement' AMS strategy. We don't restrict any ABX (its ward stock) but we have a tight feedback loop on prescribing. **All** ABX prescribed is reviewed daily by team AMS (300 pt/day) and any "off-piste" prescribing is discussed with the clinical team.
This feedback loop (hours rather than months as seen with an audit) helps change behaviours! We do ward rounds across all specialities each day and consult on complex ID/Micro patients. Here we aim to 'assist' with diagnosis, de-escalation (or escalation) and optimise current Rx
Our job is to make it easier to prescribe the right ABX:
-Make guidelines simple, clear and accessible
-Provide options for escalation & de-escalation in guidance
-Take the stress out of dosing (add to guidance)
-Avoid complex regimens where possible (AZI > CLARI, LINEZ >VANC)
-Make guidelines simple, clear and accessible
-Provide options for escalation & de-escalation in guidance
-Take the stress out of dosing (add to guidance)
-Avoid complex regimens where possible (AZI > CLARI, LINEZ >VANC)

 Read on Twitter
Read on Twitter