Were you one of the many hepatologists or txp surgeons who wondered if you should start UDCA in a transplanted patient with PBC? Well, rest assured my friend and read on.
https://aasldpubs.onlinelibrary.wiley.com/doi/abs/10.1002/lt.25935#.X7PqZWhGT8w.twitter
https://aasldpubs.onlinelibrary.wiley.com/doi/abs/10.1002/lt.25935#.X7PqZWhGT8w.twitter
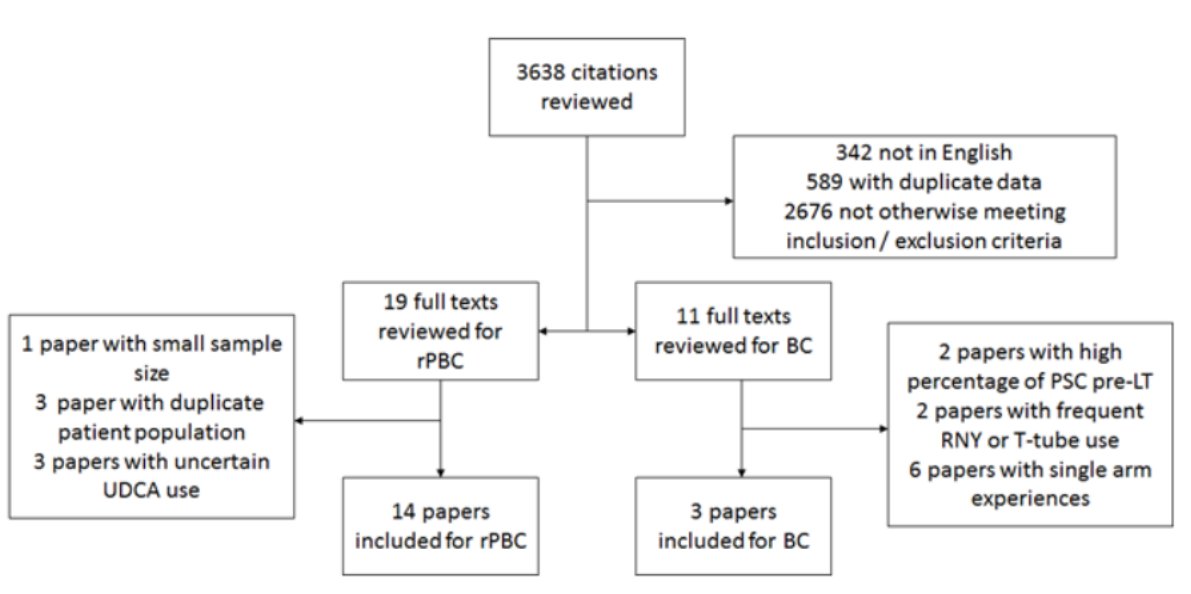
UDCA Decreases Incidence of Primary Biliary Cholangitis and Biliary Complications after Liver Transplant: A Meta-Analysis - by Pedersen et al from @UTSWNews.
