Our appraisal of the effects of apoB on diseases in 1st degree relatives and the lifespan picked up some interesting findings https://twitter.com/medrxivpreprint/status/1327022812406616064
This builds on our previous study https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003062 which includes a description of the derivation of the genetic instruments and their relationships with risk of CHD employing multivariable Mendelian randomization
First, a brief summary of methods: we used endpoints reported as occurring in 1st degree relatives in UK biobank as the primary outcomes. We constructed genetic instruments for apoB, LDL-C and TG and implemented them in uni- and multivariable MR
Use of outcomes reported as occurring in 1st degree relatives in MR is accompanied by a few nuances – which we highlight in the Intro and Discussion. E.g. magnitudes of effect will be expected to be an underestimate due to a form of regression dilution bias.
We sought replication using conventional 2-sample MR with data for large-scale GWAS of T2D from DIAMANTE and survival using a GWAS of those surviving to an age corresponding to the 90th centile of longevity
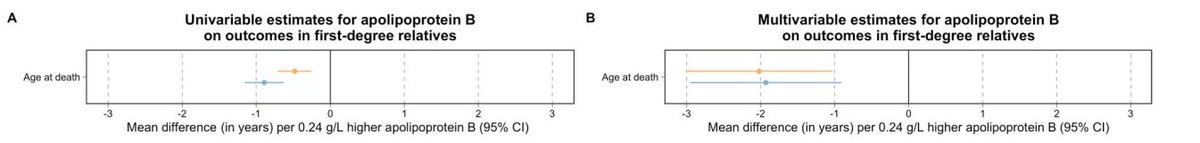
Higher genetically-instrumented apoB shortened the lifespan by 6-10 months in parents (per 0.24 g/L higher apoB) but in multivariable MR, the magnitude strengthened to ~ 2 years.
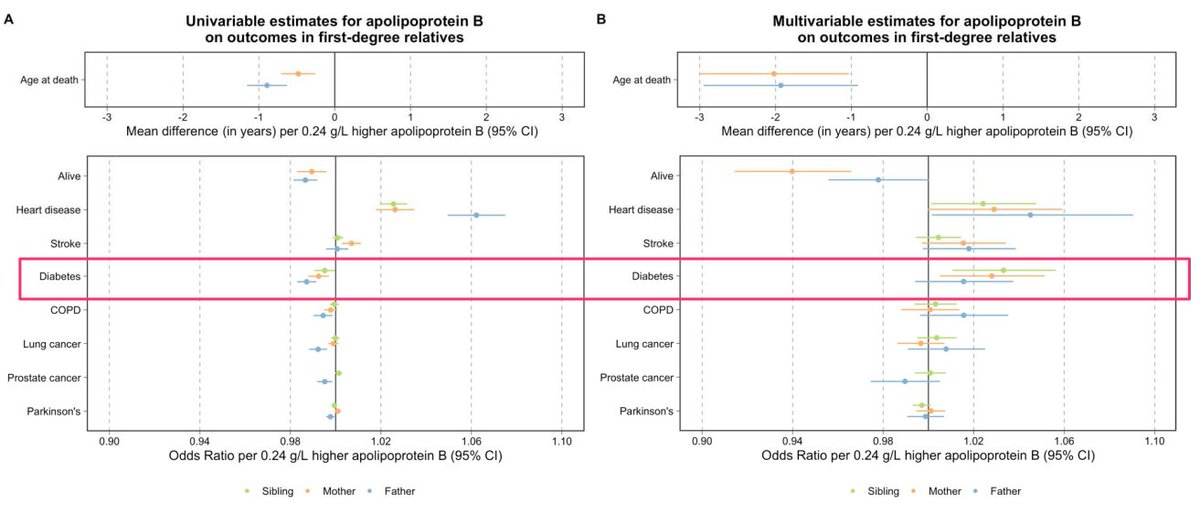
In the plot below, orange = estimates for mothers, blue = estimates for fathers
In the plot below, orange = estimates for mothers, blue = estimates for fathers
This was replicated using conventional 2-sample MR where the outcome was surviving to an age corresponding to the 90th centile of longevity: very strong effects of apoB were found (1-SD higher apoB, ~60% lower relative odds of surviving to 90th centile of longevity).
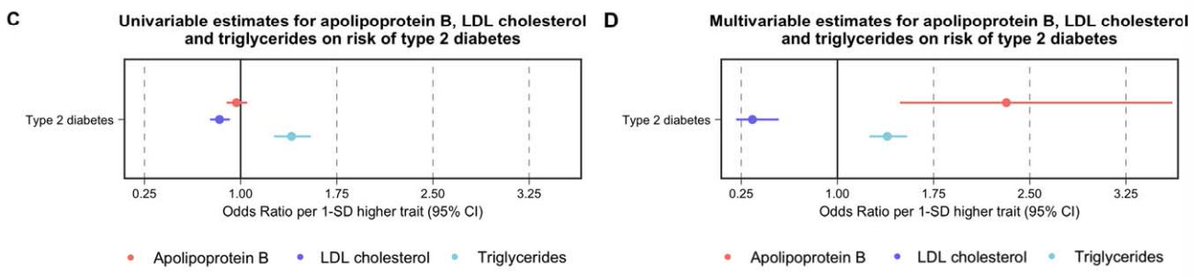
We found a peculiar relationship with type 2 diabetes: on univariable appraisal, inverse effects of apoB were identified. But in multivariable analysis, higher apoB caused a higher risk of T2D.