 15 studies
15 studies
 530 pts for biliary complications
530 pts for biliary complications
 1,727 for recurrent PBC
1,727 for recurrent PBC
 15 studies
15 studies 530 pts for biliary complications
530 pts for biliary complications 1,727 for recurrent PBC
1,727 for recurrent PBC
 UDCA
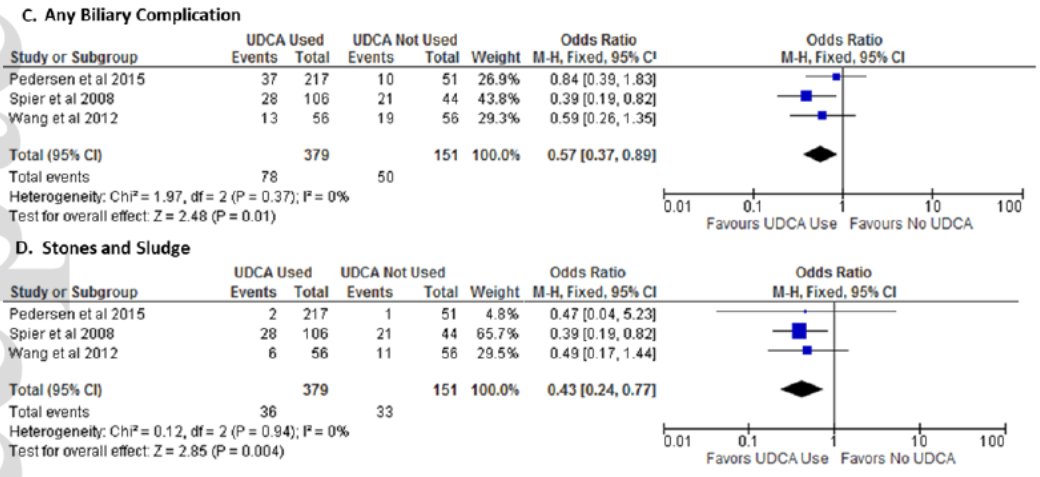
UDCA biliary complications (OR 0.70), stones and sludge (OR 0.49), but not biliary stricture
biliary complications (OR 0.70), stones and sludge (OR 0.49), but not biliary stricture UDCA
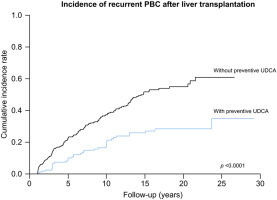
UDCA rate of recurrent PBC (13% vs. 34%)
rate of recurrent PBC (13% vs. 34%)
This is incredibly important work that echoes the findings recently published by Corpechot and Global PBC Study Group in @JHepatology showing preventive UDCA post-LT reduces recurrent disease.
https://www.journal-of-hepatology.eu/article/S0168-8278(20)30205-1/abstract#.X7Ps-ZiIg6k.twitter
https://www.journal-of-hepatology.eu/article/S0168-8278(20)30205-1/abstract#.X7Ps-ZiIg6k.twitter
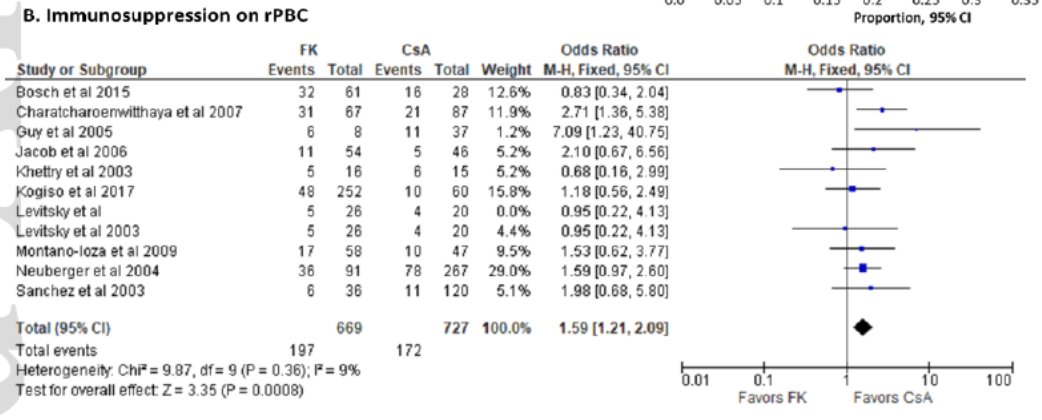
You just performed an uncomplicated transplant on a patient with decompensated PBC. Which calcineurin inhibitor do you choose for immunosuppression? @DrLiver @drbobbybrown @VatcheAgopianMD @elizabeth_verna @LizzieAbyMD @The__Liver @serperm @DebbieShawcros1

 Read on Twitter
Read on Twitter