This was replicated in conventional 2-sample MR using DIAMANTE, where pronounced effects were identified.
Fascinatingly, the effects of apoB on T2D were directionally opposite to LDL-C in multivariable MR:
Higher apoB -> higher risk of T2D
Higher LDL-C -> lower risk of T2D
Fascinatingly, the effects of apoB on T2D were directionally opposite to LDL-C in multivariable MR:
Higher apoB -> higher risk of T2D
Higher LDL-C -> lower risk of T2D
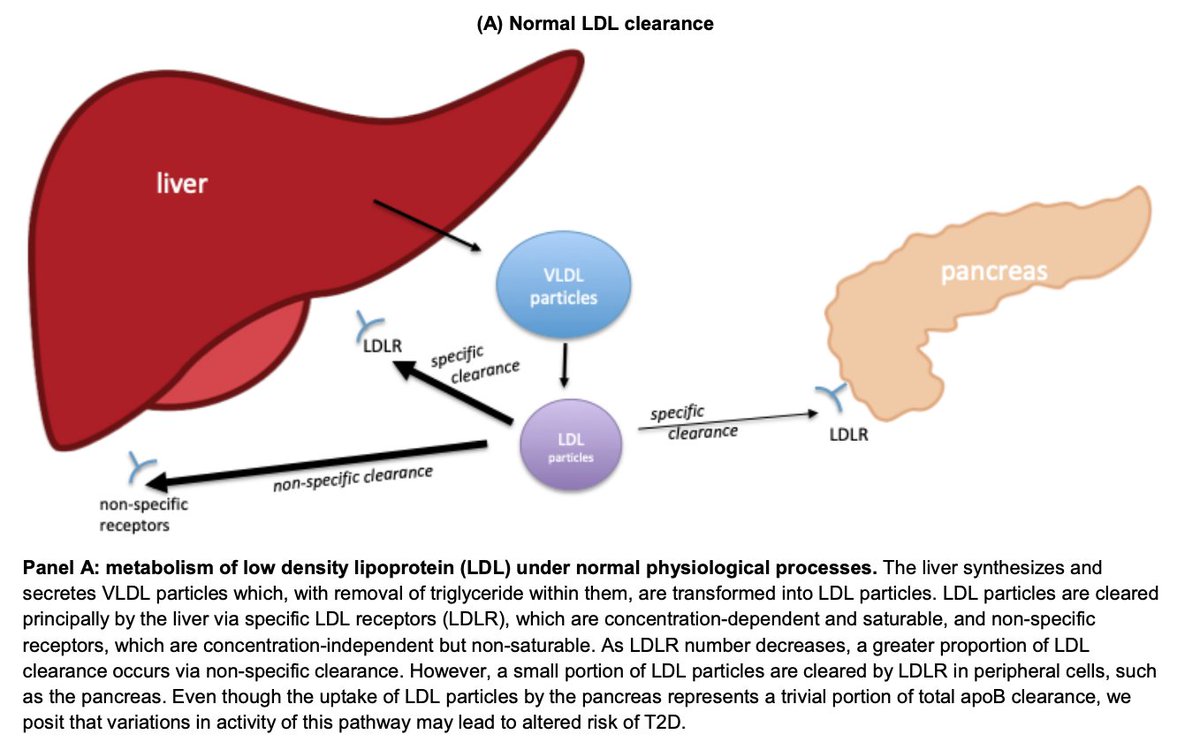
How do we explain this quandary? One potential way to reconcile these findings is to think about how LDL is metabolised.
 to Prof Allan Sniderman for the unique biological insights
to Prof Allan Sniderman for the unique biological insights
 to Prof Allan Sniderman for the unique biological insights
to Prof Allan Sniderman for the unique biological insights
Under normal conditions, LDL clearance occurs through specific and non-specific pathways, which can include clearance through peripheral tissue such as the pancreas.
In our MVMR analysis of LDL-C (where apoB is kept constant), this might approximate decreased clearance of LDL through specific pathways. Here, pancreatic-mediated clearance of LDL through specific pathways is also reduced meaning less pancreatic uptake of LDL & lower risk of T2D
In our MVMR analysis of apoB (where LDL-C is kept constant), this might approximate over-production of VLDL particles, leading to higher LDL clearance by specific and non-specific pathways. Higher pancreatic clearance leads to higher risk of T2D.
Certainly, this is a hypothesis that needs further investigation, but potentially, has important translational relevance: if we can increase LDL-C clearance through the liver and lower clearance of LDL through the pancreas, we can potentially lower risks of both CHD and T2D
Our study highlights the major relevance of apoB in causing multiple diseases and shortening the lifespan.
The effects on the lifespan are almost certainly a consequence of apoB causing CHD, stroke and T2D: the leading causes of death https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
The effects on the lifespan are almost certainly a consequence of apoB causing CHD, stroke and T2D: the leading causes of death https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
Major thanks to colleagues - this paper demonstrates what can be achieved through multidisciplinary scientific collaborations
@iTomRichardson @QinFinn @ECSanderson @anubha_M_Oxf @markmccarthyoxf @timfrayling @mak_sysepi Allan Sniderman @mendel_random
@iTomRichardson @QinFinn @ECSanderson @anubha_M_Oxf @markmccarthyoxf @timfrayling @mak_sysepi Allan Sniderman @mendel_random

 Read on Twitter
Read on Twitter